Hemorrhoids are normal vascular cushions in the anal canal composed of dilated vascular tissue, smooth muscle, and connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology. They do not cause issues unless they are enlarged, inflamed, thrombosed, or prolapsed. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship often present with rectal bleeding of bright red blood, or they may have pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, perianal pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema), or a palpable mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast. Risk factors include family history Family History Adult Health Maintenance, low-fiber diet, and constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation. The two main types of hemorrhoids are external, usually with perianal pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, and internal, which are usually painless. The main diagnostic tools are history, physical exam, and endoscopic procedures if indicated for further investigation. If symptoms are acute, excision can be performed for external hemorrhoids. Otherwise, conservative management is recommended. Surgical methods are reserved for more severe hemorrhoids or those unresponsive to primary treatment.
Last updated: Jan 16, 2024
Hemorrhoids are normal swollen vascular structures in the anorectal canal.
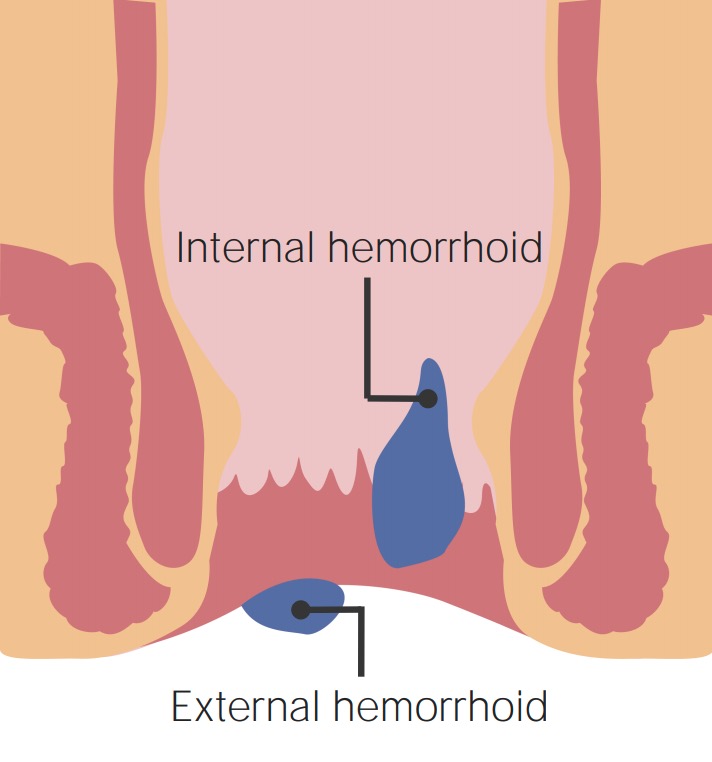
Depiction of internal hemorrhoids above the dentate line and external hemorrhoid, likely causing pain, below the dentate line
Image: “Anus with hemorrhoids” by Bruce Blaus. License: CC BY 3.0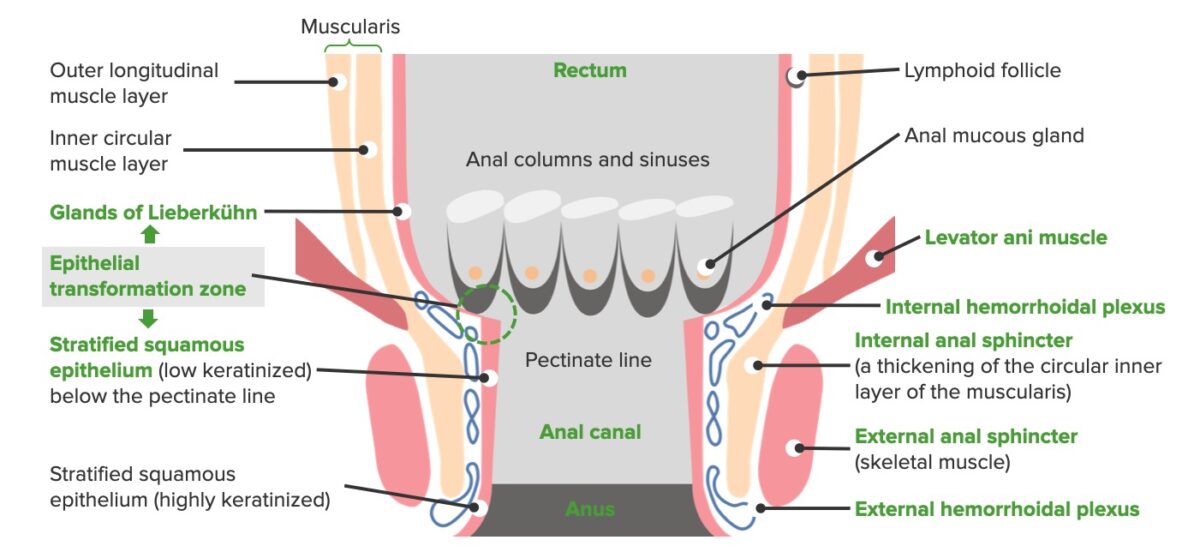
Anatomy of the anal canal:
The image shows the pectinate (dentate) line, which marks the area separating the origination of external (below the dentate line) and internal (above the dentate line) hemorrhoids.

Thrombosed external hemorrhoid with skin tag
Image: “Thrombosed external haemorrhoid” by Rohde et al. License: CC BY 2.0
Thrombosed external hemorrhoid with prolapsing internal hemorrhoid
Image: “Circular perianal thrombosis” by Rohde et al. License: CC BY 2.0The following procedures are for grades I and II internal hemorrhoids that do not respond to conservative management.
Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation:
Hemorrhoidectomy:
Other options: