Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. The disorder can usually be managed with lifestyle modification and medications, but occasionally, vascular intervention or surgery are required. Age, sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria, smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity, and diet are contributing factors to hypertension, which can lead to heart attack Heart attack Mi is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, stroke, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), and CKD CKD Chronic kidney disease (CKD) is kidney impairment that lasts for ≥ 3 months, implying that it is irreversible. Hypertension and diabetes are the most common causes; however, there are a multitude of other etiologies. In the early to moderate stages, CKD is usually asymptomatic and is primarily diagnosed by laboratory abnormalities. Chronic Kidney Disease if not managed properly. Many individuals with hypertension are undiagnosed or undertreated.
Last updated: May 16, 2024
Hypertension is defined as a BP > 130/80 mm Hg.
Primary hypertension:
The pathogenesis of primary hypertension is poorly understood but is most likely the result of numerous genetic and environmental factors affecting cardiovascular and kidney structure and function. Risk factors:
Secondary hypertension:
| BP category | Systolic BP (mm Hg) | Diastolic BP (mm Hg) | |
|---|---|---|---|
| Normal BP | < 120 mm Hg | AND | < 80 mm Hg |
| Elevated BP | 120–129 mm Hg | AND | < 80 mm Hg |
| Stage 1 Stage 1 Trypanosoma brucei/African trypanosomiasis hypertension | 130–139 mm Hg | OR | 80–89 mm Hg |
| Stage 2 hypertension | ≥ 140 mm Hg | OR | ≥ 90 mm Hg |
Evaluates for left ventricular hypertrophy Ventricular Hypertrophy Tetralogy of Fallot (LVH): strain pattern often seen with hypertensive heart disease
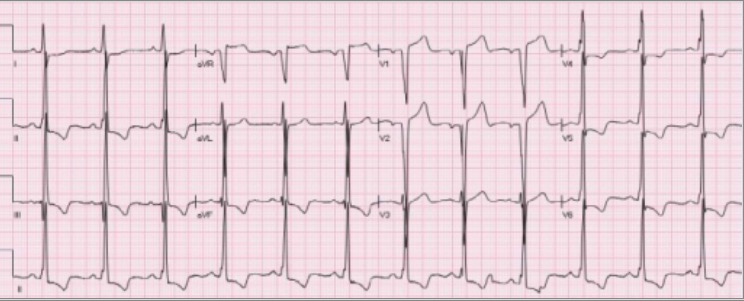
ECG showing left ventricular hypertrophy (LVH):
Note exaggerated amplitude of the QRS complexes and abnormal repolarization pattern typical of LVH.
| Pharmacologic class | Use | Avoid in |
|---|---|---|
| Thiazide Thiazide Heterocyclic compounds with sulfur and nitrogen in the ring. This term commonly refers to the benzothiadiazines that inhibit sodium-potassium-chloride symporters and are used as diuretics. Hyponatremia diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication | Edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema, osteoporosis Osteoporosis Osteoporosis refers to a decrease in bone mass and density leading to an increased number of fractures. There are 2 forms of osteoporosis: primary, which is commonly postmenopausal or senile; and secondary, which is a manifestation of immobilization, underlying medical disorders, or long-term use of certain medications. Osteoporosis, calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes nephrolithiasis Nephrolithiasis Nephrolithiasis is the formation of a stone, or calculus, anywhere along the urinary tract caused by precipitations of solutes in the urine. The most common type of kidney stone is the calcium oxalate stone, but other types include calcium phosphate, struvite (ammonium magnesium phosphate), uric acid, and cystine stones. Nephrolithiasis | Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with gout Gout Gout is a heterogeneous metabolic disease associated with elevated serum uric acid levels (> 6.8 mg/dL) and abnormal deposits of monosodium urate in tissues. The condition is often familial and is initially characterized by painful, recurring, and usually monoarticular acute arthritis, or “gout flare,” followed later by chronic deforming arthritis. Gout, pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, and electrolyte disorders |
| β-blockers | Prior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, stable angina Stable angina Persistent and reproducible chest discomfort usually precipitated by a physical exertion that dissipates upon cessation of such an activity. The symptoms are manifestations of myocardial ischemia. Stable and Unstable Angina, chronic heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), atrial arrhythmias | Heart block, sick sinus syndrome Sick Sinus Syndrome Sick sinus syndrome (SSS), also known as sinus node dysfunction, is characterized by degeneration of the sinoatrial (SA) node, the heart’s primary pacemaker. Patients with SSS may be asymptomatic or may present with tachycardia or bradycardia. Sick Sinus Syndrome, COPD COPD Chronic obstructive pulmonary disease (COPD) is a lung disease characterized by progressive, largely irreversible airflow obstruction. The condition usually presents in middle-aged or elderly persons with a history of cigarette smoking. Signs and symptoms include prolonged expiration, wheezing, diminished breath sounds, progressive dyspnea, and chronic cough. Chronic Obstructive Pulmonary Disease (COPD), asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma, acute heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) |
| ACEis ACEIs A class of drugs whose main indications are the treatment of hypertension and heart failure. They exert their hemodynamic effect mainly by inhibiting the renin-angiotensin system. They also modulate sympathetic nervous system activity and increase prostaglandin synthesis. They cause mainly vasodilation and mild natriuresis without affecting heart rate and contractility. Heart Failure and Angina Medication | Heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, unstable angina Unstable angina Precordial pain at rest, which may precede a myocardial infarction. Stable and Unstable Angina, MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, kidney disease | Pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, angioedema Angioedema Angioedema is a localized, self-limited (but potentially life-threatening), nonpitting, asymmetrical edema occurring in the deep layers of the skin and mucosal tissue. The common underlying pathophysiology involves inflammatory mediators triggering significant vasodilation and increased capillary permeability. Angioedema |
| ARBs ARBs Agents that antagonize angiotensin receptors. Many drugs in this class specifically target the angiotensin type 1 receptor. Heart Failure and Angina Medication | Heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR), diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, kidney disease | Pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care |
| Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes channel blockers | Atrial tachyarrhythmias, Raynaud syndrome | Heart block, sick sinus syndrome Sick Sinus Syndrome Sick sinus syndrome (SSS), also known as sinus node dysfunction, is characterized by degeneration of the sinoatrial (SA) node, the heart’s primary pacemaker. Patients with SSS may be asymptomatic or may present with tachycardia or bradycardia. Sick Sinus Syndrome, pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) |
| Aldosterone Aldosterone A hormone secreted by the adrenal cortex that regulates electrolyte and water balance by increasing the renal retention of sodium and the excretion of potassium. Hyperkalemia receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors blockers | Prior MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) | Pregnancy Pregnancy The status during which female mammals carry their developing young (embryos or fetuses) in utero before birth, beginning from fertilization to birth. Pregnancy: Diagnosis, Physiology, and Care, hyperkalemia Hyperkalemia Hyperkalemia is defined as a serum potassium (K+) concentration >5.2 mEq/L. Homeostatic mechanisms maintain the serum K+ concentration between 3.5 and 5.2 mEq/L, despite marked variation in dietary intake. Hyperkalemia can be due to a variety of causes, which include transcellular shifts, tissue breakdown, inadequate renal excretion, and drugs. Hyperkalemia |
Hypertension is a risk factor for atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis, which can lead to MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction, ischemic heart disease Ischemic heart disease Coronary heart disease (CHD), or ischemic heart disease, describes a situation in which an inadequate supply of blood to the myocardium exists due to a stenosis of the coronary arteries, typically from atherosclerosis. Coronary Heart Disease, cerebrovascular accident Cerebrovascular accident An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke, and peripheral ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage.
Other conditions associated with hypertension include: