Chronic venous disease is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension. "Chronic venous insufficiency" refers to the more severe forms of chronic venous disease. Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions changes typically distinguish chronic venous insufficiency from milder forms of venous disease (like varicose veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology) and include skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions pigmentation, stasis dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema), lipodermatosclerosis, and eventually, the development of ulcers. Diagnosis is usually based on physical exam findings alone, although venous duplex ultrasonography Duplex ultrasonography Ultrasonography applying the doppler effect combined with real-time imaging. The real-time image is created by rapid movement of the ultrasound beam. A powerful advantage of this technique is the ability to estimate the velocity of flow from the doppler shift frequency. Hypercoagulable States can provide additional information about the etiology, location, and extent of disease. The mainstay of management is compression Compression Blunt Chest Trauma therapy. A variety of surgical options also exist for symptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship, including ablation, sclerotherapy Sclerotherapy Treatment of varicose veins, hemorrhoids, gastric and esophageal varices, and peptic ulcer hemorrhage by injection or infusion of chemical agents which cause localized thrombosis and eventual fibrosis and obliteration of the vessels. Hemorrhoids, and valve repair. Venous ulcers are common as the disease progresses and are often very difficult to treat.
Last updated: Jan 11, 2023
Chronic venous disease is a spectrum of disorders characterized by venous dilation and/or abnormal vein function in the lower extremities resulting from venous hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension.
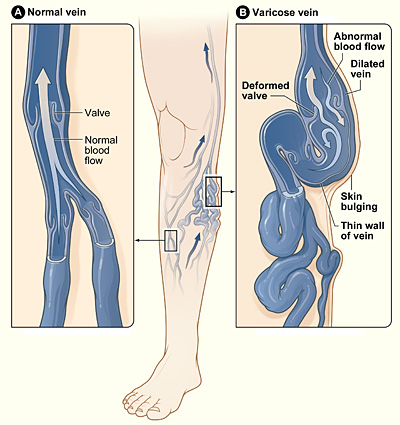
Varicose veins
Image: “Varicose veins” by National Heart Lung and Blood Institute. License: Public Domain
Irregular, nonhealing venous stasis ulcer on the lower leg and ankle, with unhealthy granulation tissue:
There is also surrounding lipodermatosclerosis, stasis dermatitis, and brown skin pigmentation, all characteristic of chronic venous insufficiency.

Stasis dermatitis
Image: “Stasis dermatitis” by Cardiologist61. License: Public DomainLower extremity appearance:
Venous refilling time:
Ankle–brachial index:
Duplex ultrasonography Duplex ultrasonography Ultrasonography applying the doppler effect combined with real-time imaging. The real-time image is created by rapid movement of the ultrasound beam. A powerful advantage of this technique is the ability to estimate the velocity of flow from the doppler shift frequency. Hypercoagulable States:
Cross-sectional venography Venography Budd-Chiari Syndrome with CT or MRI:
Catheter-based (invasive) venography Venography Budd-Chiari Syndrome:
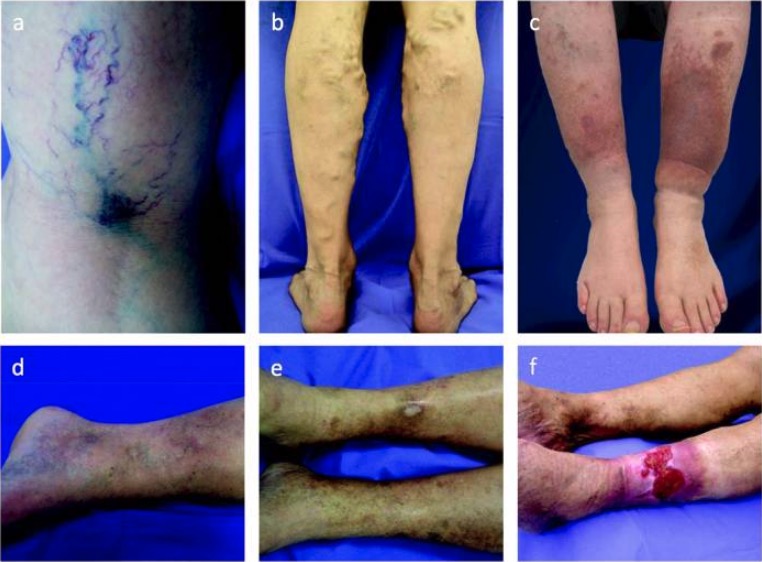
Spectrum of chronic venous disease:
Extent of disease can be classified from C1 to C6 on the basis of the following manifestations:
a: spider and reticular veins (C1)
b: varicose veins (C2)
c: edema and skin pigmentation (C4)
d: lipodermatosclerosis (C4)
e: healed ulcer (C5)
f: active venous ulcer (C6)
Goals:
Options include: