Genital herpes infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are common sexually transmitted infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease caused by herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2) type 1 Type 1 Spinal Muscular Atrophy or 2. Herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology type 1 Type 1 Spinal Muscular Atrophy is more commonly associated with non-genital herpes, while HSV-2 is more commonly associated with genital herpes. Primary infection Primary infection Herpes Simplex Virus 1 and 2 often presents with systemic, prodromal symptoms followed by clusters of painful, fluid-filled vesicles Vesicles Female Genitourinary Examination on an erythematous base, dysuria Dysuria Painful urination. It is often associated with infections of the lower urinary tract. Urinary Tract Infections (UTIs), and painful lymphadenopathy Lymphadenopathy Lymphadenopathy is lymph node enlargement (> 1 cm) and is benign and self-limited in most patients. Etiologies include malignancy, infection, and autoimmune disorders, as well as iatrogenic causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Lymphadenopathy. Primary infection Primary infection Herpes Simplex Virus 1 and 2 can also be asymptomatic. Herpes infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are unique in that the virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology is able to remain dormant in the neuronal ganglia, which allows for recurrent infections Recurrent infections Common Variable Immunodeficiency (CVID). Recurrent outbreaks Outbreaks Sudden increase in the incidence of a disease. The concept includes epidemics and pandemics. Influenza Viruses/Influenza are usually less severe than the initial infection. Treatment is with antiviral Antiviral Antivirals for Hepatitis B therapy, primarily acyclovir Acyclovir A guanosine analog that acts as an antimetabolite. Viruses are especially susceptible. Used especially against herpes. Herpes Zoster (Shingles).
Last updated: May 17, 2024
Genital herpes is a mucocutaneous ulcerative disease caused by either herpes simplex Herpes Simplex A group of acute infections caused by herpes simplex virus type 1 or type 2 that is characterized by the development of one or more small fluid-filled vesicles with a raised erythematous base on the skin or mucous membrane. It occurs as a primary infection or recurs due to a reactivation of a latent infection. Congenital TORCH Infections virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology ( HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2) type 1 Type 1 Spinal Muscular Atrophy or 2.
HSV-1:
HSV-2:
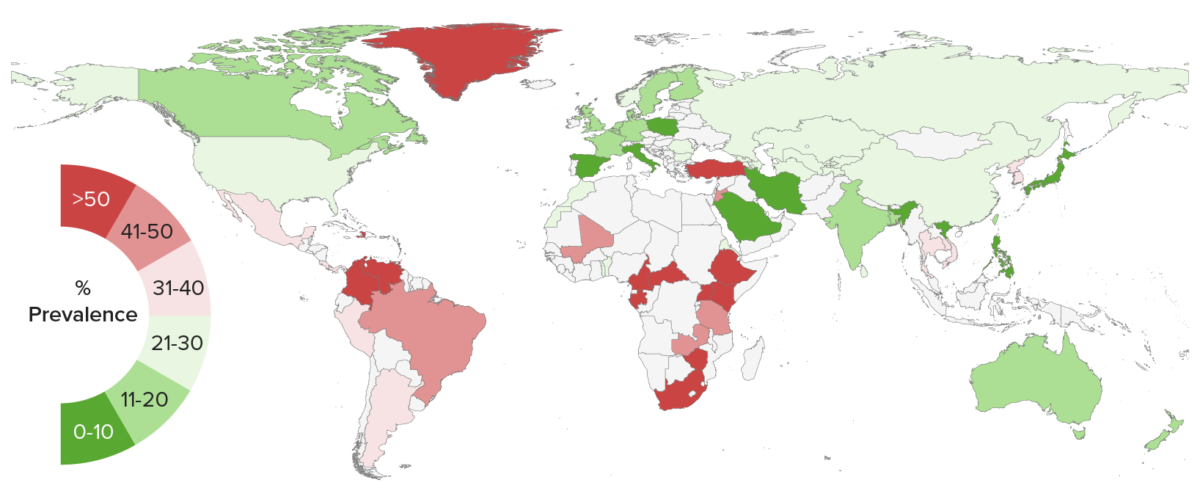
Global seroprevalence of herpes simplex virus type 2 infection
Image by Lecturio.Primary infection Primary infection Herpes Simplex Virus 1 and 2 occurs when the virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology travels through tiny breaks or even microscopic abrasions Abrasions Corneal Abrasions, Erosion, and Ulcers in the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions or mucous membranes in the mouth or genital areas.
Recurrent infection is due to HSV HSV Herpes simplex virus (HSV) is a double-stranded DNA virus belonging to the family Herpesviridae. Herpes simplex virus commonly causes recurrent infections involving the skin and mucosal surfaces, including the mouth, lips, eyes, and genitals. Herpes Simplex Virus 1 and 2 reactivation Reactivation Herpes Simplex Virus 1 and 2.
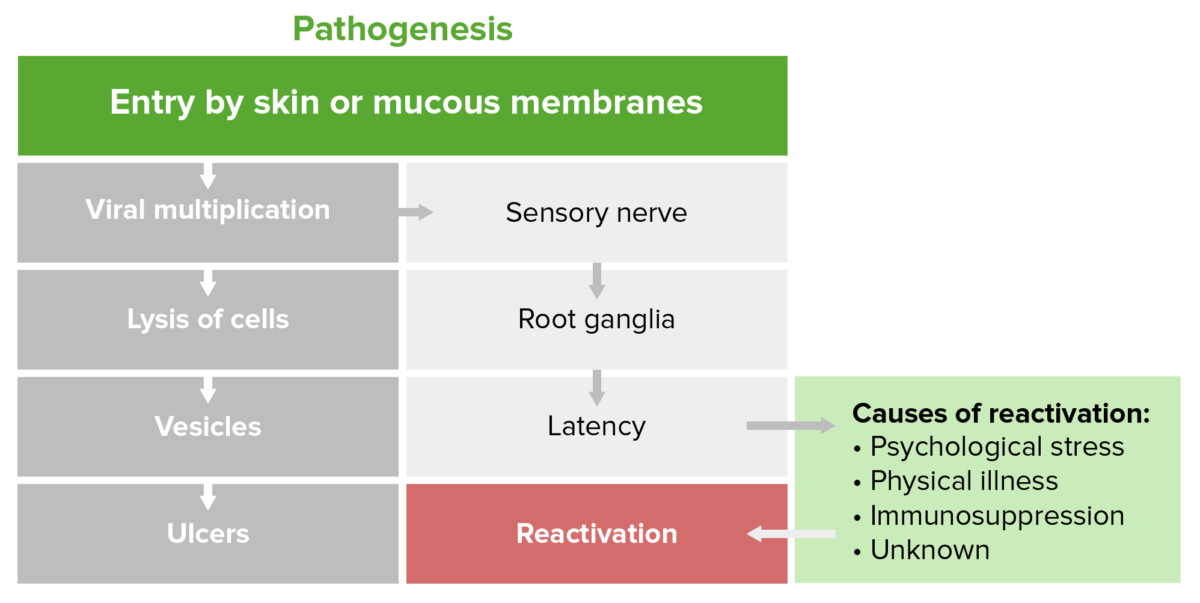
Pathophysiology of herpes
Image by Lecturio.Genital herpes infection can be symptomatic or asymptomatic/subclinical and is defined as either primary, non-primary, or recurrent.
Other forms of herpetic infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease associated with HSV-1 include:

Crusted blister scabs from broken and healing vesicles of cold sores (“fever blisters,” herpes simplex labialis) which are a common viral infection.
Cold sores start as a cluster of tiny, fluid-filled blisters on and around the lips. After the blisters break, a scab forms that can last for several days.
Cold sores usually heal in 2 to 3 weeks without leaving a scar.
Cold sores spread from person to person via close contact, such as kissing. These sores are usually caused by HSV-1 (HSV-1).
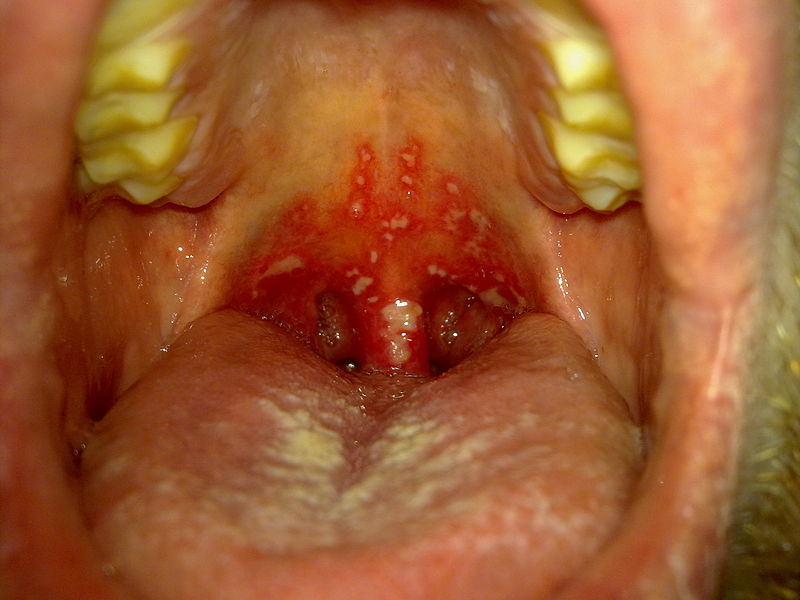
Herpetic gingivostomatitis
Image: “Stomatitis herpetica” by Klaus D. Peter. License: CC BY 3.0 DE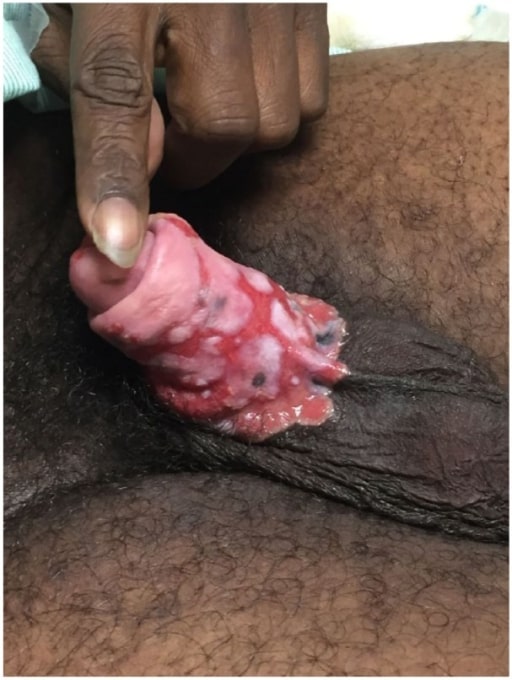
Penile ulcers due to chronic refractory genital herpes in a patient with AIDS
