Spinal stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) is the progressive narrowing of the central spinal canal Spinal Canal The cavity within the spinal column through which the spinal cord passes. Spinal Cord Injuries, intervertebral foramen, and lateral recess, leading to compression Compression Blunt Chest Trauma of the nerve root. Spinal stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) can occur in the cervical, thoracic, and lumbar spine Spine The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy and is commonly caused by degenerative bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types disease (mostly affecting the elderly). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, weakness, numbness, and tingling Tingling Posterior Cord Syndrome in the neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess or lower back, which may radiate to the legs and buttocks. Clinical examination shows symptom improvement with spinal flexion Flexion Examination of the Upper Limbs and symptom deterioration with spinal extension Extension Examination of the Upper Limbs. The diagnosis is confirmed with MRI. Conservative management includes analgesic/antiinflammatory medications and physiotherapy. Decompression surgery Decompression surgery A surgical operation for the relief of pressure in a body compartment or on a body part. Cranial Nerve Palsies ( laminectomy Laminectomy A surgical procedure that entails removing all (laminectomy) or part (laminotomy) of selected vertebral lamina to relieve pressure on the spinal cord and/or spinal nerve roots. Vertebral lamina is the thin flattened posterior wall of vertebral arch that forms the vertebral foramen through which pass the spinal cord and nerve roots. Neurosurgery) is considered in advanced cases, or if conservative management fails.
Last updated: May 21, 2025
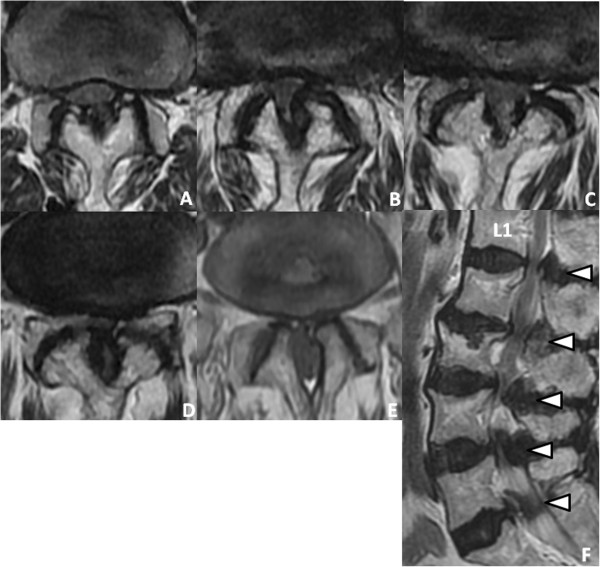
Magnetic resonance imaging (MRI) showing extensive spinal stenosis:
(A): L1–L2
(B): L2–L3
(C): L3–L4
(D): L4–L5
(E): L5–S1
(F): Sagittal T2-weighted image reveals stenosis from L1–L2 through L5–S1 (arrowheads).
The goal of spinal stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) management is to reduce symptoms and increase the individual’s functional status.
Conservative management:
Surgery: