Peptic ulcer disease (PUD) refers to the full-thickness ulcerations of duodenal or gastric mucosa Gastric mucosa Lining of the stomach, consisting of an inner epithelium, a middle lamina propria, and an outer muscularis mucosae. The surface cells produce mucus that protects the stomach from attack by digestive acid and enzymes. When the epithelium invaginates into the lamina propria at various region of the stomach (cardia; gastric fundus; and pylorus), different tubular gastric glands are formed. These glands consist of cells that secrete mucus, enzymes, hydrochloric acid, or hormones. Stomach: Anatomy. The ulcerations form when exposure to acid and digestive enzymes Enzymes Enzymes are complex protein biocatalysts that accelerate chemical reactions without being consumed by them. Due to the body's constant metabolic needs, the absence of enzymes would make life unsustainable, as reactions would occur too slowly without these molecules. Basics of Enzymes overcomes mucosal defense mechanisms Defense mechanisms Defense mechanisms are normal subconscious means of resolving inner conflicts between an individual's subjective moral sense and their thoughts, feelings, or actions. Defense mechanisms serve to protect the self from unpleasant feelings (anxiety, shame, and/or guilt) and are divided into pathologic, immature, mature, neurotic, and other types. Defense Mechanisms. The most common etiologies include Helicobacter pylori Helicobacter pylori A spiral bacterium active as a human gastric pathogen. It is a gram-negative, urease-positive, curved or slightly spiral organism initially isolated in 1982 from patients with lesions of gastritis or peptic ulcers in Western Australia. Helicobacter pylori was originally classified in the genus campylobacter, but RNA sequencing, cellular fatty acid profiles, growth patterns, and other taxonomic characteristics indicate that the micro-organism should be included in the genus Helicobacter. It has been officially transferred to Helicobacter gen. Helicobacter ( H. pylori H. pylori A spiral bacterium active as a human gastric pathogen. It is a gram-negative, urease-positive, curved or slightly spiral organism initially isolated in 1982 from patients with lesions of gastritis or peptic ulcers in Western Australia. Helicobacter pylori was originally classified in the genus campylobacter, but RNA sequencing, cellular fatty acid profiles, growth patterns, and other taxonomic characteristics indicate that the micro-organism should be included in the genus Helicobacter. It has been officially transferred to Helicobacter gen. Helicobacter) infection and prolonged use of nonsteroidal anti-inflammatory drugs ( NSAIDs NSAIDS Primary vs Secondary Headaches). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may be asymptomatic or may present with abdominal pain Abdominal Pain Acute Abdomen, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, and early satiety Early Satiety Bariatric Surgery. Peptic ulcer disease typically responds well to medical treatment consisting of H. pylori H. pylori A spiral bacterium active as a human gastric pathogen. It is a gram-negative, urease-positive, curved or slightly spiral organism initially isolated in 1982 from patients with lesions of gastritis or peptic ulcers in Western Australia. Helicobacter pylori was originally classified in the genus campylobacter, but RNA sequencing, cellular fatty acid profiles, growth patterns, and other taxonomic characteristics indicate that the micro-organism should be included in the genus Helicobacter. It has been officially transferred to Helicobacter gen. Helicobacter eradication, eliminating risk factors, and proton pump Pump ACES and RUSH: Resuscitation Ultrasound Protocols inhibitors (PPIs). If left untreated, it can lead to bleeding, perforation Perforation A pathological hole in an organ, blood vessel or other soft part of the body, occurring in the absence of external force. Esophagitis, gastric outlet obstruction Gastric Outlet Obstruction Hypertrophic Pyloric Stenosis, and gastric cancer Gastric cancer Gastric cancer is the 3rd-most common cause of cancer-related deaths worldwide. The majority of cases are from adenocarcinoma. The modifiable risk factors include Helicobacter pylori infection, smoking, and nitrate-rich diets. Gastric Cancer.
Last updated: May 21, 2025
A peptic ulcer is a mucosal defect in the wall of the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy or duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy that penetrates the muscularis mucosa.
In many cases, the listed etiologies are not enough to produce PUD. Contributing risk factors to PUD development:
| Type | Location | Acid level |
|---|---|---|
| I | Lesser curve of the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy at the incisura angularis | Low to normal |
| II | Gastric body; coexists with duodenal ulcer | Increased |
| III | In the pyloric channel (within 3 cm of pylorus Pylorus The region between the sharp indentation at the lower third of the stomach (incisura angularis) and the junction of the pylorus with the duodenum. Pyloric antral glands contain mucus-secreting cells and gastrin-secreting endocrine cells (g cells). Stomach: Anatomy) | Increased |
| IV | Proximal gastroesophageal ulcer | Normal |
| V | Anywhere in the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy ( aspirin Aspirin The prototypical analgesic used in the treatment of mild to moderate pain. It has anti-inflammatory and antipyretic properties and acts as an inhibitor of cyclooxygenase which results in the inhibition of the biosynthesis of prostaglandins. Aspirin also inhibits platelet aggregation and is used in the prevention of arterial and venous thrombosis. Nonsteroidal Antiinflammatory Drugs (NSAIDs)/ NSAID NSAID Nonsteroidal antiinflammatory drugs (NSAIDs) are a class of medications consisting of aspirin, reversible NSAIDs, and selective NSAIDs. NSAIDs are used as antiplatelet, analgesic, antipyretic, and antiinflammatory agents. Nonsteroidal Antiinflammatory Drugs (NSAIDs) induced) | Normal |
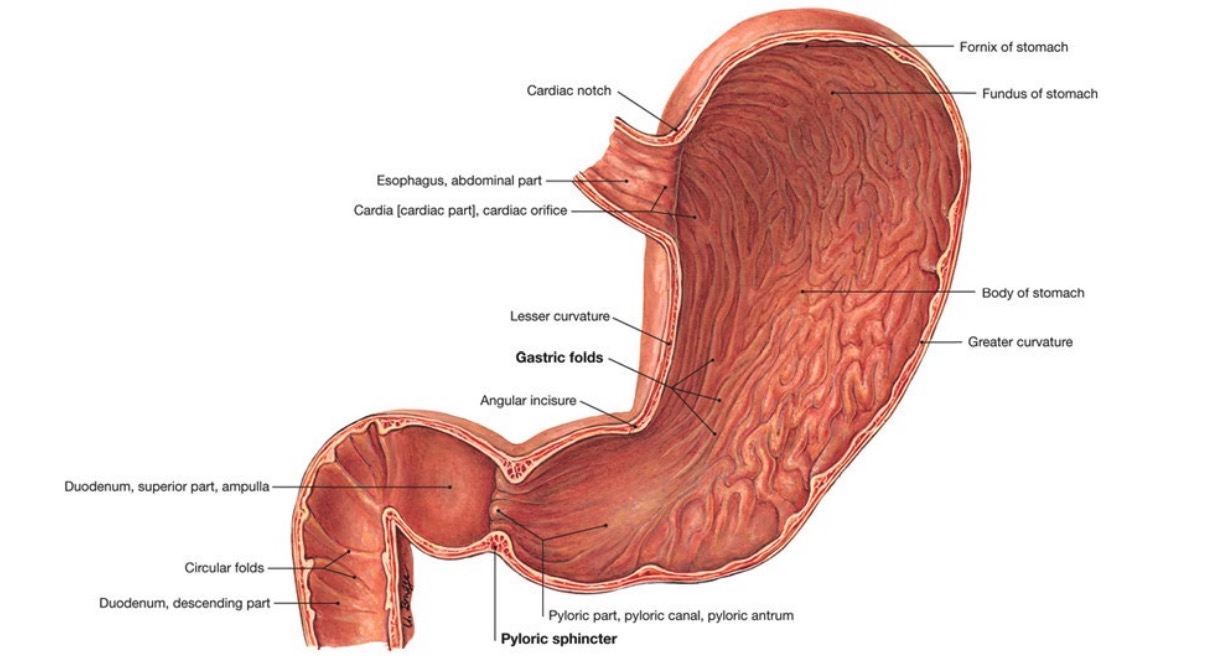
Anatomic components of the stomach
Image by Lecturio.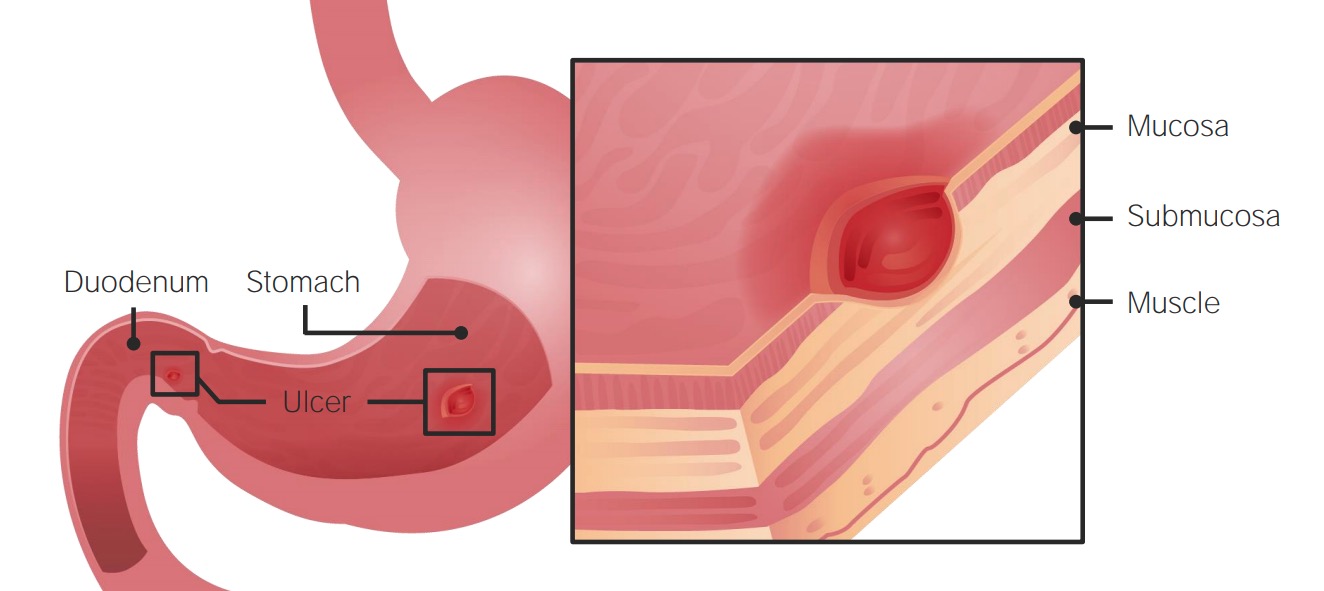
Development of PUD in the stomach and duodenum
Image by Lecturio.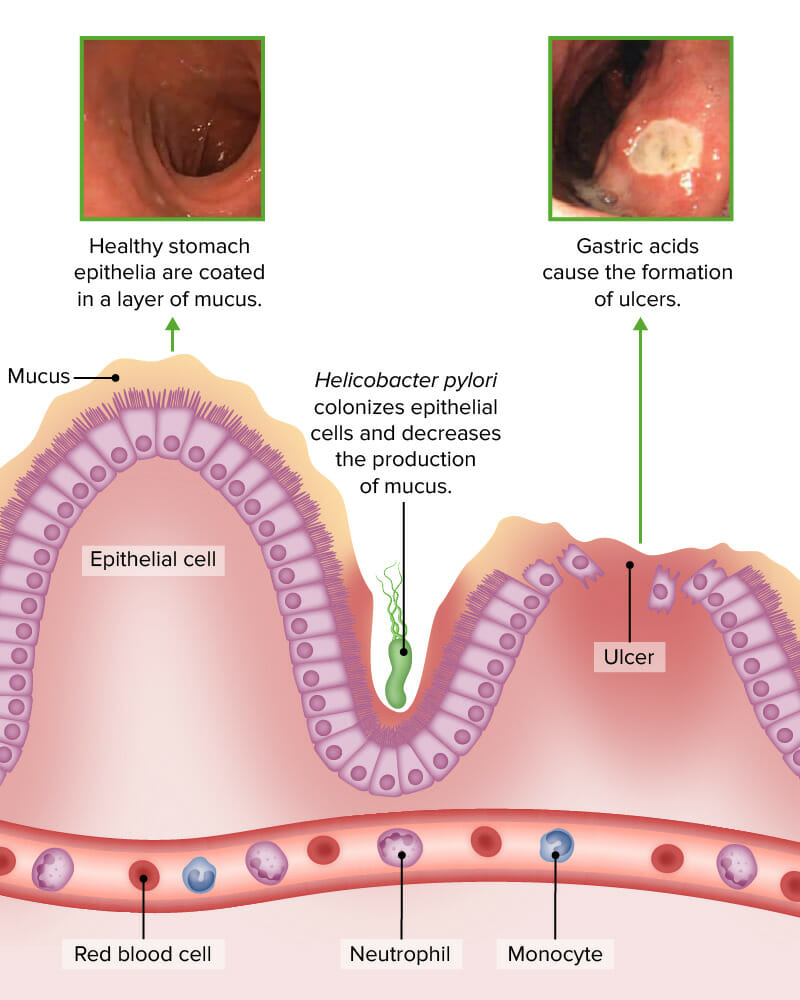
Helicobacter infection decreases mucus production and increases risk for ulcer formation.
Image by Lecturio (credit top photos: Image: “Helicobacter infection decreases mucus production and causes peptic ulcers.“ by Janice Carr, Centers for Disease Control and Prevention. License: CC BY 4.0)Review of common risk factors:
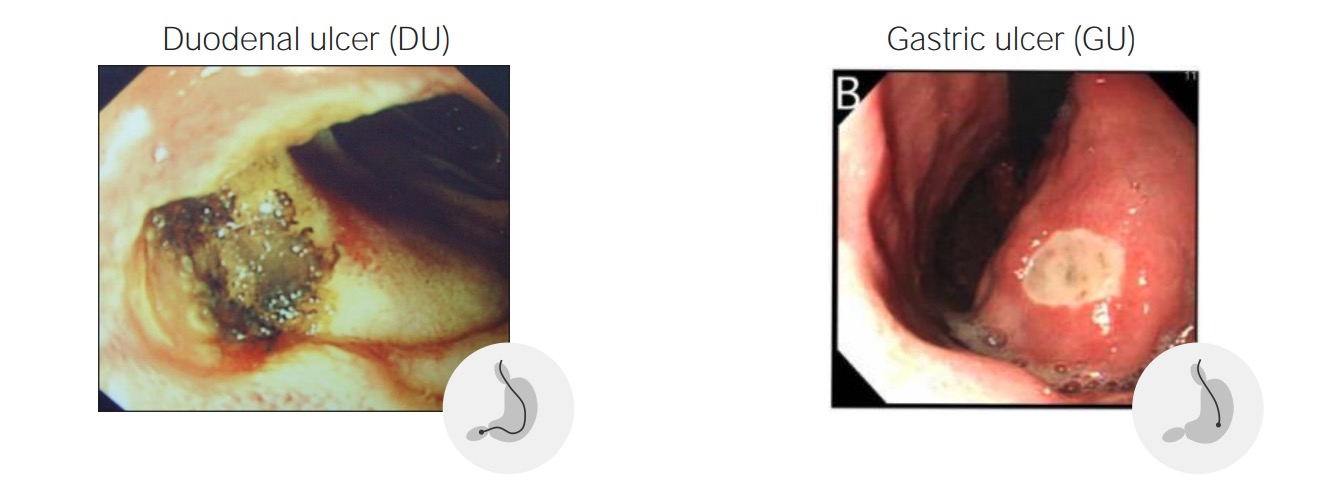
Endoscopic view of duodenal (left) and gastric (right) ulcerative lesions
Image: “F0002” by the Department of Surgery, King Fahad Specialist Hospital, Dammam, Saudi Arabia. License: CC BY 2.0, and Image: “F1” by the Department of Psychosomatic Internal Medicine, Health Sciences University of Hokkaido, Japan. License: CC BY 2.0, edited by Lecturio.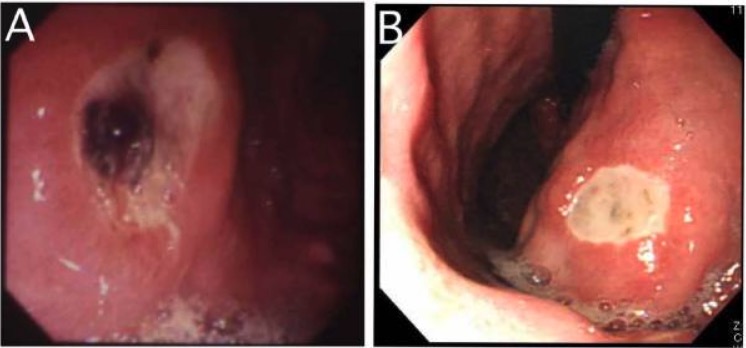
A: esophagogastroduodenoscopy of an open gastric ulcer with exposed vessel
B: gastric ulcer without active bleeding