Oral cancer includes neoplasms Neoplasms New abnormal growth of tissue. Malignant neoplasms show a greater degree of anaplasia and have the properties of invasion and metastasis, compared to benign neoplasms. Benign Bone Tumors arising from the oral mucosa Oral mucosa Lining of the oral cavity, including mucosa on the gums; the palate; the lip; the cheek; floor of the mouth; and other structures. The mucosa is generally a nonkeratinized stratified squamous epithelium covering muscle, bone, or glands but can show varying degree of keratinization at specific locations. Stomatitis, tonsils Tonsils Tonsillitis, and salivary glands Salivary glands The salivary glands are exocrine glands positioned in and around the oral cavity. These glands are responsible for secreting saliva into the mouth, which aids in digestion. There are 3 major paired salivary glands: the sublingual, submandibular, and parotid glands. Salivary Glands: Anatomy. More than 90% of oral cancers are squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC) (SCC). Risk factors include premalignant lesions, tobacco chewing/ smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, alcohol consumption, and HPV HPV Human papillomavirus (HPV) is a nonenveloped, circular, double-stranded DNA virus belonging to the Papillomaviridae family. Humans are the only reservoir, and transmission occurs through close skin-to-skin or sexual contact. Human papillomaviruses infect basal epithelial cells and can affect cell-regulatory proteins to result in cell proliferation. Papillomavirus (HPV) infection. The patient typically presents with a nonhealing, oral mucosa Oral mucosa Lining of the oral cavity, including mucosa on the gums; the palate; the lip; the cheek; floor of the mouth; and other structures. The mucosa is generally a nonkeratinized stratified squamous epithelium covering muscle, bone, or glands but can show varying degree of keratinization at specific locations. Stomatitis ulcer, oral pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast, or a red/white lesion. Lesions persisting beyond 3 weeks warrant further evaluation with a biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Additional evaluation of the extent of the disease is made with imaging studies. Depending on the stage of the disease, management options include surgical resection, radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy, and chemotherapy Chemotherapy Osteosarcoma. The involvement of lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy is the most important prognostic factor.
Last updated: May 17, 2024

Erythroplakia: red, sharply demarcated, velvety lesion usually found on the buccal mucosa
Image: “Clinical characteristics of narrow-band imaging of oral erythroplakia and its correlation with pathology” by Yang SW, Lee YS, Chang LC, Hwang CC, Luo CM, Chen TA. License: CC BY 4.0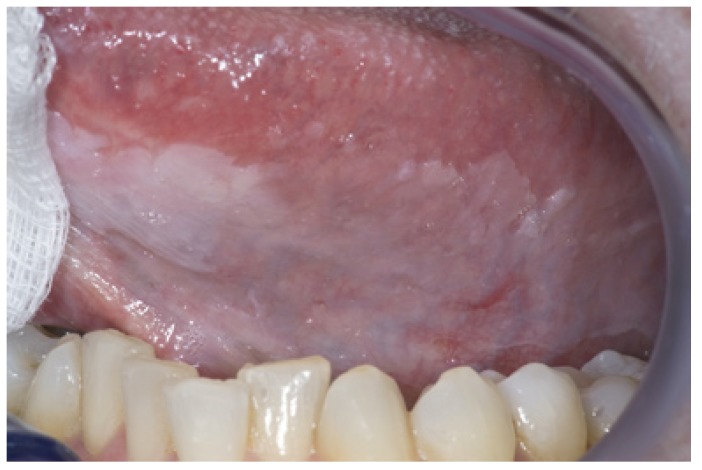
Leukoplakia: homogeneous, flat, white lesion(s) on the tongue of a 53-year-old man
Image: “Oral leukoplakia, the ongoing discussion on definition and terminology” by van der Waal, I. License: CC BY 2.5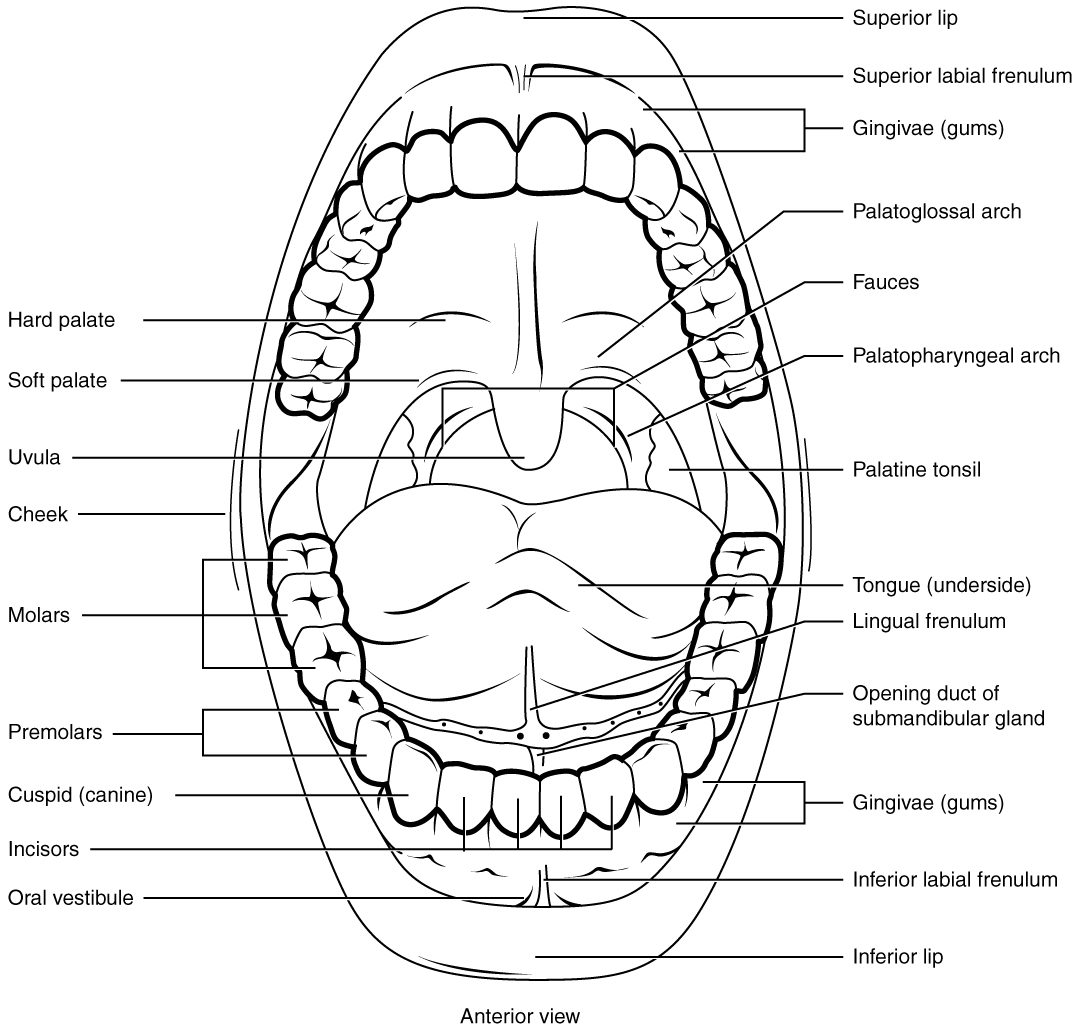
Oral cavity:
Common areas for oral cancer include the tongue, the floor of the mouth, and the retromolar trigone (the area posterior to the molars).

Oral carcinoma: exophytic tongue masses noted on exam.
On biopsy, the 3 exophytic lesions revealed oral carcinomas, while the surrounding hyperkeratotic area showed the histologic features of oral lichen planus.

Mouth cancer in a male smoker
Image: “Mouth cancer bionerd” by Bionerd. License: CC BY 3.0Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is recommended for suspicious oral lesions lasting 3 or more weeks:
| Stage | Description |
|---|---|
| 0 | TisN0M0 (in situ or cancer limited to epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology) |
| I | T1N0M0 (lesion ≤ 2 cm and without node involvement or distant spread) |
| II | T2N0M0 (lesion > 2 cm but < 4 cm without node involvement or distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis) |
| III |
|
| IV | Invasion of adjacent structures or distant metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis |