Gout is a heterogeneous metabolic disease associated with elevated serum uric acid Uric acid An oxidation product, via xanthine oxidase, of oxypurines such as xanthine and hypoxanthine. It is the final oxidation product of purine catabolism in humans and primates, whereas in most other mammals urate oxidase further oxidizes it to allantoin. Nephrolithiasis levels (> 6.8 mg/dL) and abnormal deposits of monosodium urate in tissues. The condition is often familial and is initially characterized by painful, recurring, and usually monoarticular acute arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, or “gout flare,” followed later by chronic deforming arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis. The kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy can also be affected, and urate crystals can precipitate as chalkstone-like deposits (“tophi”) in the soft tissues, synovial tissues, or in bones near the joints. Hyperuricemia is due to overproduction and/or underexcretion of uric acid Uric acid An oxidation product, via xanthine oxidase, of oxypurines such as xanthine and hypoxanthine. It is the final oxidation product of purine catabolism in humans and primates, whereas in most other mammals urate oxidase further oxidizes it to allantoin. Nephrolithiasis and is a necessary but insufficient precondition to developing urate crystal deposition disease (most hyperuricemic individuals never experience clinical gout). The most commonly involved joint is the first metatarsophalangeal joint Metatarsophalangeal Joint Foot: Anatomy. The identification Identification Defense Mechanisms of urate crystals in joint aspirate or tophi is diagnostic. Effective therapies to relieve the pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways of a gout flare include nonsteroidal anti-inflammatory drugs ( NSAIDs NSAIDS Primary vs Secondary Headaches), colchicine Colchicine A major alkaloid from colchicum autumnale l. And found also in other colchicum species. Its primary therapeutic use is in the treatment of gout. Gout Drugs, and glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids; the choice of therapy depends on the individual and if there are any contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation.
Last updated: May 16, 2024
Drugs causing acute precipitation of gout: FACT
F: Furosemide diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication
A: Aspirin/Alcohol
C: Anti-Cancer drugs (e.g., cyclosporine Cyclosporine A cyclic undecapeptide from an extract of soil fungi. It is a powerful immunosupressant with a specific action on T-lymphocytes. It is used for the prophylaxis of graft rejection in organ and tissue transplantation. Immunosuppressants)
T: Thiazide diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication
Upon resolution of an acute gout flare, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship enter an intercritical (between-flares) period.

Tophi at different sites throughout the body
Image: “Tophaceous gout affecting the right great toe and finger interphalangeal joints” by Arthritis Research UK Primary Care Centre, Primary Care Sciences, Keele University, Keele, UK. License: CC BY 2.0
Gouty tophi affecting the hand
Image: “Gouty tophus” by Service de Dermatologie, Chu Hassan II, Fès, Maroc. License: CC BY 2.0
26-year-old man with tophaceous gout that has manifested as tophi in the ear
Image: “Gouty Tophi in the Helix of the Ear” by Michael McCullough. License: CC BY 2.0
Monosodium urate crystals, negatively birefringent (appearing as needle-like yellow crystals when parallel to the polarizing light with a red compensator, and blue when perpendicular), from a patient’s joint aspirate. This finding is diagnostic of gout.
Image: “Monosodium Urate Crystals in Elbow Joint Fluid” by Ed Uthman. License: CC BY 2.0Management differs for acute and chronic gout.
The goal of management is to reduce inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation.
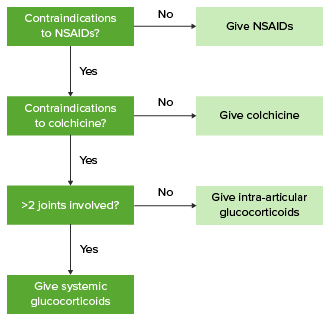
Algorithm for the management of acute gout
Image by Lecturio.The goal of management is to minimize urate deposition in tissues.
General measures
Medical measures
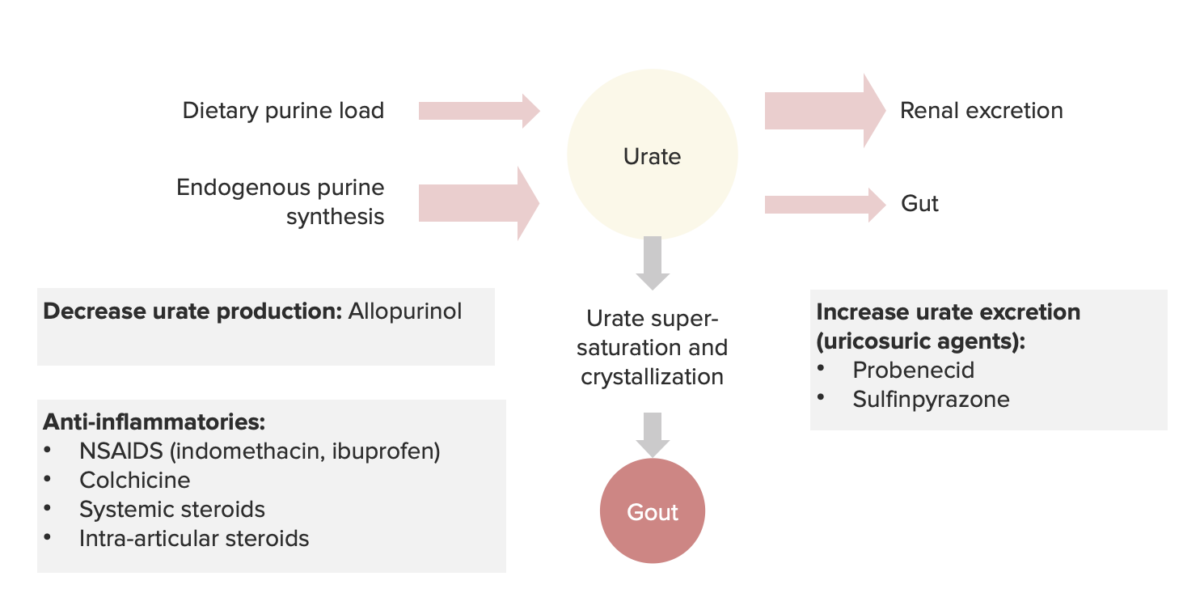
Summary of the pathophysiology and drugs used for gout
Image by Lecturio.The following conditions are differential diagnoses of gout: