Bullous pemphigoid and pemphigus vulgaris are two different blistering autoimmune diseases Autoimmune diseases Disorders that are characterized by the production of antibodies that react with host tissues or immune effector cells that are autoreactive to endogenous peptides. Selective IgA Deficiency. In bullous pemphigoid, autoantibodies Autoantibodies Antibodies that react with self-antigens (autoantigens) of the organism that produced them. Blotting Techniques attack the hemidesmosomes, which connect epidermal keratinocytes Keratinocytes Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Skin: Structure and Functions to the basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN). This attack results in large, tense subepidermal blisters. In pemphigus vulgaris, autoantibodies Autoantibodies Antibodies that react with self-antigens (autoantigens) of the organism that produced them. Blotting Techniques attack the desmosomal proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis, which connect the keratinocytes Keratinocytes Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Skin: Structure and Functions to one another. This attack results in a more severe, potentially fatal condition with fragile, flaccid blisters, usually with significant mucosal involvement. Diagnosis is made with biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma and IF staining to identify and localize the antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions. Management involves immunosuppression with corticosteroids Corticosteroids Chorioretinitis and other steroid-sparing immunomodulatory agents.
Last updated: May 17, 2024
Bullous pemphigoid:
Pemphigus vulgaris:
| Bullous pemphigoid | Pemphigus vulgaris | |
|---|---|---|
| Incidence Incidence The number of new cases of a given disease during a given period in a specified population. It also is used for the rate at which new events occur in a defined population. It is differentiated from prevalence, which refers to all cases in the population at a given time. Measures of Disease Frequency per year | 6‒13 per 1 million | 0.1‒0.5 per 100,000 |
| Age | > 60 years old | 40‒60 years old |
| Gender Gender Gender Dysphoria predominance | Women = men | Women = men |
| Racial/ethnic bias Bias Epidemiological studies are designed to evaluate a hypothesized relationship between an exposure and an outcome; however, the existence and/or magnitude of these relationships may be erroneously affected by the design and execution of the study itself or by conscious or unconscious errors perpetrated by the investigators or the subjects. These systematic errors are called biases. Types of Biases | None | More common in:
|
| Etiology | None have been proven, but several possible associations:
|
Possible associations:
|
Both bullous pemphigoid and pemphigus vulgaris are autoimmune diseases Autoimmune diseases Disorders that are characterized by the production of antibodies that react with host tissues or immune effector cells that are autoreactive to endogenous peptides. Selective IgA Deficiency that attack anchoring connections of the epidermal keratinocytes Keratinocytes Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Skin: Structure and Functions.
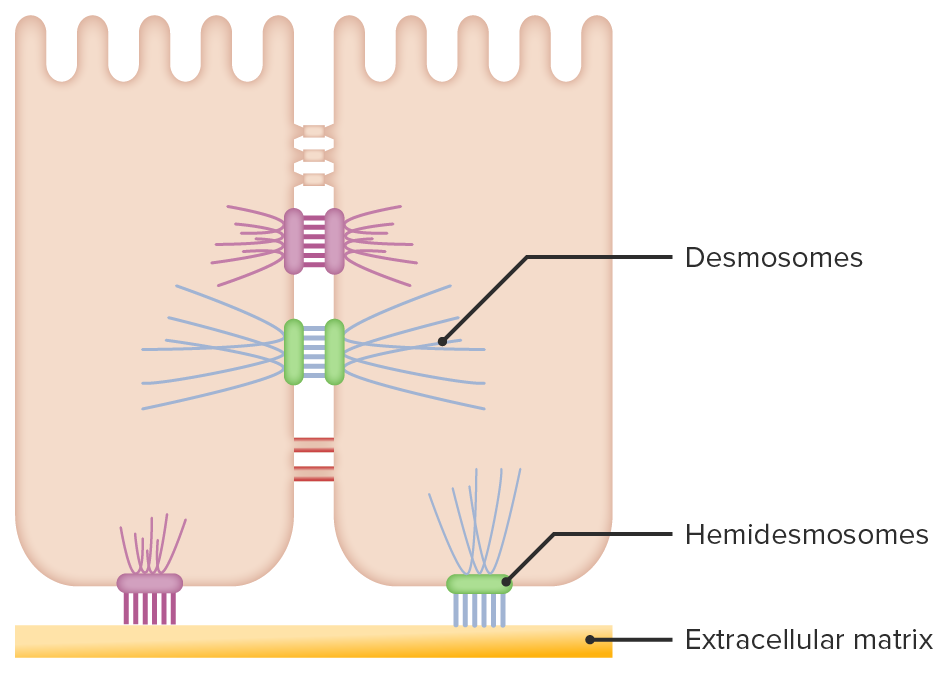
Epidermal keratinocyte connections:
Desmosomes connect keratinocytes to each other, while hemidesmosomes anchor the basal layer of keratinocytes to the basement membrane.
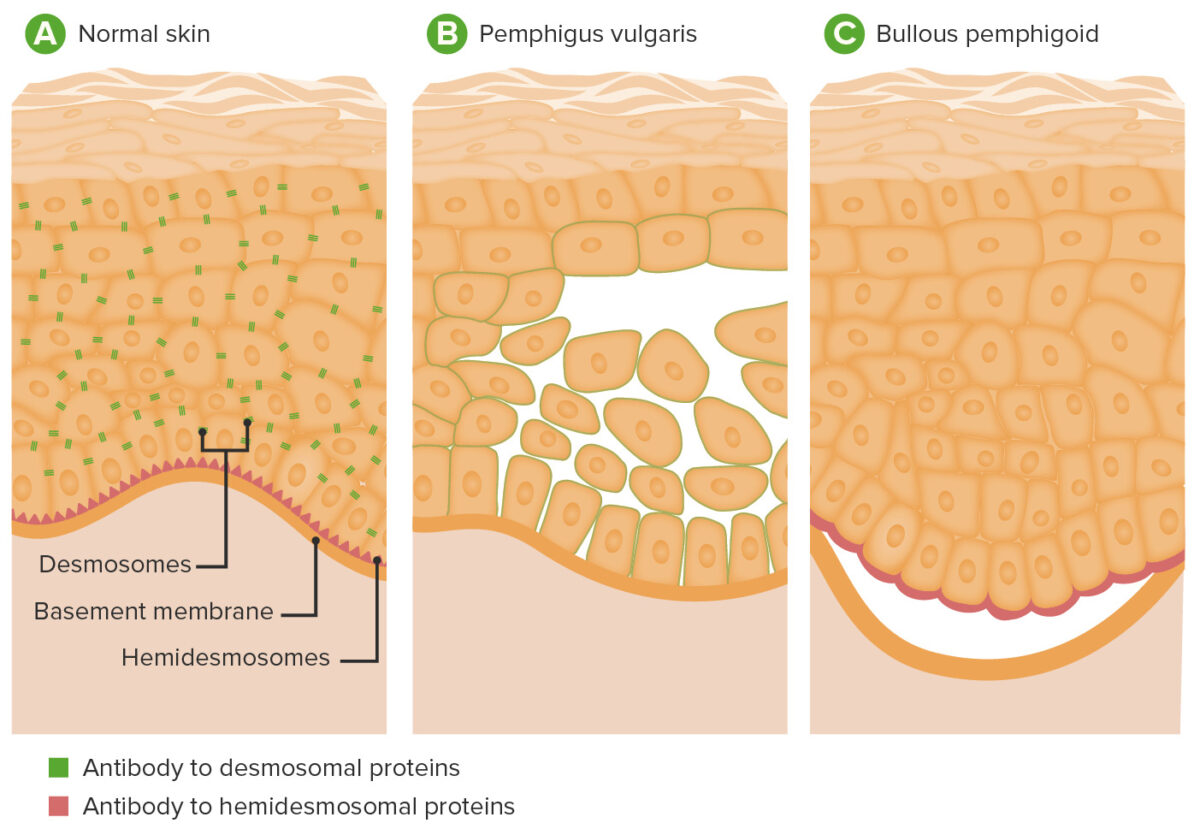
Pathophysiology of pemphigus vulgaris and bullous pemphigoid:
A: Location of desmosomes and hemidesmosomes in epidermis
B: In pemphigus vulgaris, antibodies to desmoglein result in disruption of desmosomes, causing acantholysis and blistering within the epidermis.
C: In bullous pemphigoid, antibodies against hemidesmosomal proteins result in separation of the epidermis from the dermis.

Cutaneous findings in bullous pemphigoid:
Multiple large, tense vesicles and bullae in the groin on normal to mildly erythematous skin

Cutaneous findings in bullous pemphigoid:
Multiple bullae, with some revealing moist erosions after rupture
Pemphigus vulgaris is characterized by bullae Bullae Erythema Multiforme with the following properties:

Cutaneous findings in pemphigus vulgaris
Image: “Pemphigus Vulgaris Ulcer and Hemorrhagic Crust on the Trunk” by Mohsen Masjedi, Ali Asilian, Zabihollah Shahmoradi, Parvin Rajabi Dehnavi, and Bahareh Abtahi Naeini. License: CC BY 3.0, edited by Lecturio.
Mucosal erosion due to pemphigus vulgaris
Image: “Oral Lesions: The Clue to Diagnosis of Pemphigus Vulgaris” by Kuriachan D, Suresh R, Janardhanan M, Savithri V. License: CC BY 3.0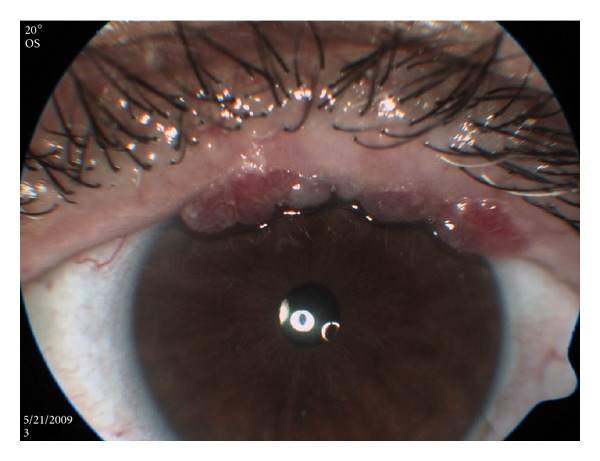
Conjunctival findings in pemphigus vulgaris
Image: “Multiple Conjunctival Papillomas of Eyelid Margins in Pemphigus vulgaris” by Avisar, I., Yassur, I., Kremer, I. License: CC BY 3.0Diagnosis involves checking for a Nikolsky sign Nikolsky Sign Dermatologic Examination, biopsies for routine histopathology and IF, and ELISA ELISA An immunoassay utilizing an antibody labeled with an enzyme marker such as horseradish peroxidase. While either the enzyme or the antibody is bound to an immunosorbent substrate, they both retain their biologic activity; the change in enzyme activity as a result of the enzyme-antibody-antigen reaction is proportional to the concentration of the antigen and can be measured spectrophotometrically or with the naked eye. Many variations of the method have been developed. St. Louis Encephalitis Virus testing.
| Test | Bullous pemphigoid | Pemphigus vulgaris |
|---|---|---|
| Nikolsky’s sign | Negative | Positive |
| H&E staining |
|
|
| IF | Linear staining along the basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN) | Staining within the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions in a reticular (net-like) pattern |
| ELISA ELISA An immunoassay utilizing an antibody labeled with an enzyme marker such as horseradish peroxidase. While either the enzyme or the antibody is bound to an immunosorbent substrate, they both retain their biologic activity; the change in enzyme activity as a result of the enzyme-antibody-antigen reaction is proportional to the concentration of the antigen and can be measured spectrophotometrically or with the naked eye. Many variations of the method have been developed. St. Louis Encephalitis Virus | Autoantibodies Autoantibodies Antibodies that react with self-antigens (autoantigens) of the organism that produced them. Blotting Techniques against bullous pemphigoid antigens BP180 and BP230 | Autoantibodies Autoantibodies Antibodies that react with self-antigens (autoantigens) of the organism that produced them. Blotting Techniques against DSG-1 and DSG-3 |
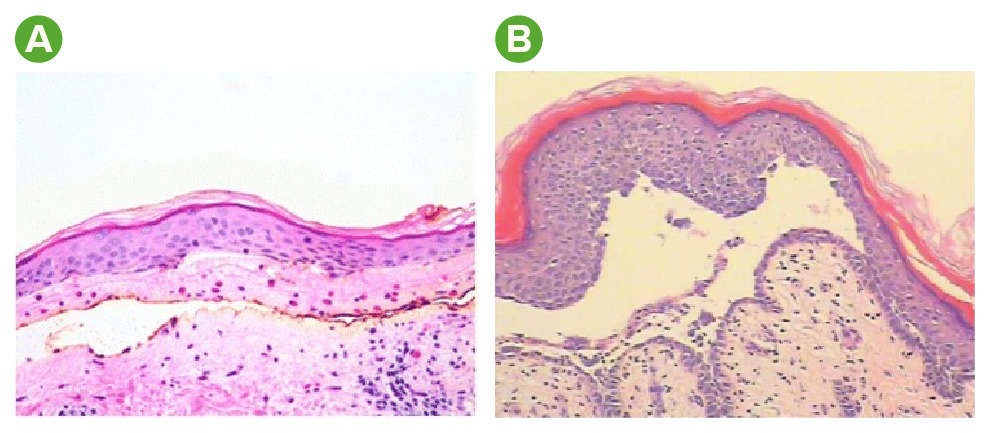
Histology findings in bullous pemphigoid and pemphigus vulgaris:
A: H&E staining in bullous pemphigoid reveals a subepidermal bulla and numerous eosinophils.
B: H&E staining in pemphigus vulgaris reveals a suprabasal acantholytic blister. Note the row-of-tombstone appearance (a layer of keratinocytes still attached to the basement membrane).
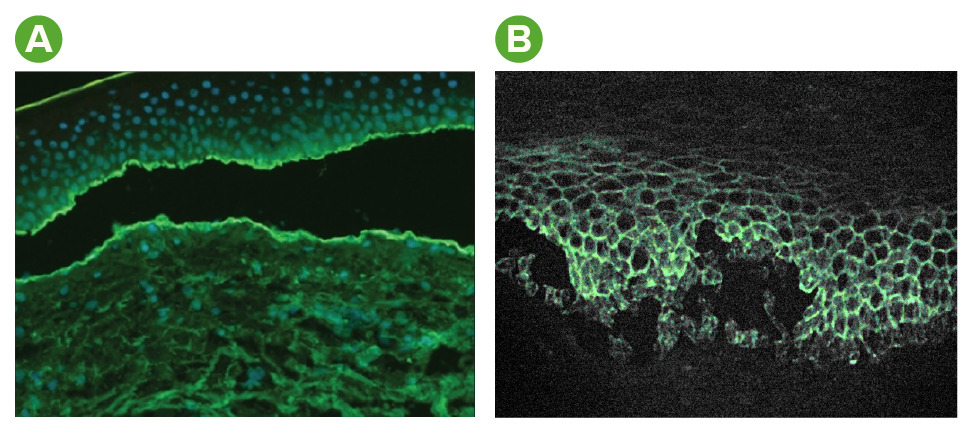
Immunofluorescence findings in bullous pemphigoid and pemphigus vulgaris:
A: In bullous pemphigoid, staining of complement and antibodies occurs at the dermal–epidermal junction.
B: In pemphigus vulgaris, staining of antibodies occurs within the epidermis in a reticular (net-like) pattern.
The goal of therapy for both bullous pemphigoid and pemphigus vulgaris is to decrease autoantibody production while minimizing drug-induced side effects.