Hypothermia can be defined as a drop in the core body temperature below 35°C (95°F) and is classified into mild, moderate, severe, and profound forms based on the degree of temperature decrease. Certain populations may be more vulnerable to accidental hypothermia, including extremes of age, homeless, individuals with mental illness, and alcohol and drug abusers. Evaluation should include assessment for associated trauma and contributing medical conditions. Management involves rewarming the patient by different methods based on the severity of the hypothermia.
Last updated: Apr 14, 2025
Hypothermia is a decrease in core body temperature Body Temperature The measure of the level of heat of a human or animal. Heatstroke to below 35°C (95°F).

Accidental hypothermia results from exposure to cold temperatures.
Image: “Skiing uphill” by Free-Photos. License: Pixabay License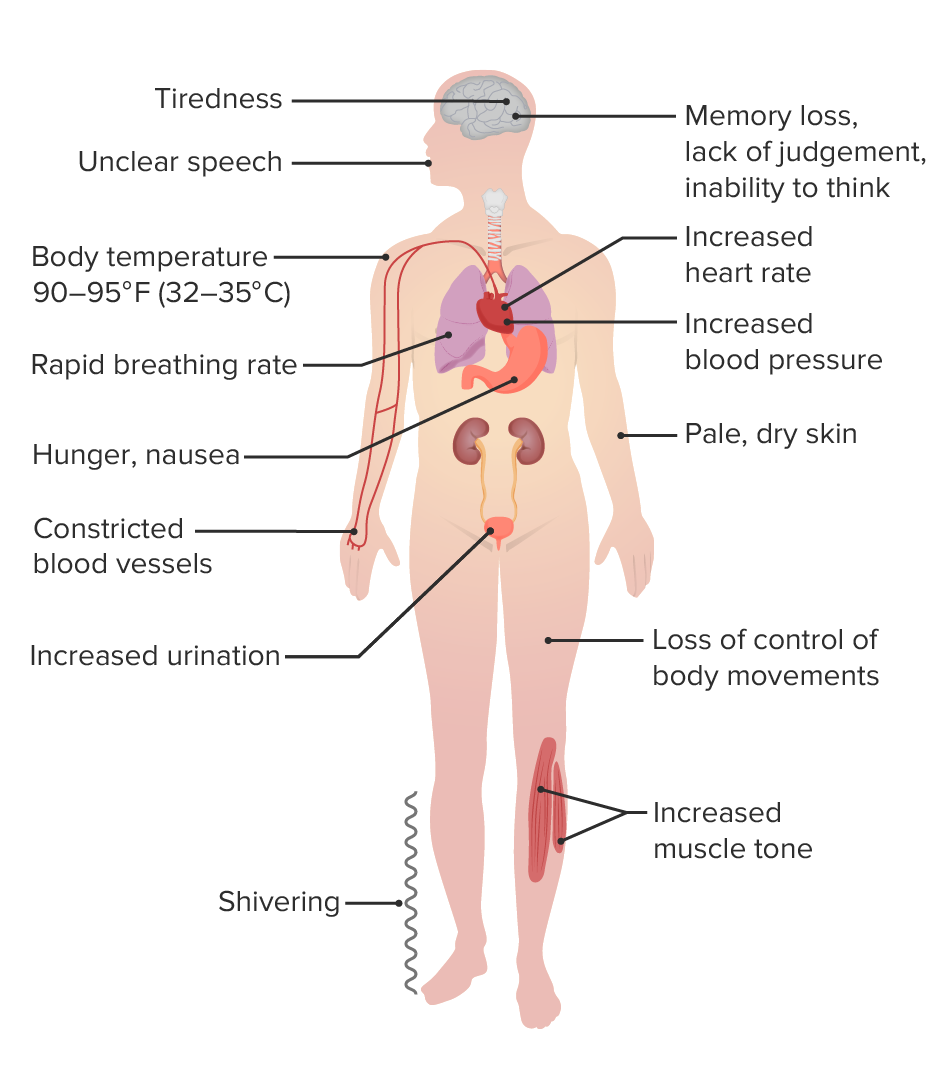
Clinical presentation of mild hypothermia
Image by Lecturio.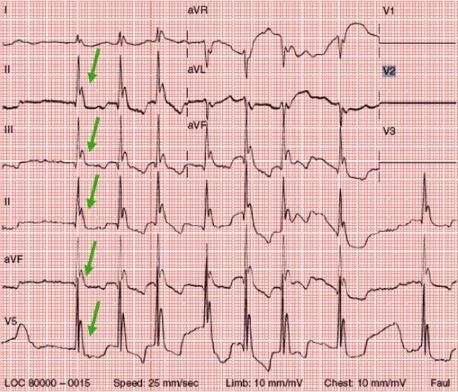
Osborn waves (J point elevation) associated with hypothermia
Image: “Osborn waves” by the First Department of Internal Medicine, Nippon Medical School, Tokyo, Japan. License: CC BY 2.5, edited by Lecturio.