Genitourinary examination is an integral part of the male physical examination that provides important information on the normal development in infants and children. Genitourinary examination is used for preventative health exams in adult men and is also a part of problem-focused exams performed to evaluate complaints such as pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, infection, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions, or lumps in the genital or inguinal areas. In subjects with urologic emergencies, such as testicular torsion Testicular torsion Testicular torsion is the sudden rotation of the testicle, specifically the spermatic cord, around its axis in the inguinal canal or below. The acute rotation results in compromised blood flow to and from the testicle, which puts the testicle at risk for necrosis. Testicular Torsion, an accurate exam leading to prompt treatment can be the defining factor in maintaining fertility. Other significant conditions found on the genitourinary exam are STIs STIs Sexually transmitted infections (STIs) or sexually transmitted diseases (STDs) are infections that spread either by vaginal intercourse, anal sex, or oral sex. Symptoms and signs may include vaginal discharge, penile discharge, dysuria, skin lesions (e.g., warts, ulcers) on or around the genitals, and pelvic pain. Some infections can lead to infertility and chronic debilitating disease. Sexually Transmitted Infections (STIs), Peyronie disease Peyronie Disease Penile Anomalies and Conditions, and masses that may need further evaluation to confirm malignancy Malignancy Hemothorax.
Last updated: Apr 20, 2023
Components of the external male genitourinary exam include the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions of the penis Penis The penis is the male organ of copulation and micturition. The organ is composed of a root, body, and glans. The root is attached to the pubic bone by the crura penis. The body consists of the 2 parallel corpora cavernosa and the corpus spongiosum. The glans is ensheathed by the prepuce or foreskin. Penis: Anatomy, urethral orifice, scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy, and inguinal area (groin).
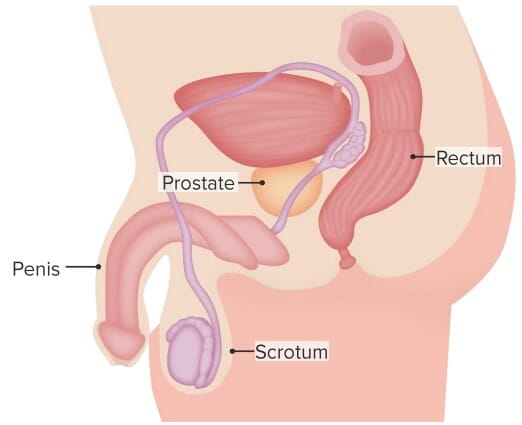
Sagittal view of the male pelvis, identifying the main reproductive structures and the rectum
Image by Lecturio.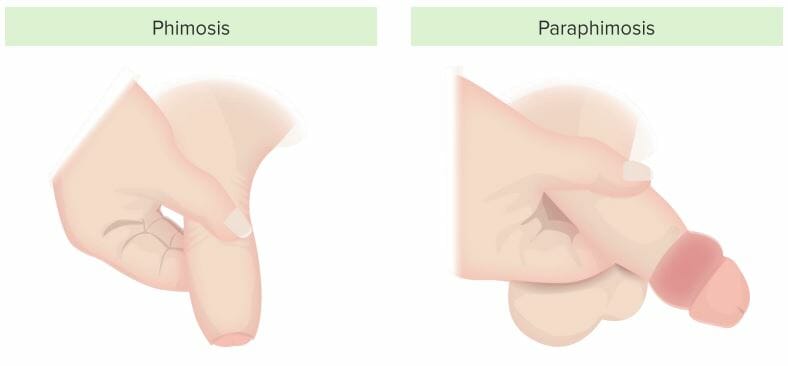
Illustrations of phimosis (left) and paraphimosis (right)
Image by Lecturio.
Examination of the urethral meatus
Image by Lecturio.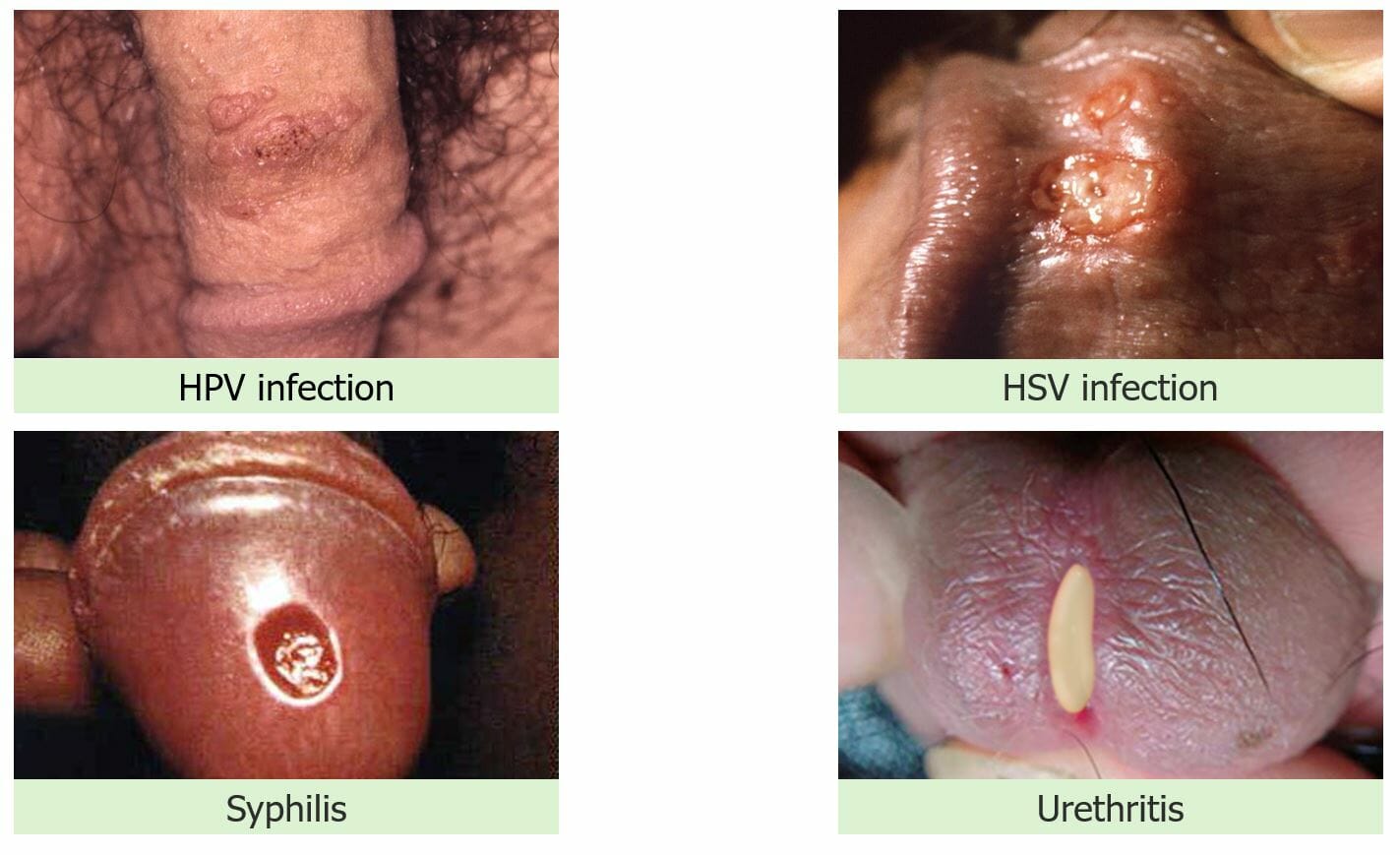
Physical examination findings with STIs:
Upper left:
genital warts
Upper right: vesicles with
genital herpes
Lower left: ulcer/chancre with
syphilis
Lower right: purulent discharge with urethritis from
gonorrhea
or
chlamydia
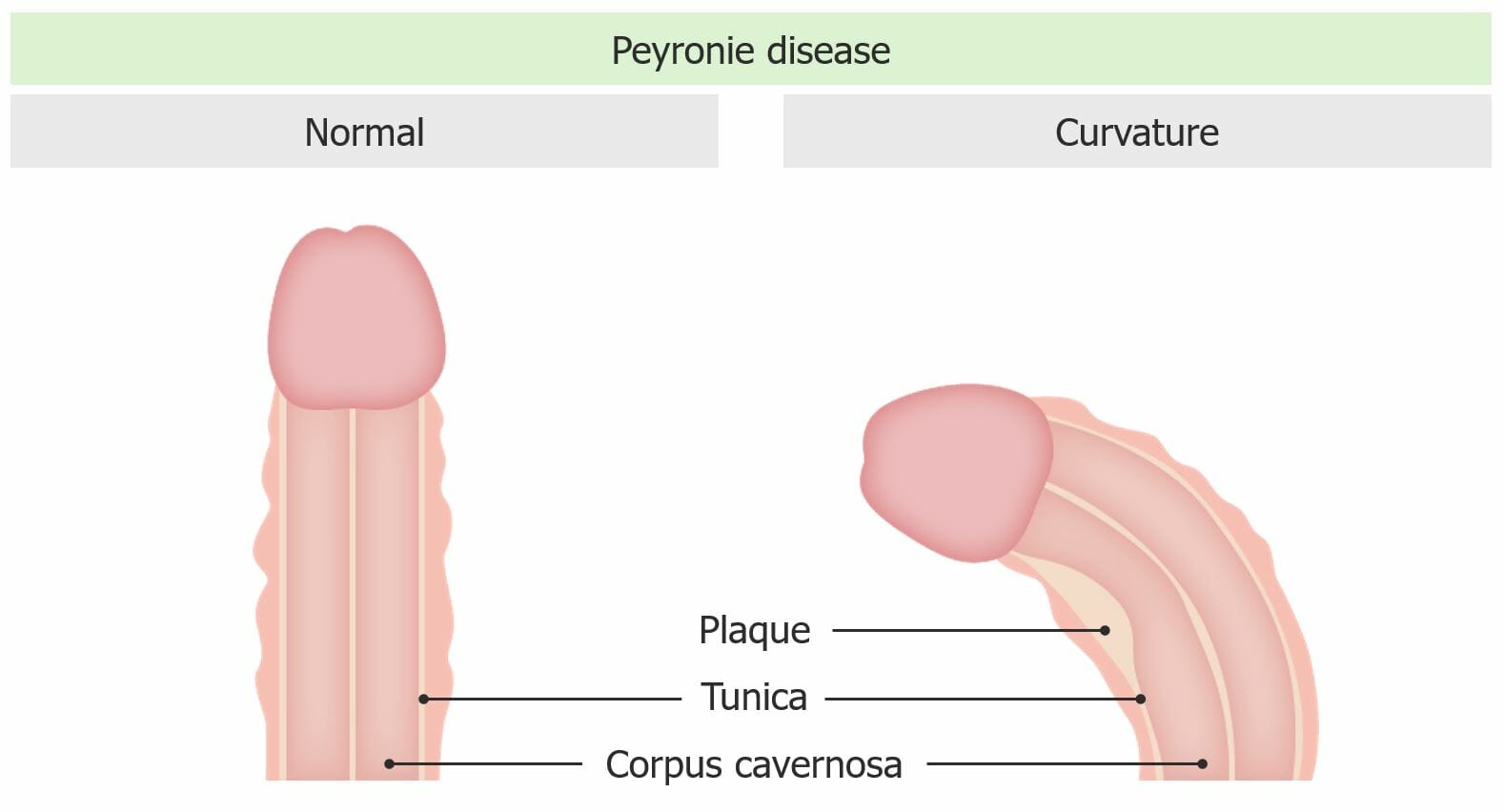
Left: normal penis anatomy
Right: Abnormal curvature is seen with Peyronie disease.
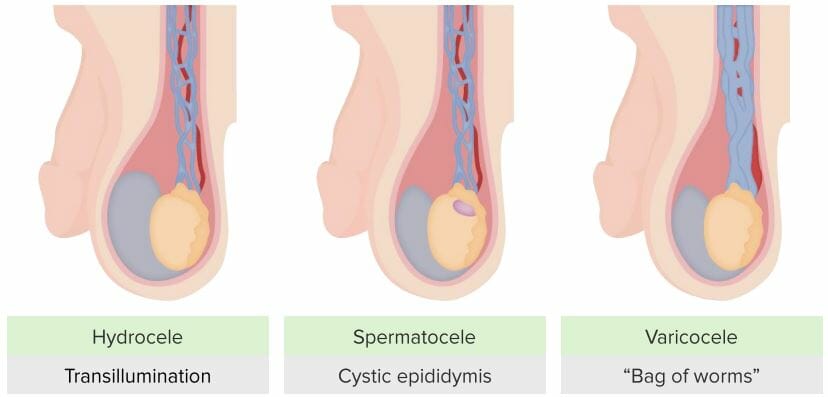
Causes of scrotal enlargement
Image by Lecturio.
Palpation of the inguinal ring during an exam to check for a hernia
Image by Lecturio.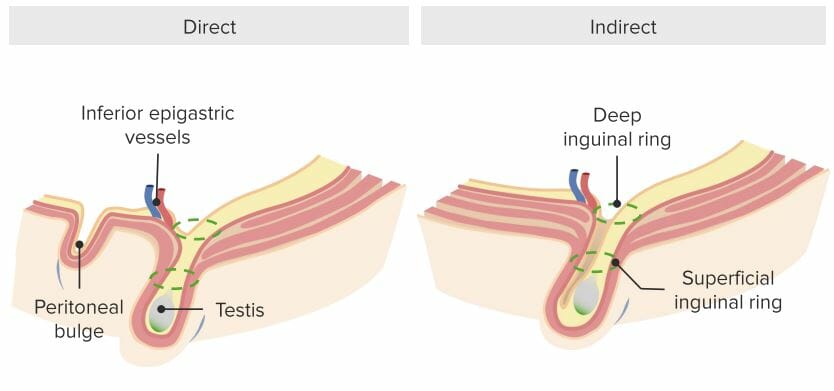
Illustrations of an inguinal hernia. Note the protrusion of the peritoneal cavity into the scrotum through the deep inguinal ring.
Image by Lecturio.The rectal examination is controversial with regard to screening Screening Preoperative Care benefits and is no longer recommended by some guidelines; however, it is helpful for individuals with urinary or rectal complaints.

Inspection of the anal orifice: Notice that the examiner retracts the buttocks with the back of the hand.
Image by Lecturio.
Digital rectal exam of the prostate gland
Image by Lecturio.