Varicella-zoster virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology (VZV) is a linear, double-stranded DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology in the Herpesviridae Herpesviridae A family of enveloped, linear, double-stranded DNA viruses infecting a wide variety of animals. Subfamilies, based on biological characteristics, include: alphaherpesvirinae; betaherpesvirinae; and gammaherpesvirinae. Herpes Simplex Virus 1 and 2 family. Varicella-zoster infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are highly contagious and transmitted through aerosolized respiratory droplets or contact with infected skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions. Chickenpox is the primary infection Primary infection Herpes Simplex Virus 1 and 2 and occurs most commonly in children. The typical clinical presentation includes prodromal symptoms and a generalized, intensely pruritic vesicular rash Rash Rocky Mountain Spotted Fever. Shingles (also known as herpes zoster) is more common in adults and occurs due to the reactivation Reactivation Herpes Simplex Virus 1 and 2 of VZV. The diagnosis is primarily clinical. Management is supportive, although antiviral Antiviral Antivirals for Hepatitis B therapy can be used in certain patient populations. Complications can include secondary bacterial infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, encephalitis Encephalitis Encephalitis is inflammation of the brain parenchyma caused by an infection, usually viral. Encephalitis may present with mild symptoms such as headache, fever, fatigue, and muscle and joint pain or with severe symptoms such as seizures, altered consciousness, and paralysis. Encephalitis, or pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia. Varicella-zoster vaccine Vaccine Suspensions of killed or attenuated microorganisms (bacteria, viruses, fungi, protozoa), antigenic proteins, synthetic constructs, or other bio-molecular derivatives, administered for the prevention, amelioration, or treatment of infectious and other diseases. Vaccination is recommended as a preventive measure in early childhood.
Last updated: Sep 8, 2022
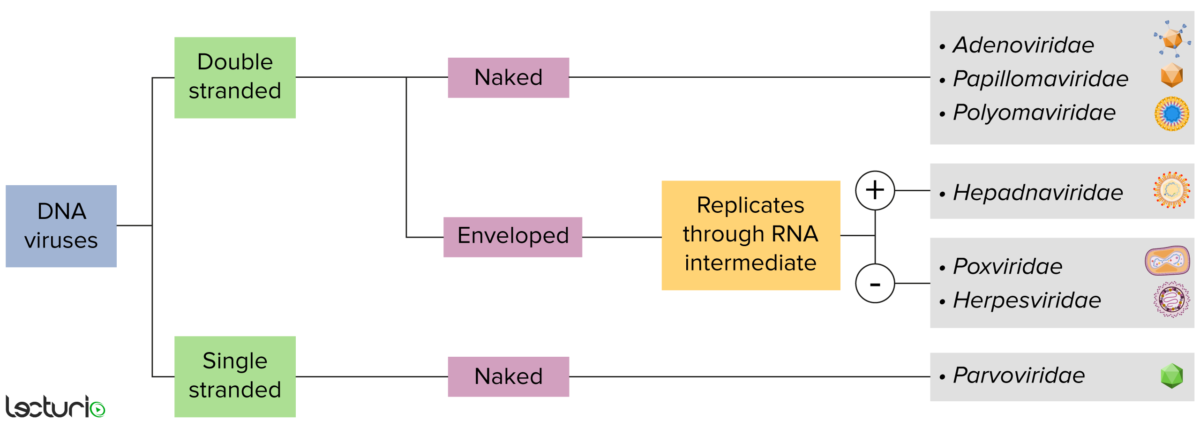
Identification of DNA viruses:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. Viruses with a DNA genome can be further characterized as single or double stranded. “Enveloped” viruses are covered by a thin coat of cell membrane, which is usually taken from the host cell. If the coat is absent, however, the viruses are called “naked” viruses. Some enveloped viruses translate DNA into RNA before incorporating into the genome of the host cell.
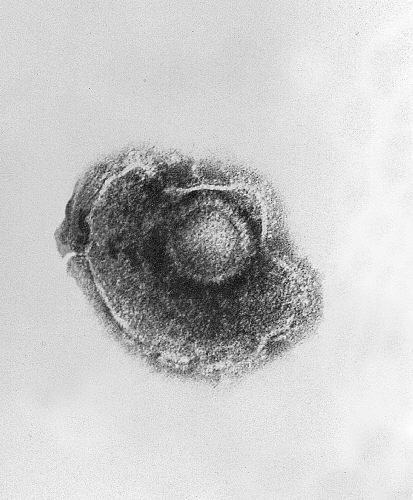
Transmission electron microscopic image showing a single varicella-zoster virus (VZV), also known as human herpesvirus 3, which causes chickenpox
Image: “Ultrastructural features exhibited by a single varicella-zoster virus (VZV), also known as human herpesvirus 3 (HHV-3), the cause of chickenpox.” by CDC. License: Public DomainVaricella-zoster virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology causes 2 distinct syndromes:
Chickenpox:
Shingles:
Humans are the only reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli for VZV.
Infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are highly contagious and the virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology may be transmitted through:
Individuals at higher risk for severe disease and complications:
Primary infection Primary infection Herpes Simplex Virus 1 and 2 (chickenpox):
Secondary infection (shingles):
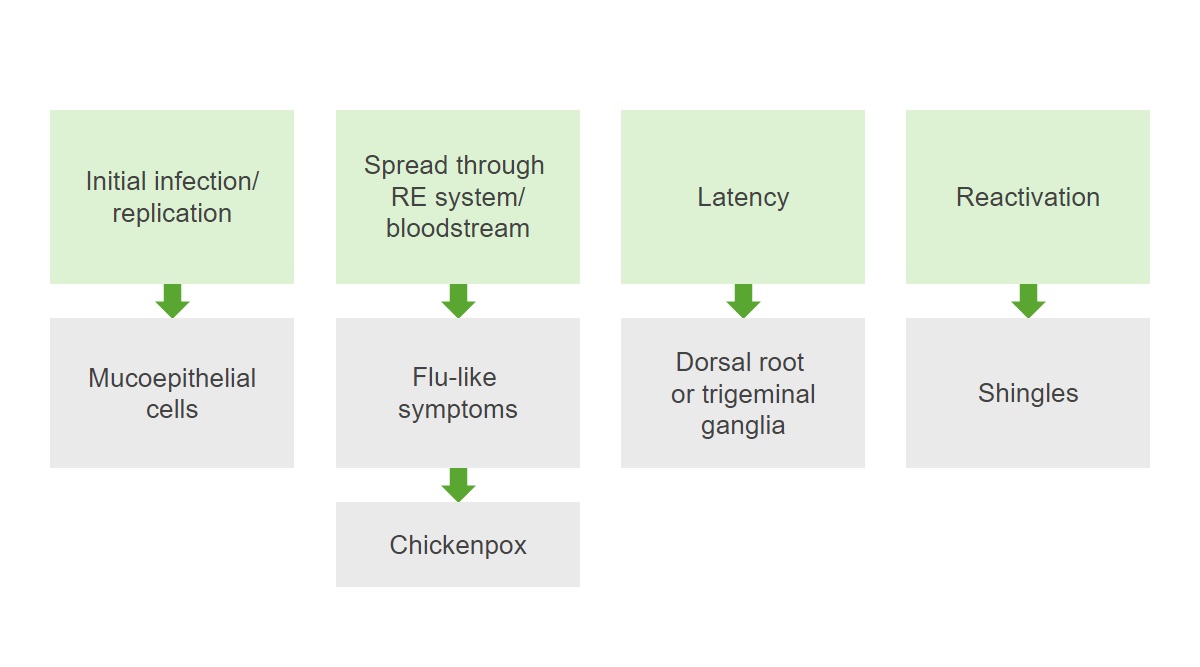
Pathogenesis of varicella-zoster virus (VZV):
Initially, the infection replicates viruses in mucoepithelial cells. The infection spreads throughout the reticuloendothelial (RE) system and bloodstream, causing flu-like symptoms and chickenpox. After resolution of the primary infection, a latency period occurs and the virus remains dormant in the dorsal root ganglia. Reactivation of the infection results in shingles.
The histology of herpes infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease is distinctive.
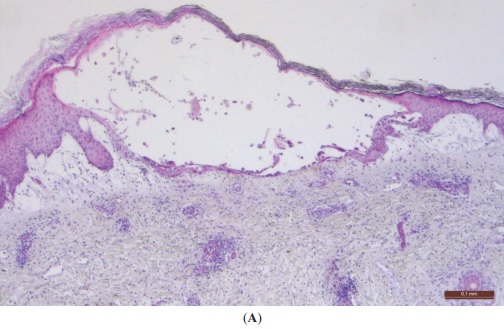
Typical histopathological findings seen with herpetic infections:
A: Skin with intraepidermal vesicle (hematoxylin & eosin, ×40)
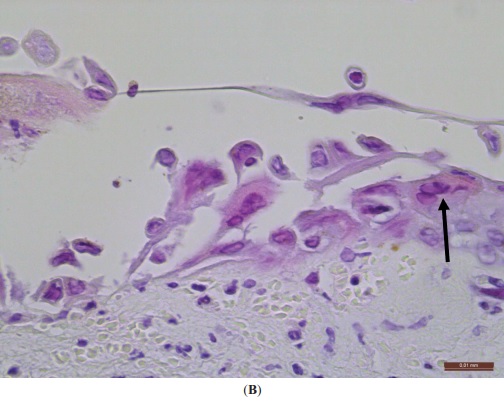
Typical histopathological findings seen with herpetic infections:
B: Ballooning (swelling) degeneration of keratinocytes, and multinucleated cells (H&E, ×400). An arrow points to a multinucleated cell with nuclei containing viral inclusions. Scale bar = 0.1 mm
Chickenpox is caused by a primary infection Primary infection Herpes Simplex Virus 1 and 2 with VZV and has an incubation Incubation The amount time between exposure to an infectious agent and becoming symptomatic. Rabies Virus period of 10‒21 days after exposure.

Classic rash of chickenpox with lesions in different stages of evolution
Image: “10170” by CDC. License: Public Domain
A boy presenting with the characteristic vesicular lesions of chickenpox
Image: “Chicken Pox” by Camilo A. License: Public Domain
A chickenpox rash made up of macules, papules, vesicles, and scabs
Image: “A chickenpox rash made up of macules, papules, vesicles, and scabs” by Jean Jacques Nzeale Noubiap et al. License: CC BY 2.0Shingles is a reactivation Reactivation Herpes Simplex Virus 1 and 2 infection that can occur with increasing age or stress and in immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis individuals.

Shingles rash in the T10‒11 dermatome along a patient’s back
Image: “This view of a patient’s skin, revealed a maculopapular rash, which had been due to an outbreak of shingles.” by CDC. License: Public Domain
Close-up view of the vesicular rash of shingles
Image: “This view of a patient’s skin, revealed a maculopapular rash, which had been due to an outbreak of shingles.” by CDC. License: Public Domain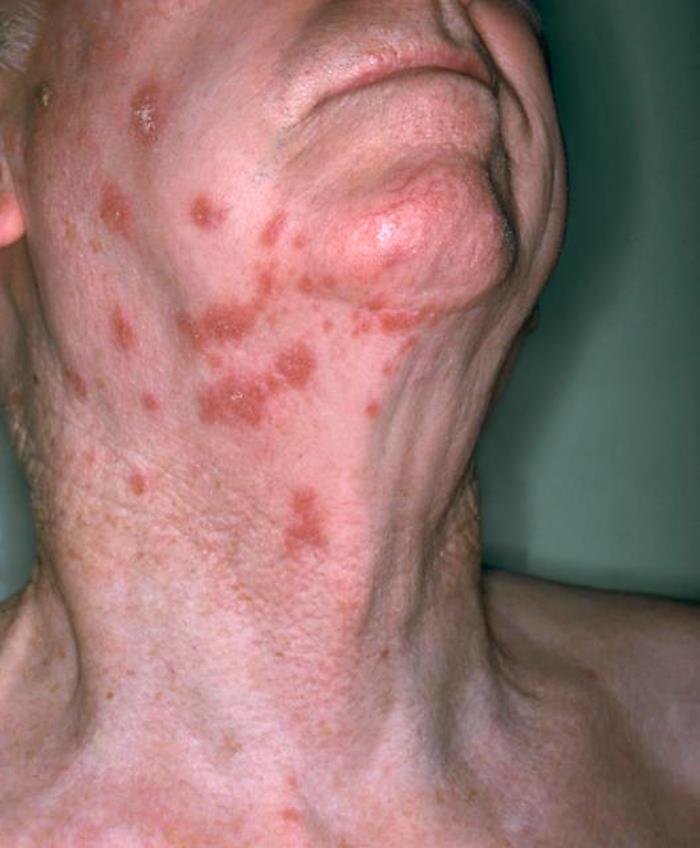
Anterolateral view of a patient’s neck showing the presence of an erythematous rash due to shingles
Image: “Anterolateral view of this patient’s neck showing the presence of an erythematous rash due to shingles” by NIAID. License: Public Domain
Picture of a shingles outbreak on the chest
Image: “Picture of a shingles (herpes zoster) outbreak on the chest” by Preston Hunt. License: CC BY 3.0The diagnosis of chickenpox is most often clinical. The following tests may be used to diagnose patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with atypical presentations:
Supportive care:
Antiviral Antiviral Antivirals for Hepatitis B therapy:
Secondary bacterial skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:
Neurologic complications:
Reye syndrome:
Varicella congenital syndrome (congenital TORCH infection):
Other complications:
The table below compares the 9 herpesviruses considered endemic in humans. There are 115 different total known species of herpesviruses that are grouped into 3 families:
| HHV | Common name | Primary target cells | Latency site | Clinical presentation* |
|---|---|---|---|---|
|
1 (alpha group) |
HSV-1 | Mucoepithelial cells | Dorsal root ganglia |
|
|
2 (alpha group) |
HSV-2 |
|
||
|
3 (alpha group) |
VZV |
|
||
|
4 (gamma group) |
