An abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease is a collection of pus in the dermis Dermis A layer of vascularized connective tissue underneath the epidermis. The surface of the dermis contains innervated papillae. Embedded in or beneath the dermis are sweat glands; hair follicles; and sebaceous glands. Skin: Structure and Functions or subcutaneous tissue. Abscesses are one of the commonly encountered skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and soft tissue infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease. Although abscesses may occur spontaneously, predisposing factors such as abrasions Abrasions Corneal Abrasions, Erosion, and Ulcers and punctures are often identified. A patient with a skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease usually presents with a localized, fluctuant Fluctuant Dermatologic Examination, tender mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast that appears red and warm. Incision and drainage Incision And Drainage Chalazion are the mainstay of management, but antibiotics can be used depending on the size of the abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease as well as the patient’s risk factors for severe infection.
Last updated: Dec 5, 2022
Soft tissue abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease is a collection of pus in the dermis Dermis A layer of vascularized connective tissue underneath the epidermis. The surface of the dermis contains innervated papillae. Embedded in or beneath the dermis are sweat glands; hair follicles; and sebaceous glands. Skin: Structure and Functions or subcutaneous tissue.
Causative agents:
Risk factors:
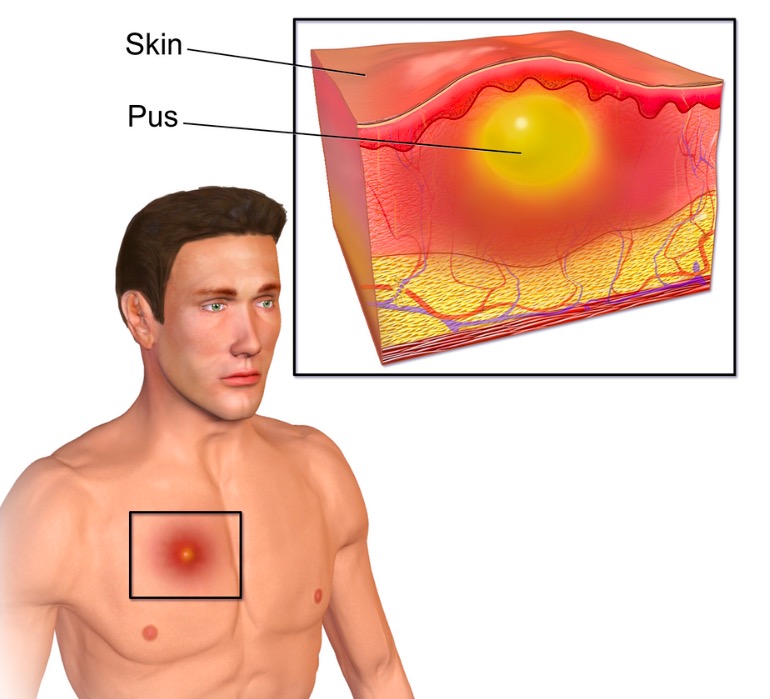
An illustration of a cutaneous abscess
Image: “Abscess” by BruceBlaus. License: CC BY 3.0
A cutaneous abscess located on the hip with some spontaneous purulent drainage
Image: “Cutaneous abscess MRSA” by CDC/Bruno Coignard, M.D. License: Public DomainSoft tissue abscesses are usually diagnosed based on exam and history.

An ultrasound showing hypoechoic area surrounded by soft tissue swelling consistent with abscess
Image: “Abscess” by Section of Emergency Medicine, Department of Medicine, Louisiana State University Health Sciences Center, New Orleans, LA 70112, USA. License: CC BY 3.0