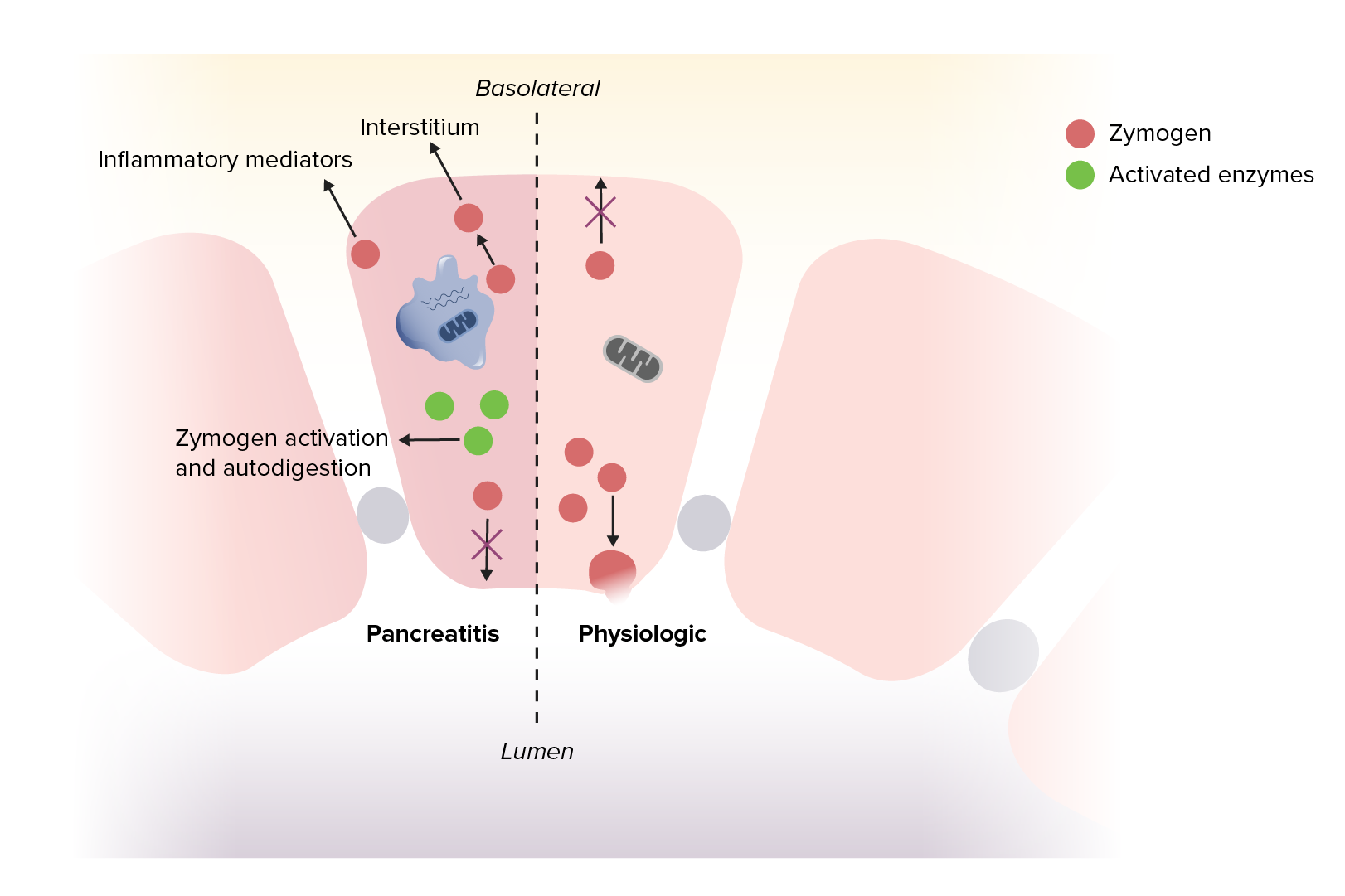
Acute pancreatitis is an inflammatory disease of the pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy due to autodigestion. Common etiologies include gallstones Gallstones Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis and excessive alcohol use. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with epigastric pain Epigastric pain Mallory-Weiss Syndrome (Mallory-Weiss Tear) radiating to the back. Diagnosis requires 2 of 3 criteria, including: characteristic abdominal pain Abdominal Pain Acute Abdomen, serum amylase Amylase A group of amylolytic enzymes that cleave starch, glycogen, and related alpha-1, 4-glucans. Digestion and Absorption and lipase Lipase An enzyme of the hydrolase class that catalyzes the reaction of triacylglycerol and water to yield diacylglycerol and a fatty acid anion. It is produced by glands on the tongue and by the pancreas and initiates the digestion of dietary fats. Malabsorption and Maldigestion 3 times the upper limit Limit A value (e.g., pressure or time) that should not be exceeded and which is specified by the operator to protect the lung Invasive Mechanical Ventilation of normal, or characteristic radiology findings. Ranson’s criteria is commonly used to assess the severity. Management includes aggressive intravenous (IV) hydration, analgesia Analgesia Methods of pain relief that may be used with or in place of analgesics. Anesthesiology: History and Basic Concepts, nutritional support, and treatment of the underlying cause.
Last updated: May 12, 2025
Acute pancreatitis
Image by Lecturio.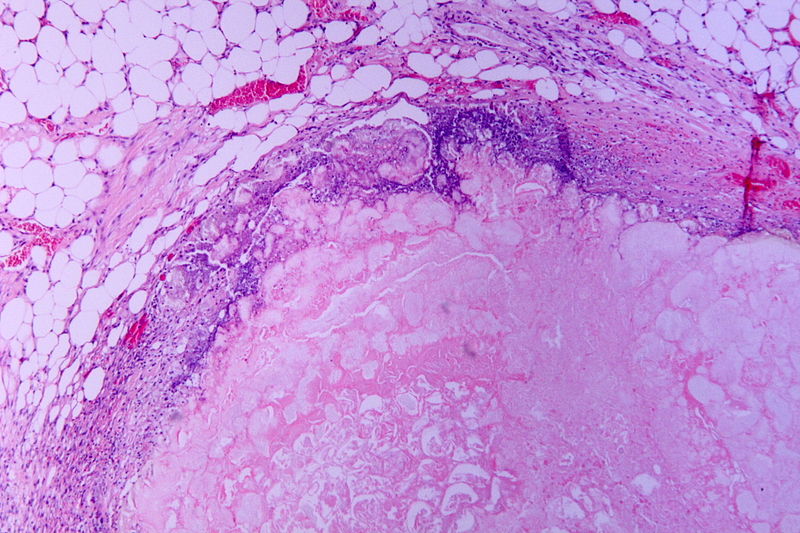
Hematoxylin and eosin (H&E) stain of necrotic pancreatitis (eosinophilic area without architecture: necrosis), surrounded by basophilic inflammatory cells and normal fat cells
Image: “Tryptic fat tissue necrosis in severe pancreatitis” by Patho. License: CC BY-SA 3.0.
Cullen’s sign, signaling blood in the peritoneum
Image: “Cullen’s sign” by Herbert L. Fred, MD. License: CC BY 2.0.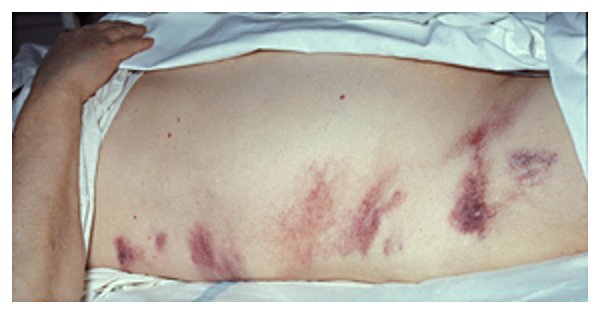
Grey-Turner’s sign due to hemorrhagic pancreatitis
Image: by Herbert L. Fred, MD and Hendrik A. van Dijk. License: CC BY 2.0.The diagnosis of acute pancreatitis requires at least 2 of the following:
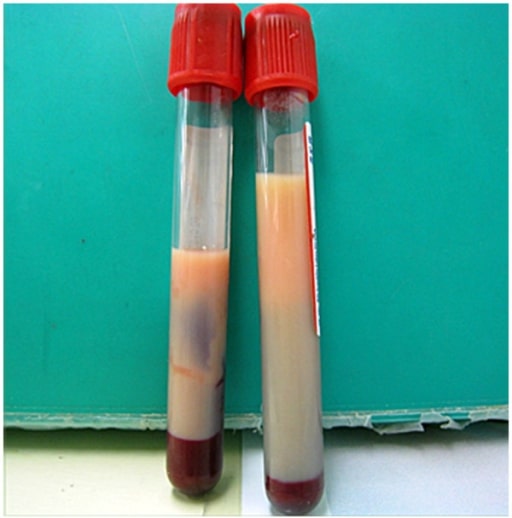
Milky plasma seen in a patient with hypertriglyceridemia: If seen, milky plasma should be considered as a potential cause of acute pancreatitis.