Image: “Penile ulcers” by University of Texas Medical Branch School of Medicine, Galveston, TX, USA. License: CC BY 3.0
Herpetic whitlow
Image: “Herpetic Whitlow” by Salford Royal Foundation Trust, Manchester, UK. License: CC BY 3.0A diagnosis of genital herpes should be confirmed with laboratory testing. The classic appearance is that of multiple, clear, fluid-filled vesicles Vesicles Female Genitourinary Examination on an erythematous base. A diagnostic clue is that the vesicles Vesicles Female Genitourinary Examination are painful and tend to be clustered into small groups, although the presentation can vary widely.
Laboratory testing possibilities include:
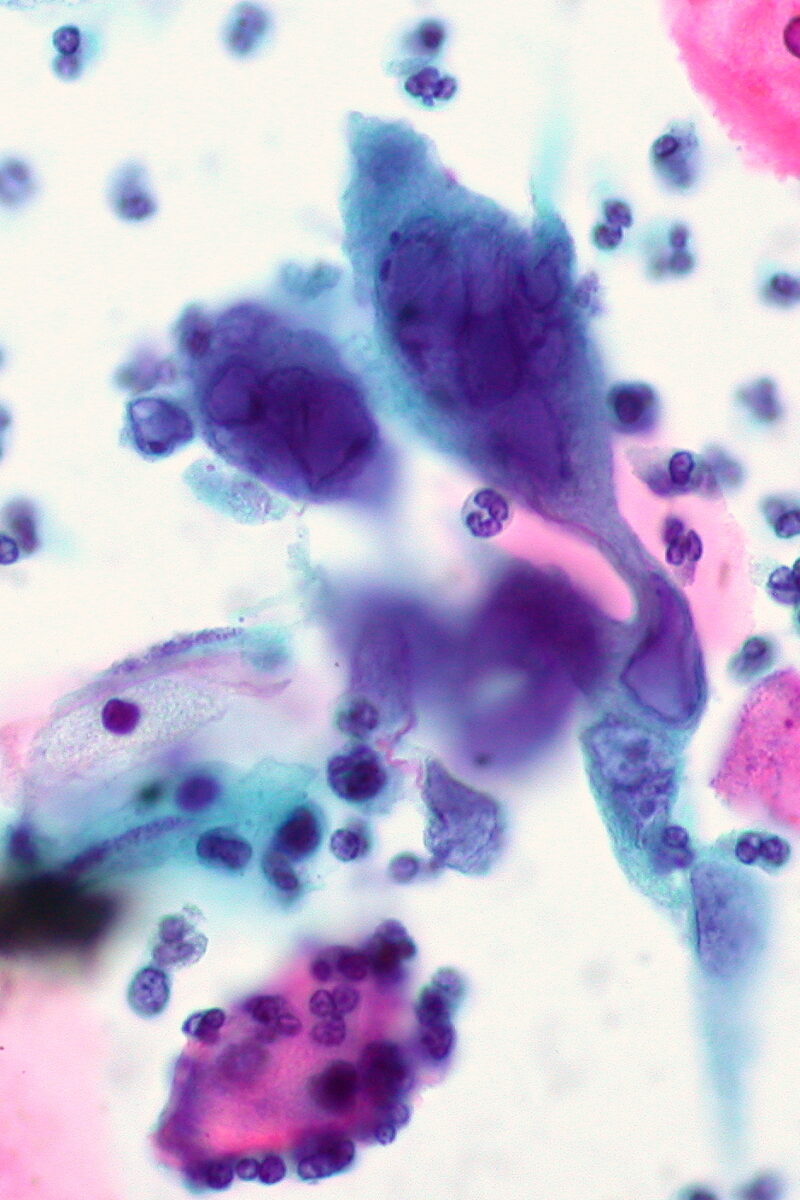
Herpes infection with classic multinucleated giant cell on ThinPrep Pap smear
Image: “Herpes infection on ThinPrep Pap smear” by Ed Uthman. License: CC BY 2.0Prevention is accomplished through patient education, the use of barrier contraceptive devices, and chronic suppressive therapy.
The differential diagnosis of genital herpes includes the following conditions: