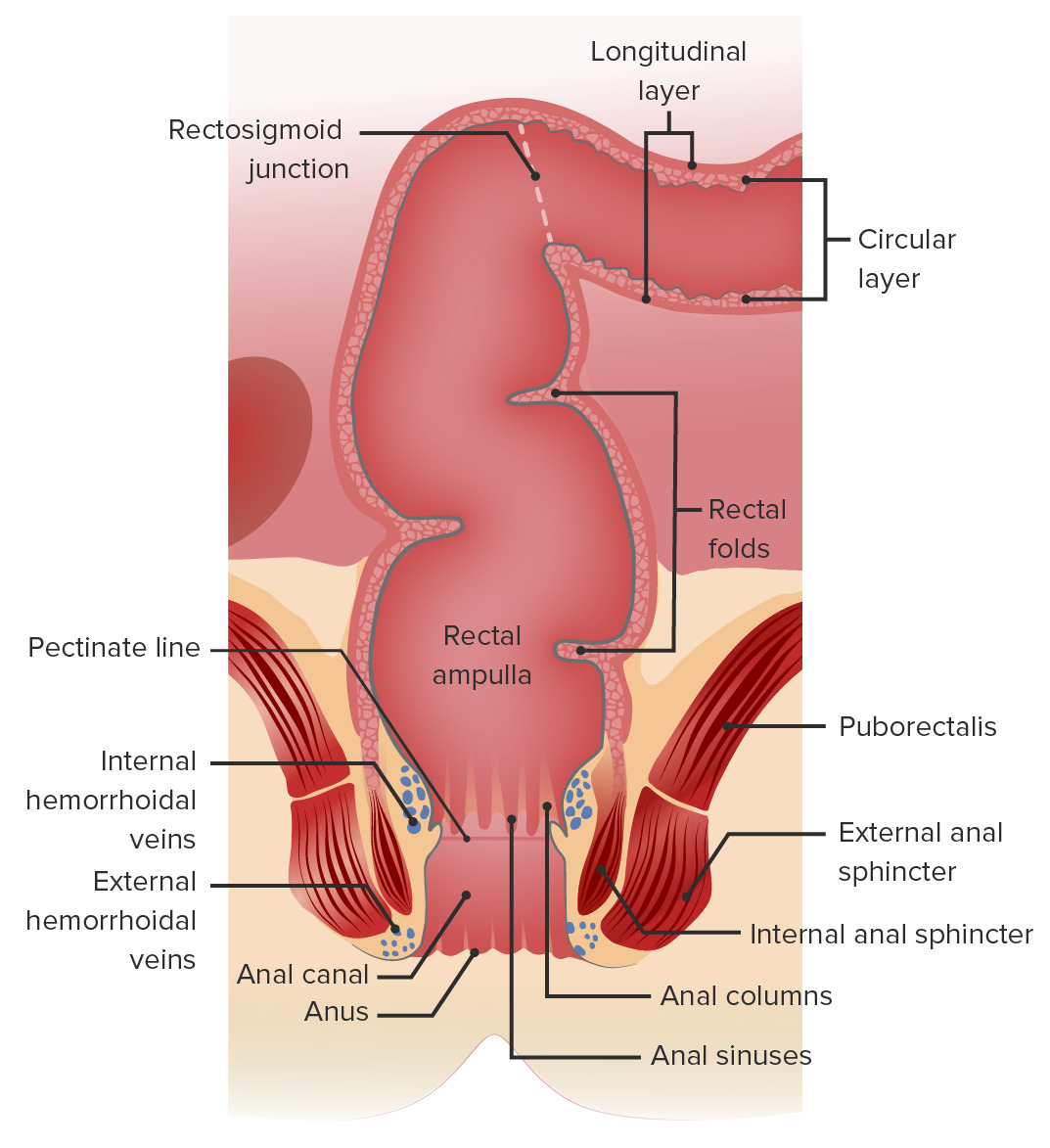
The rectum and anal canal are the most terminal parts of the lower GI tract/ large intestine Large intestine The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy that form a functional unit and control defecation Defecation The normal process of elimination of fecal material from the rectum. Gastrointestinal Motility. Fecal incontinence Fecal incontinence Failure of voluntary control of the anal sphincters, with involuntary passage of feces and flatus. Pediatric Constipation can occur if this function is disturbed. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis Puborectalis Vagina, Vulva, and Pelvic Floor: Anatomy muscle, and internal and external anal sphincters. Peristaltic waves within the rectal muscularis, involuntary relaxation of the internal anal sphincter (controlled by the ANS ANS The ans is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ans consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy), and voluntary relaxation of the external anal sphincter (controlled by the cerebral cortex Cerebral cortex The cerebral cortex is the largest and most developed part of the human brain and CNS. Occupying the upper part of the cranial cavity, the cerebral cortex has 4 lobes and is divided into 2 hemispheres that are joined centrally by the corpus callosum. Cerebral Cortex: Anatomy) are essential for defecation Defecation The normal process of elimination of fecal material from the rectum. Gastrointestinal Motility to occur. The rich plexus of veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology surrounding the anal canal can develop into hemorrhoids Hemorrhoids Hemorrhoids are normal vascular cushions in the anal canal composed of dilated vascular tissue, smooth muscle, and connective tissue. They do not cause issues unless they are enlarged, inflamed, thrombosed, or prolapsed. Patients often present with rectal bleeding of bright red blood, or they may have pain, perianal pruritus, or a palpable mass. Hemorrhoids if dilated.
Last updated: Nov 19, 2024
Gross anatomy of the rectum and anal canal
Image by Lecturio.The rectum is the most posterior visceral organ in the pelvic cavity.
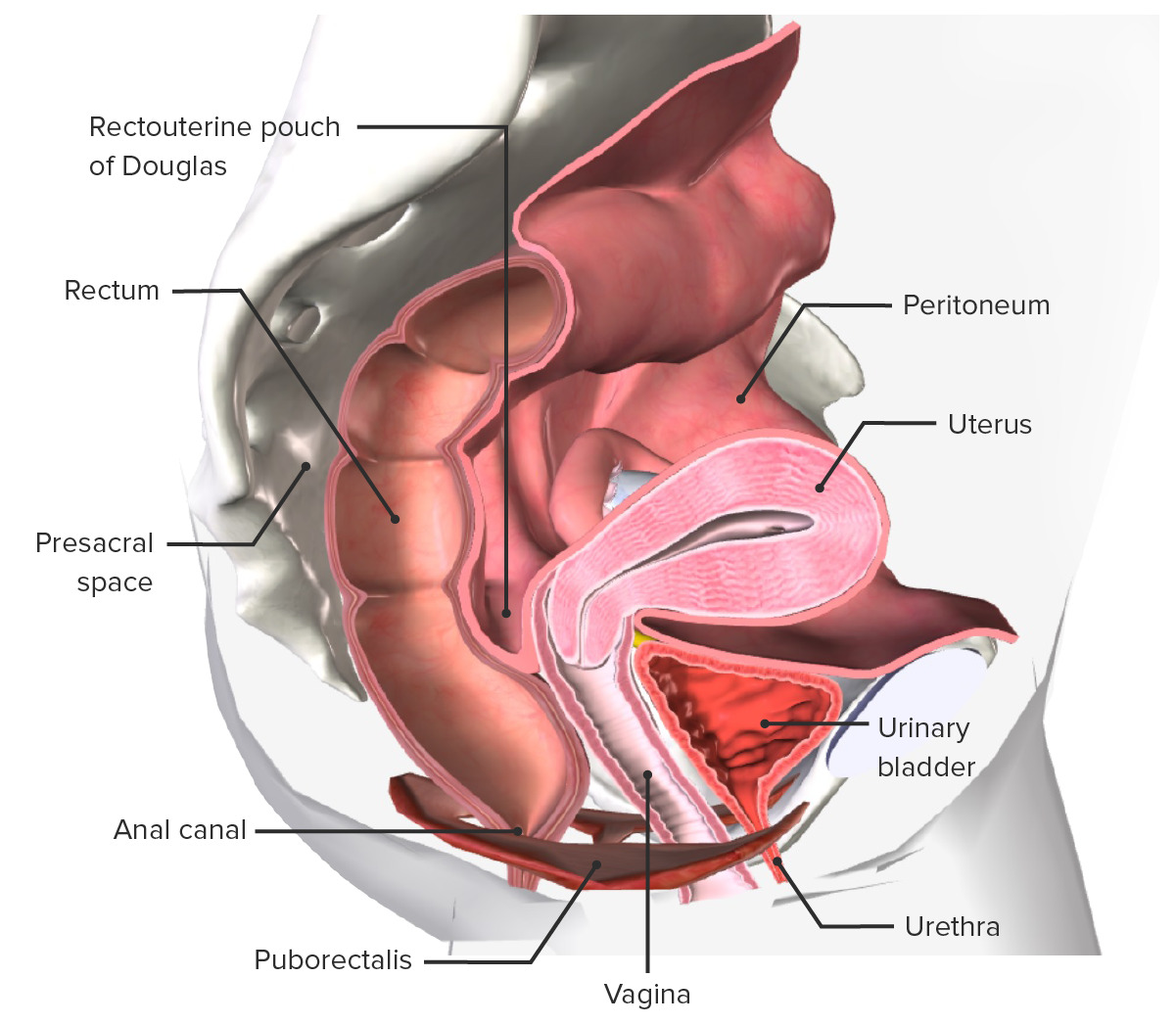
Anatomy of the internal female pelvis
Image by BioDigital, edited by Lecturio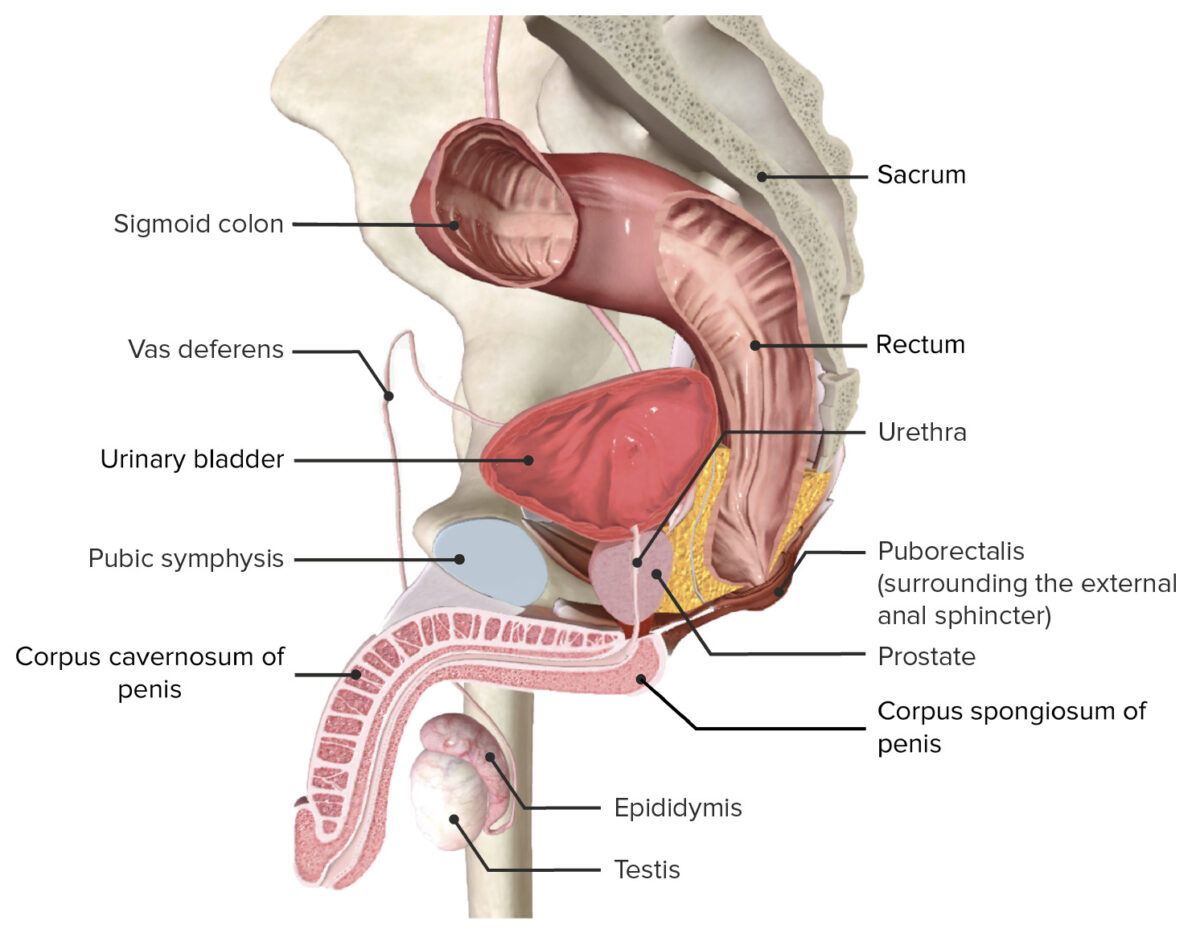
Anatomy of the internal male pelvis
Image by BioDigital, edited by LecturioSimilar to other segments of the GI tract, the layers of the anorectal wall (from the inner lumen outward) are mucosa → submucosa → muscular layer → serosa. There are no villi or circular folds Circular folds Small Intestine: Anatomy in the anorectal wall like those in the small intestine Small intestine The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy.
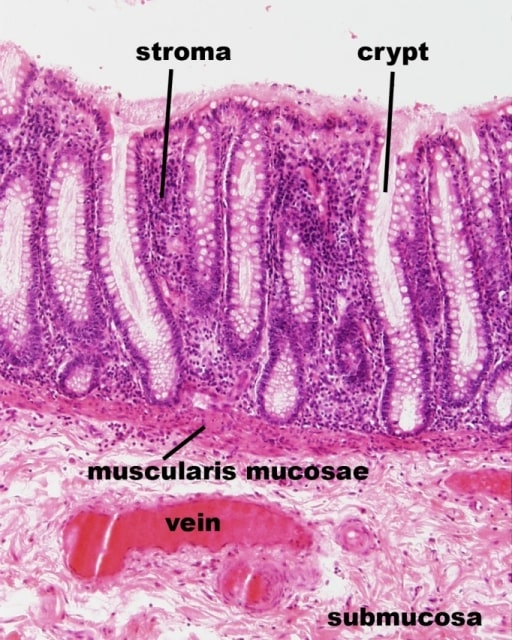
Histological image of the rectal mucosa (longitudinal section):
Rectal crypts with simple columnar epithelium are visible and the stroma (lamina propria) is seen wrapping around the crypts.
Made up of 2 layers of smooth muscle:
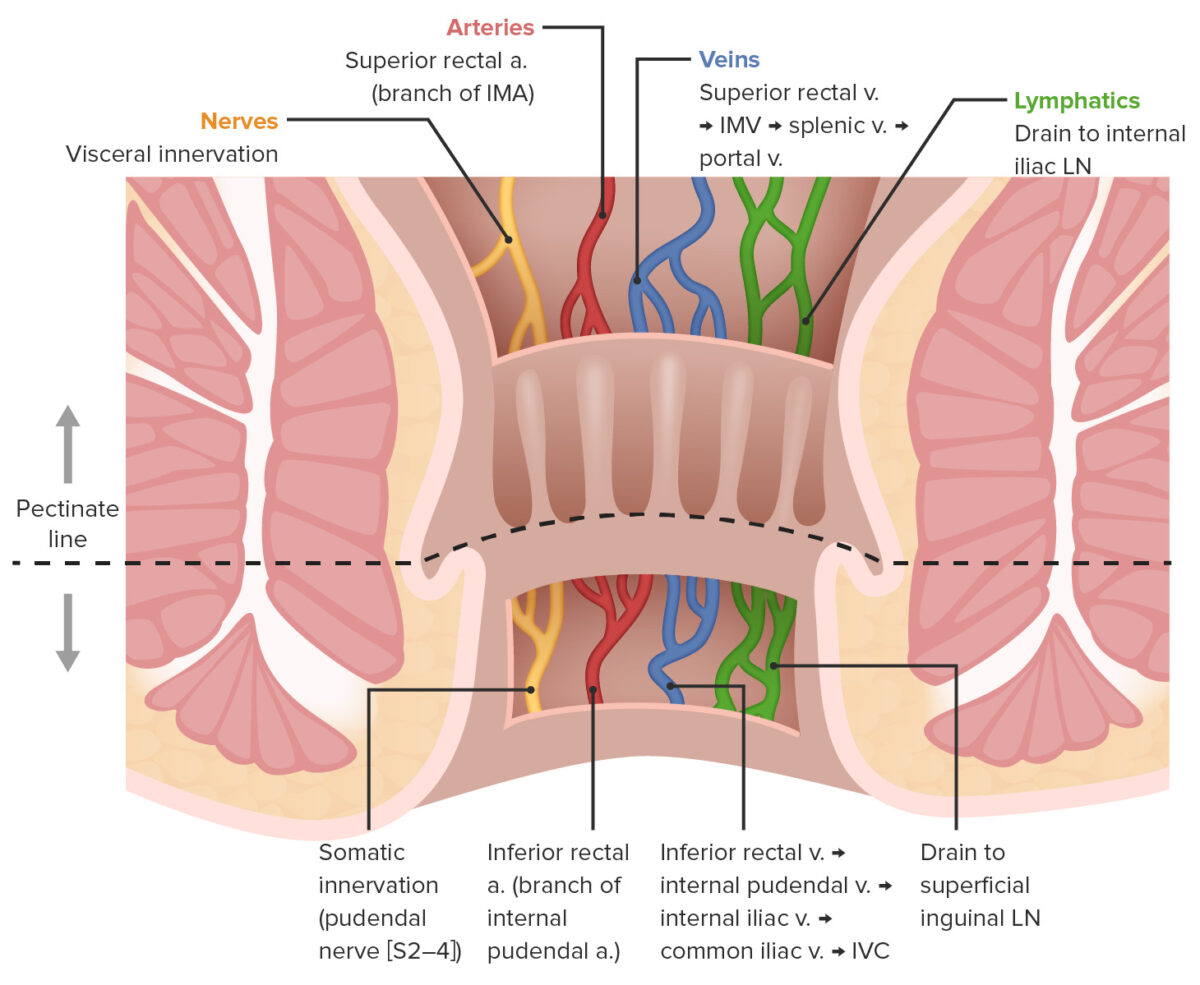
Differences in anal neurovasculature above and below the pectinate line:
IMA: inferior mesenteric artery
IMV: inferior mesenteric vein
LN: lymph node
IVC: inferior vena cava
The primary roles of the rectum and anal canal involve controlled defecation Defecation The normal process of elimination of fecal material from the rectum. Gastrointestinal Motility.
The rectum contains stretch receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors that stimulate the defecation reflex Defecation reflex Gastrointestinal Motility when the rectum begins to fill with feces.
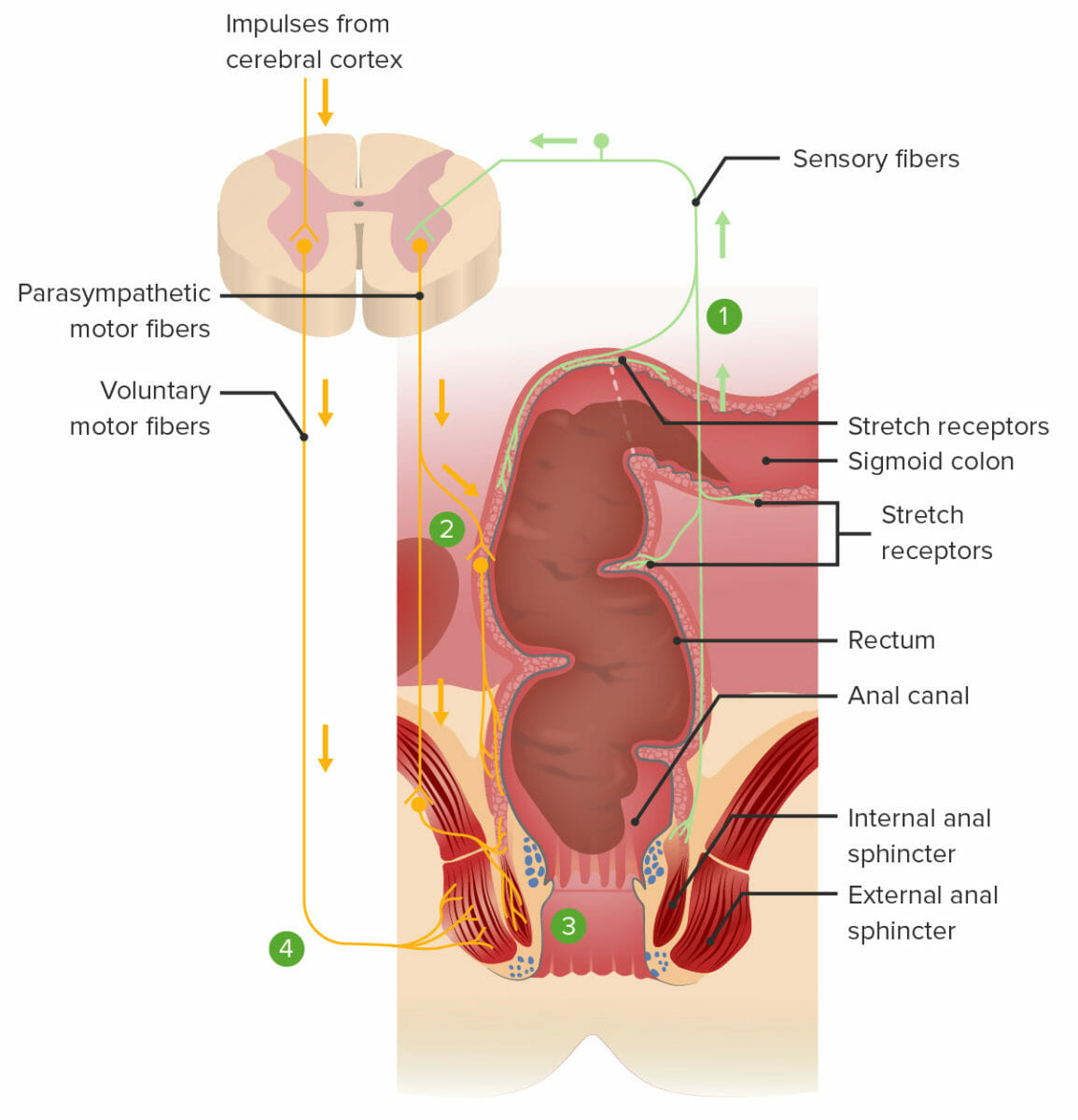
Defecation reflex:
1. Feces stretch the rectum and stimulate the stretch receptors, transmitting the signal to the spinal cord.
2. A spinal reflex sends parasympathetic motor signals to the myenteric nerve plexus, resulting in contraction of the smooth muscles within the rectum, pushing feces downward.
3. The same spinal reflex also sends parasympathetic motor signals to relax the internal anal sphincter.
4. Voluntary impulses from the brain prevent defecation by keeping the external anal sphincter contracted. Defecation will occur if voluntary signals allow the external anal sphincter to relax.