Image: “Milky plasma” by the Department of Emergency and Critical Care Medicine, Ohta Nishinouchi Hospital, 2-5-20 Nishinouchi, Koriyama, Fukushima, 963-8558, Japan. License: CC BY 2.0.Imaging may not be required if the 1st 2 diagnostic criteria are met MET Preoperative Care, but can be used for evaluating the underlying cause and complications:
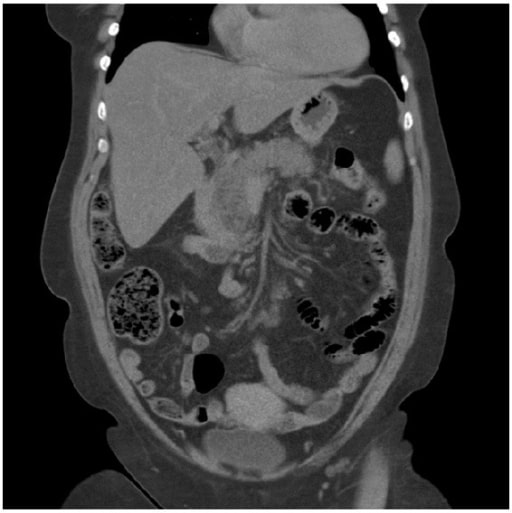
Acute pancreatitis: A CT scan showing pancreatitis changes, which appears enlarged and edematous.
Image: “A computed tomography scan” by Department of Surgery, Helsingborg Hospital, 25187 Helsingborg, Sweden. License: CC BY 3.0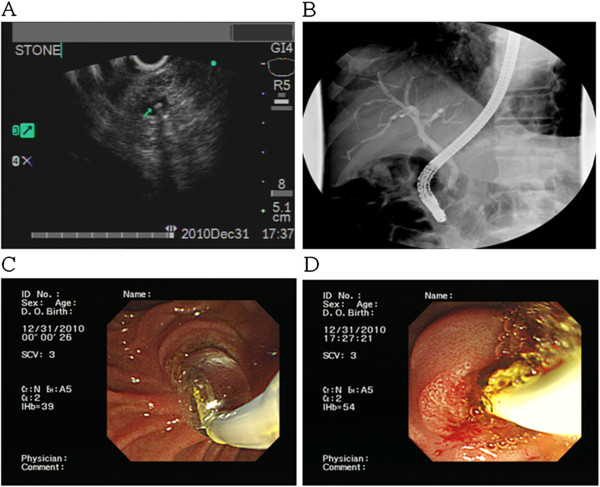
A tiny CBD stone is revealed using US. Such stones should be considered a potential etiology in a patient presenting with acute pancreatitis.
Image: “F2” by the Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Veterans General Hospital, 386 Ta-Chung 1st Road, Kaohsiung 81362, Taiwan. License: CC BY 2.0, edited by Lecturio.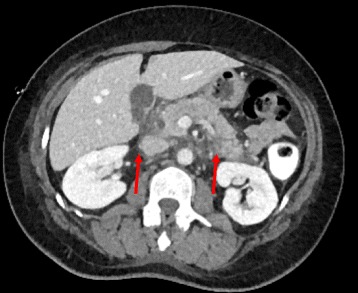
Acute pancreatitis on CT scan, showing edema around the pancreas
Image: “Arterial phase contrast CT showing an acute pancreatitis” by Benoît Bédat et al. License: CC BY 4.0.Identifying the severity of acute pancreatitis is helpful in order to ensure the patient is treated appropriately:
| Present on admission | At 48 hours after admission |
|---|---|
| Age > 55 years | Decrease in hematocrit Hematocrit The volume of packed red blood cells in a blood specimen. The volume is measured by centrifugation in a tube with graduated markings, or with automated blood cell counters. It is an indicator of erythrocyte status in disease. For example, anemia shows a low value; polycythemia, a high value. Neonatal Polycythemia > 10% |
| WBC > 16,000/μL | Increase in BUN by ≥ 5 mg/dL |
| Blood glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance > 200 mg/dL | Serum Ca CA Condylomata acuminata are a clinical manifestation of genital HPV infection. Condylomata acuminata are described as raised, pearly, flesh-colored, papular, cauliflower-like lesions seen in the anogenital region that may cause itching, pain, or bleeding. Condylomata Acuminata (Genital Warts) < 8 mg/dL |
| Serum LDH LDH Osteosarcoma > 350 IU/L | PaO2 < 60 mm Hg |
| Aspartate Aspartate One of the non-essential amino acids commonly occurring in the l-form. It is found in animals and plants, especially in sugar cane and sugar beets. It may be a neurotransmitter. Synthesis of Nonessential Amino Acids transaminase Transaminase A subclass of enzymes of the transferase class that catalyze the transfer of an amino group from a donor (generally an amino acid) to an acceptor (generally a 2-keto acid). Most of these enzymes are pyridoxyl phosphate proteins. Catabolism of Amino Acids ( AST AST Enzymes of the transferase class that catalyze the conversion of l-aspartate and 2-ketoglutarate to oxaloacetate and l-glutamate. Liver Function Tests) > 250 IU/L | Base deficit > 4 mEq/L |
| Estimated fluid sequestration > 6 L |
| BUN | > 25 mg/dL |
|---|---|
| Impaired mental status | GCS GCS A scale that assesses the response to stimuli in patients with craniocerebral injuries. The parameters are eye opening, motor response, and verbal response. Coma < 15 |
| Systemic inflammatory response syndrome Systemic Inflammatory Response Syndrome Sepsis in Children (SIRS) | Evidence of SIRS |
| Age | > 60 years |
| Pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion | Positive finding on imaging |
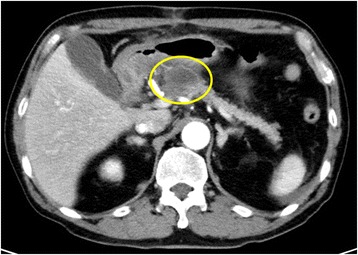
Abdominal CT scan showing the initial area of patchy necrosis around the head of the pancreas
Image: “Abdominal CT scan” by Francesco Fontana. License: CC BY 4.0.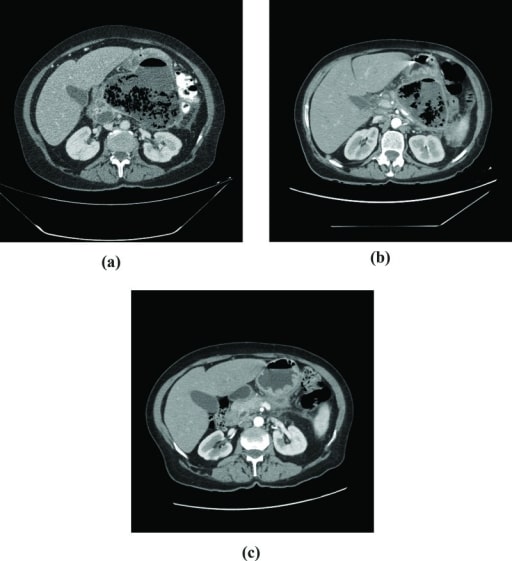
CT scans in a patient who developed infected pancreatic necrosis:
A: Extensive pancreatic necrosis with a large amount of gas is seen in the body and tail of the pancreas.
B: After 60 days of follow-up, a small decrease in the collection of gas is noted.
C: 4 months after hospital discharge: atrophy of pancreatic parenchyma
Acute pancreatitis repeatedly occurred 1 month after the 1st operation, and a pancreatic pseudocyst developed at the same site. Enhanced CT showed a cyst with a diameter of 29 mm in the body of the pancreas.
Image: “Pancreatic pseudocyst” by the Department of Gastroenterological Surgery, Kumamoto University Graduate School of Medical Sciences, 1-1-1 Honjo, Kumamoto, 860-8556 Japan. License: CC BY 4.0.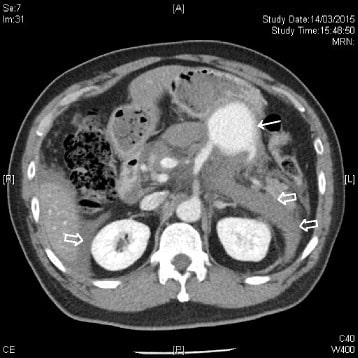
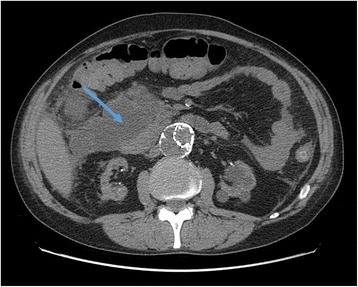
CT scan of the abdomen with IV contrast showing a contrast-enhanced mass (solid arrow) at the splenic artery (branching from the superior mesenteric artery) compatible with a splenic artery pseudoaneurysm. Hemoretroperitoneum and hemoperitoneum were demonstrated (hollow arrows).
Image: “CT scan of the abdomen” by the Accident and Emergency Department, Ruttonjee Hospital, Wanchai, Hong Kong. License: CC BY 4.0.
Contrast-enhanced CT scan of the abdomen reveals a 5 × 6 × 7 cm complex cystic mass in the region of the uncinate process of the pancreatic head with an enhancing capsule and a small hyperdensity consistent with pseudoaneurysm of a peripancreatic vessel with active bleeding into the pancreatic pseudocyst.
Image: “Contrast-enhanced CT scan” by Rohan Mandaliya. License: CC BY 2.0.