Anterior cord syndrome (ACS) is an incomplete cord syndrome predominantly affecting the anterior (ventral) ⅔ of the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy while sparing the dorsal columns Dorsal Columns Posterior Cord Syndrome. Anterior cord syndrome can be caused by occlusion of the anterior spinal artery or by trauma, which results in disk herniation Herniation Omphalocele and bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types fragments disrupting the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy. Clinical manifestations include loss of both motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology and sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology function below the level of injury. Diagnosis of ACS is by clinical exam and neuroimaging Neuroimaging Non-invasive methods of visualizing the central nervous system, especially the brain, by various imaging modalities. Febrile Infant with MRI. Management is directed at resolving the underlying cause. Preservation of motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology function is a priority, but the prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is poor.
Last updated: Mar 29, 2023
Anterior cord syndrome (ACS) is an incomplete cord syndrome affecting the anterior ⅔ of the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy while sparing the dorsal columns Dorsal Columns Posterior Cord Syndrome, resulting in loss of motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology and sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology function below the level of injury.
Anterior cord syndrome starts with occlusion of the blood supply or injury to the vertebral column Vertebral column The human spine, or vertebral column, is the most important anatomical and functional axis of the human body. It consists of 7 cervical vertebrae, 12 thoracic vertebrae, and 5 lumbar vertebrae and is limited cranially by the skull and caudally by the sacrum. Vertebral Column: Anatomy. The syndrome is infrequently due to spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy tumors.
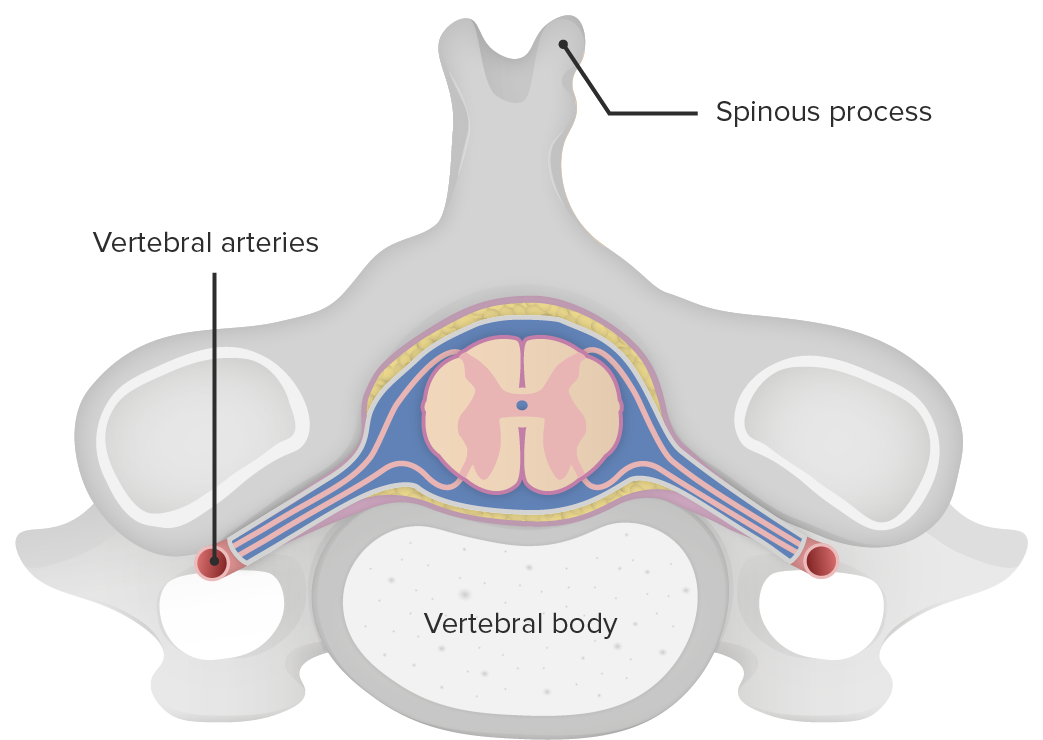
Cross section of the spinal cord in relation to the vertebral body
Image by Lecturio.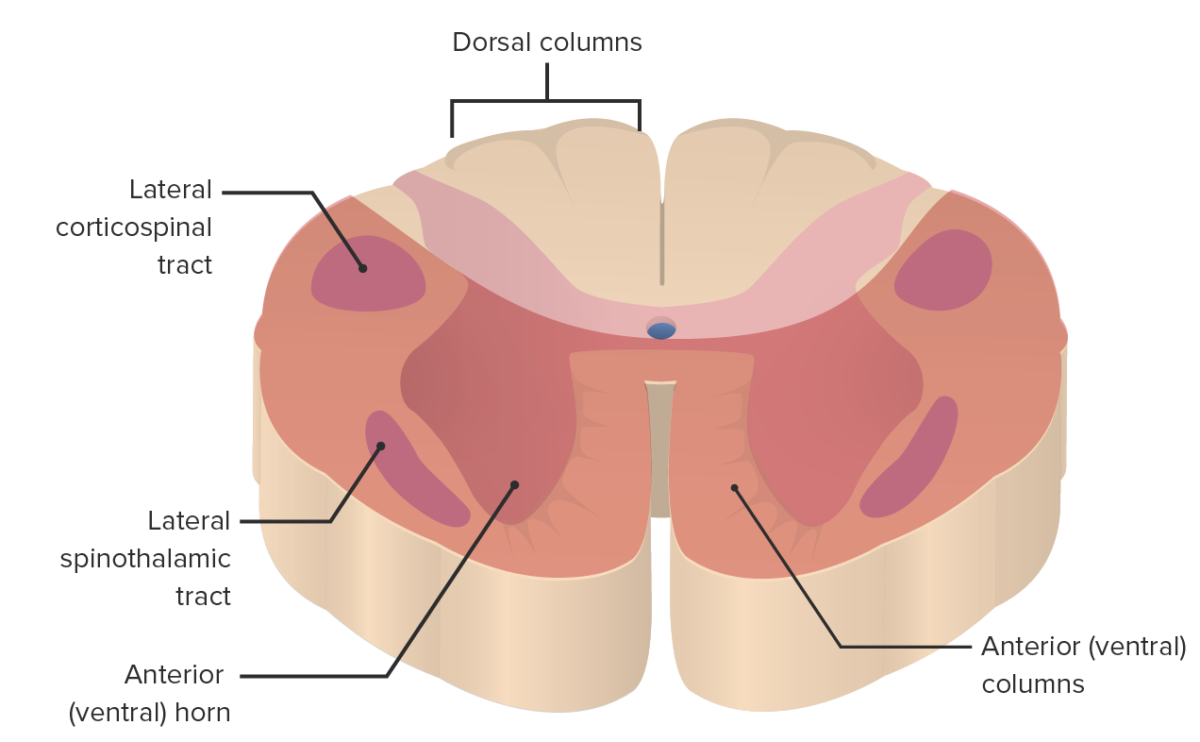
The area affected by anterior cord syndrome (salmon color)
Image by Lecturio.Understanding the structures affected by an anterior cord lesion is key to correlating clinical signs and symptoms.
History:
Physical exam findings:

Sagittal view of spinal T2 magnetic resonance imaging showing “pencil-like” ischemic changes in the spinal cord consistent with anterior cord syndrome
Image: “T2 Weighted sagittal image shows linear hyperintensity along the lower cervical and thoracic cord without cord expansion” by Nilukshana Yogendranathan, et al. License: CC BY 4.0Management is directed at relieving symptoms and preserving motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology function.