Hypertrophic pyloric stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) is hypertrophy Hypertrophy General increase in bulk of a part or organ due to cell enlargement and accumulation of fluids and secretions, not due to tumor formation, nor to an increase in the number of cells (hyperplasia). Cellular Adaptation and hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation of the pyloric sphincter muscle. The condition is the most common cause of gastrointestinal obstruction in infants. Affected newborns typically present after the third to fifth week of life with progressive non-bilious vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia and a firm, olive-like mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast in the epigastrium Epigastrium Surgical Anatomy of the Abdomen. Ultrasound confirms the diagnosis based on the thickness and length of the pyloric muscle and channel diameter. Initial treatment consists of fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome with correction of electrolyte imbalances, followed by either open or laparoscopic pyloromyotomy.
Last updated: Mar 27, 2025
Hypertrophic pyloric stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) is a functional obstruction of the gastric outlet caused by hypertrophy Hypertrophy General increase in bulk of a part or organ due to cell enlargement and accumulation of fluids and secretions, not due to tumor formation, nor to an increase in the number of cells (hyperplasia). Cellular Adaptation and hyperplasia Hyperplasia An increase in the number of cells in a tissue or organ without tumor formation. It differs from hypertrophy, which is an increase in bulk without an increase in the number of cells. Cellular Adaptation of both the circular and longitudinal layers of the pylorus Pylorus The region between the sharp indentation at the lower third of the stomach (incisura angularis) and the junction of the pylorus with the duodenum. Pyloric antral glands contain mucus-secreting cells and gastrin-secreting endocrine cells (g cells). Stomach: Anatomy in infants.
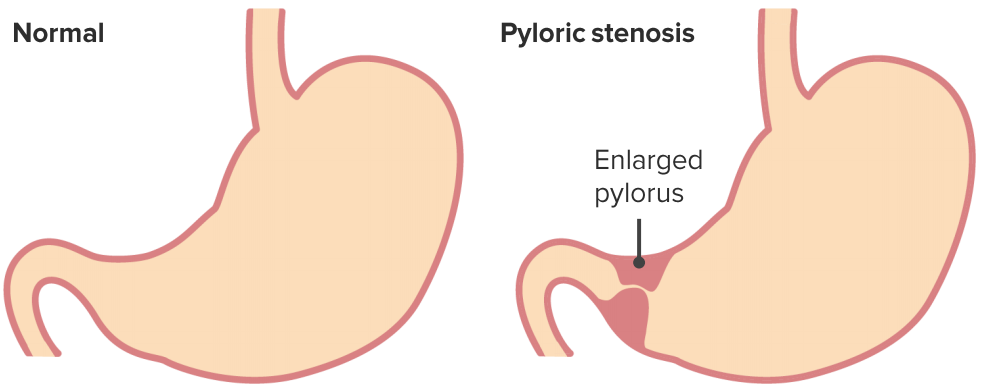
Hypertrophic pyloric stenosis
Image by Lecturio.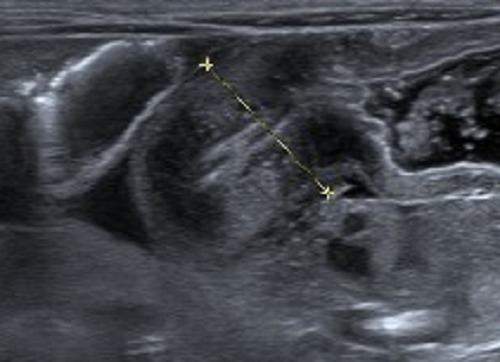
Hypertrophic pyloric stenosis
Image: “USG Confirmed IHPS” by Department of Pediatric Surgery, School of Medical Sciences, Universiti Sains Malaysia. License: CC BY 3.0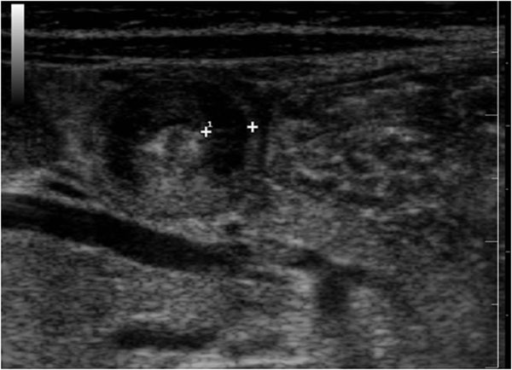
Ultrasound features of hypertrophic pyloric stenosis. On the cross scanning with the infant in the supine position, the “doughnut sign” is visualized consisting of a prominent anechoic rim of thickened muscle, and an echogenic center of mucosa and submucosa.
Image: “Ultrasound features of hypertrophic pyloric stenosis” by Second University of Naples, Department of Clinical and Experimental Internistic F, Magrassi, Naples, Italy. License: CC BY 2.0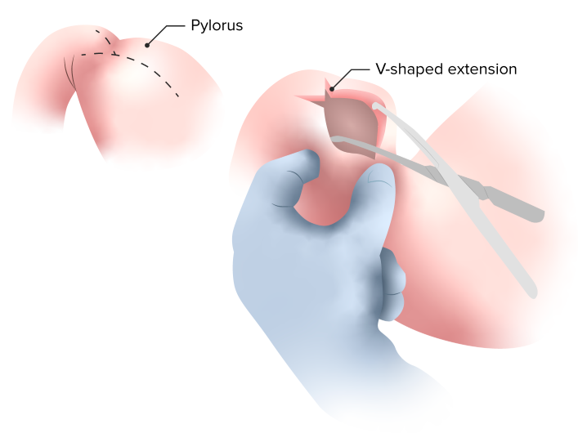
This is the classic definitive surgical treatment of hypertrophic pyloric stenosis called a “Ramstedt pyloromyotomy”, in which a longitudinal incision of the anterior surface of the pylorus is made down through the muscle layer only to the level of the submucosa, leaving the submucosa and mucosa in a prolapsed state.
Image by Lecturio.