Thromboangiitis obliterans (TAO), also known as Buerger disease, is a rare condition causing inflammatory thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus of the small- to medium-sized arteries Medium-Sized Arteries Kawasaki Disease and veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology of the upper and lower extremities. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are typically young smokers presenting with distal extremity ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, ulcers, or gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction. Superficial thrombophlebitis and Raynaud phenomenon can be early manifestations. Diagnosis is based on clinical findings, vascular testing, and angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery. Other potential diagnoses must be ruled out. The use of tobacco products is strongly associated with the disease; therefore, smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases cessation is an essential part of management and decreases the risk of amputation Amputation An amputation is the separation of a portion of the limb or the entire limb from the body, along with the bone. Amputations are generally indicated for conditions that compromise the viability of the limb or promote the spread of a local process that could manifest systemically. Amputation.
Last updated: Mar 25, 2025
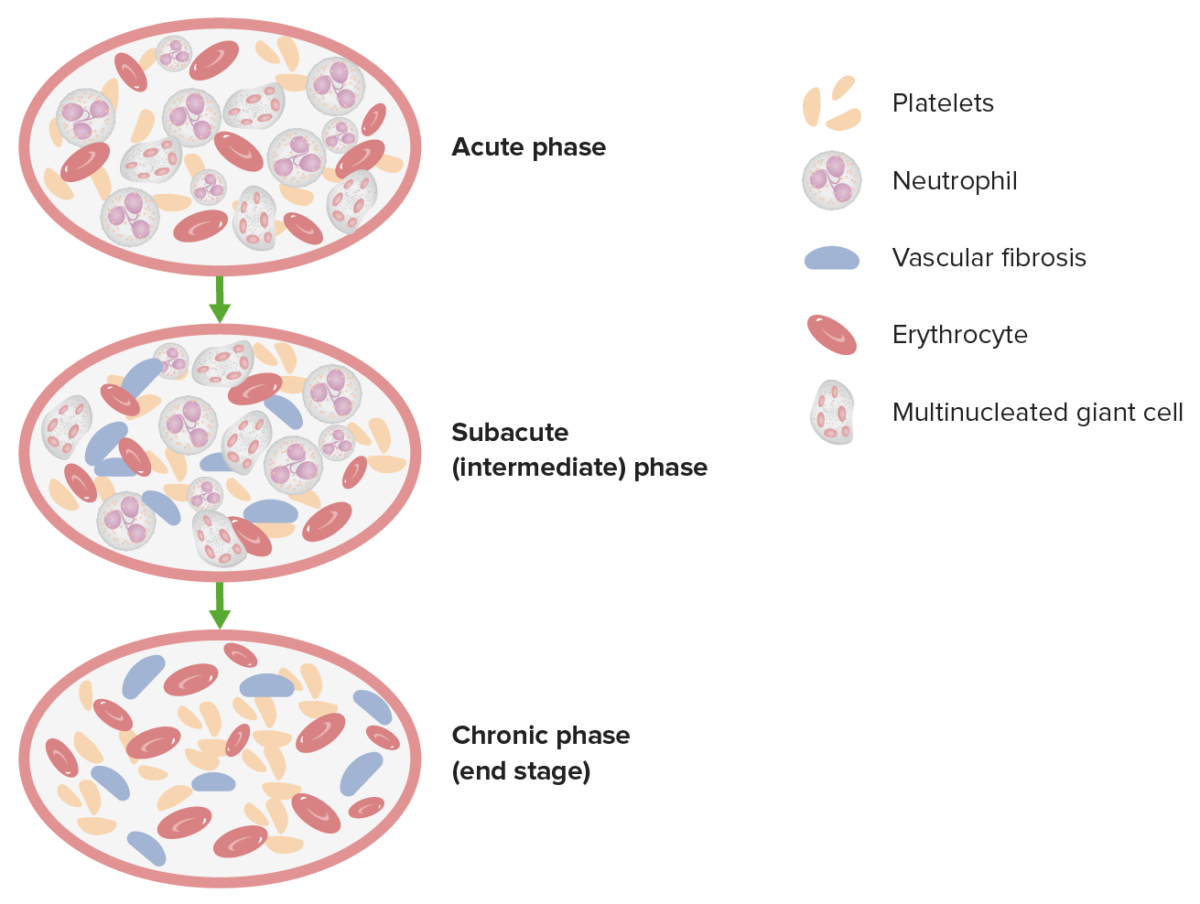
This image demonstrates the 3 pathologic phases in TAO.
Image by Lecturio.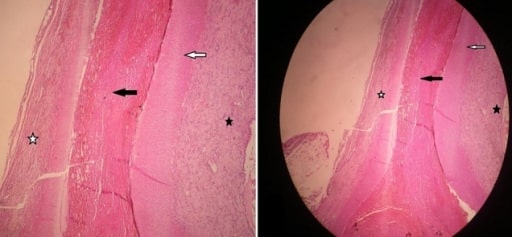
Histopathological specimen obtained from a patient with thromboangiitis obliterans . The vessel lumen has a thrombus rich in neutrophils (black star). Both the tunica intima and media are normal (white and black arrows). Periarterial lymphocytic infiltrate is seen (white star).
Image: “[Severe mesenteric infarction by superior mesenteric artery occlusion in a patient suffering from Buerger disease].” by Ratbi MI, Abissegue GY, Tarchouli M, Tajedine MT. License: CC BY 2.0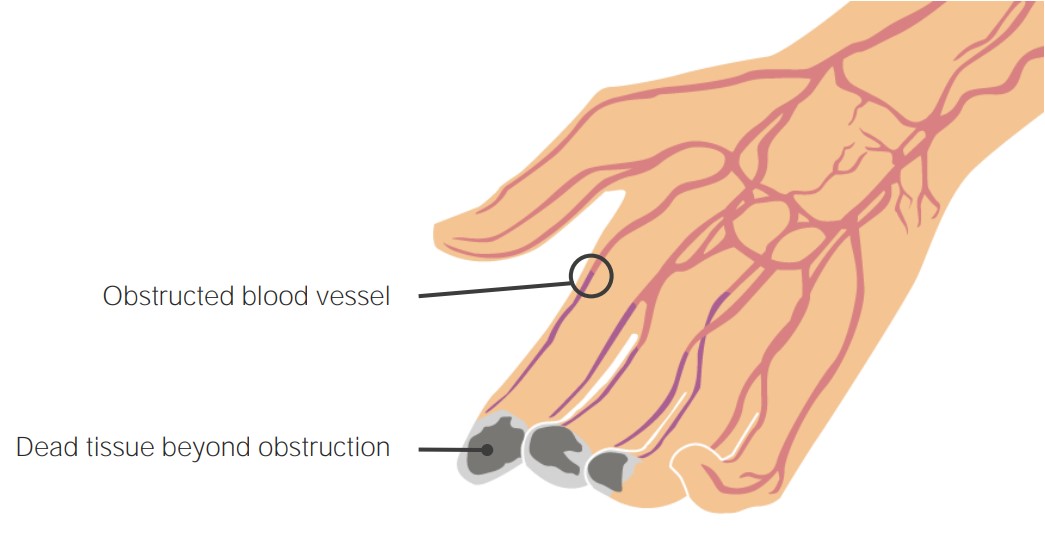
The inflammatory thrombus occluding arteries and veins of the distal extremities leads to diminished blood supply, causing damage and tissue death distally.
Image by Lecturio.
Superficial thrombophlebitis of the right leg. Notice the arrow pointing at a darkened cord-like structure that is following venous distribution. The cord-like structures are tender and can be the initial presentation of TAO.
Image: “Ischemic toes after venous thromboembolism: a difficult differential diagnosis with good response to combination therapy-a case report” by Owlia MB, Salimzadeh A, Alishiri G, Kargar S. License: CC BY 3.0.
Ischemic ulceration and necrosis of the middle finger of the left hand in a patient with TAO. Inflammatory thrombus in distal arteries and veins causes digital ischemia, ulceration, and necrosis.
Image: “Raynaud Phenomenon.” by Shah J, Billington AR, Elston JB, Payne WG. License: CC BY 2.0The diagnosis can be established without biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma if the following criteria are met MET Preoperative Care:
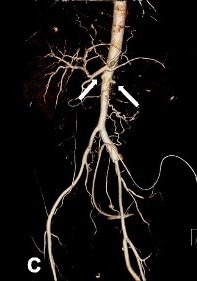
Abdominal aorta CT angiography of a patient with TAO showing total occlusion of both renal arteries (white arrows)
Image: “Contrast-enhanced abdominal CT and abdominal aorta CT angiography” by Yun et al. 2015. License: CC BY 4.0, edited by Lecturio.