EBV EBV Epstein-barr virus (EBV) is a linear, double-stranded DNA virus belonging to the herpesviridae family. This highly prevalent virus is mostly transmitted through contact with oropharyngeal secretions from an infected individual. The virus can infect epithelial cells and B lymphocytes, where it can undergo lytic replication or latency. Epstein-Barr Virus |
|
Memory Memory Complex mental function having four distinct phases: (1) memorizing or learning, (2) retention, (3) recall, and (4) recognition. Clinically, it is usually subdivided into immediate, recent, and remote memory. Psychiatric Assessment B cells B cells Lymphoid cells concerned with humoral immunity. They are short-lived cells resembling bursa-derived lymphocytes of birds in their production of immunoglobulin upon appropriate stimulation. B cells: Types and Functions |
|
|
5 (beta group) |
CMV |
|
Hematopoietic progenitor cells in bone marrow Bone marrow The soft tissue filling the cavities of bones. Bone marrow exists in two types, yellow and red. Yellow marrow is found in the large cavities of large bones and consists mostly of fat cells and a few primitive blood cells. Red marrow is a hematopoietic tissue and is the site of production of erythrocytes and granular leukocytes. Bone marrow is made up of a framework of connective tissue containing branching fibers with the frame being filled with marrow cells. Bone Marrow: Composition and Hematopoiesis |
|
|
6A, 6B (beta group) |
HHV-6 HHV-6 Human herpesvirus (HHV)-6 and HHV-7 are similar double-stranded DNA viruses belonging to the Herpesviridae family. Human herpesviruses are ubiquitous and infections are commonly contracted during childhood. Human Herpesvirus 6 and 7 | T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions | Monocytes Monocytes Large, phagocytic mononuclear leukocytes produced in the vertebrate bone marrow and released into the blood; contain a large, oval or somewhat indented nucleus surrounded by voluminous cytoplasm and numerous organelles. Innate Immunity: Phagocytes and Antigen Presentation | Roseola |
|
7 (beta group) |
HHV-7 HHV-7 Human herpesvirus (HHV)-6 and HHV-7 are similar double-stranded DNA viruses belonging to the Herpesviridae family. Human herpesviruses are ubiquitous and infections are commonly contracted during childhood. Human Herpesvirus 6 and 7 | T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions | ||
|
8 (gamma group) |
KSHV |
|
B cells B cells Lymphoid cells concerned with humoral immunity. They are short-lived cells resembling bursa-derived lymphocytes of birds in their production of immunoglobulin upon appropriate stimulation. B cells: Types and Functions | Kaposi Kaposi A multicentric, malignant neoplastic vascular proliferation characterized by the development of bluish-red cutaneous nodules, usually on the lower extremities, most often on the toes or feet, and slowly increasing in size and number and spreading to more proximal areas. The tumors have endothelium-lined channels and vascular spaces admixed with variably sized aggregates of spindle-shaped cells, and often remain confined to the skin and subcutaneous tissue, but widespread visceral involvement may occur. Hhv-8 is the suspected cause. There is also a high incidence in AIDS patients. AIDS-defining Conditions sarcoma |