Streptococcus is one of the two medically important genera of gram-positive Gram-Positive Penicillins cocci Cocci Bacteriology, the other being Staphylococcus Staphylococcus Staphylococcus is a medically important genera of Gram-positive, aerobic cocci. These bacteria form clusters resembling grapes on culture plates. Staphylococci are ubiquitous for humans, and many strains compose the normal skin flora. Staphylococcus. Streptococci are identified as different species on blood agar Blood agar Nocardia/Nocardiosis on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci (e.g., S. mutans, S. mitis, and S. sanguinis). Streptococcal infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease cause a wide array of clinical manifestations, including pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis, pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and soft tissue Soft Tissue Soft Tissue Abscess infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, endocarditis Endocarditis Endocarditis is an inflammatory disease involving the inner lining (endometrium) of the heart, most commonly affecting the cardiac valves. Both infectious and noninfectious etiologies lead to vegetations on the valve leaflets. Patients may present with nonspecific symptoms such as fever and fatigue. Endocarditis, septicemia, meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis, and streptococcal toxic shock syndrome Streptococcal Toxic Shock Syndrome Toxic Shock Syndrome. They are also responsible for the postinfectious syndromes of acute rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever and poststreptococcal glomerulonephritis Poststreptococcal Glomerulonephritis Post-streptococcal glomerulonephritis (PSGN) is a type of nephritis that is caused by a prior infection with group A beta-hemolytic Streptococcus (GAS). The clinical presentation of PSGN can range from asymptomatic, microscopic hematuria to full-blown acute nephritic syndrome, which is characterized by red-to-brown urine, proteinuria, edema, and acute kidney injury. Postinfectious Glomerulonephritis. Most streptococci are sensitive to penicillin Penicillin Rheumatic Fever.
Last updated: Dec 29, 2024

Streptococcus pyogenes:
Note the spherical (sometimes ovoid) shape of the cocci and their typical arrangement in chains.
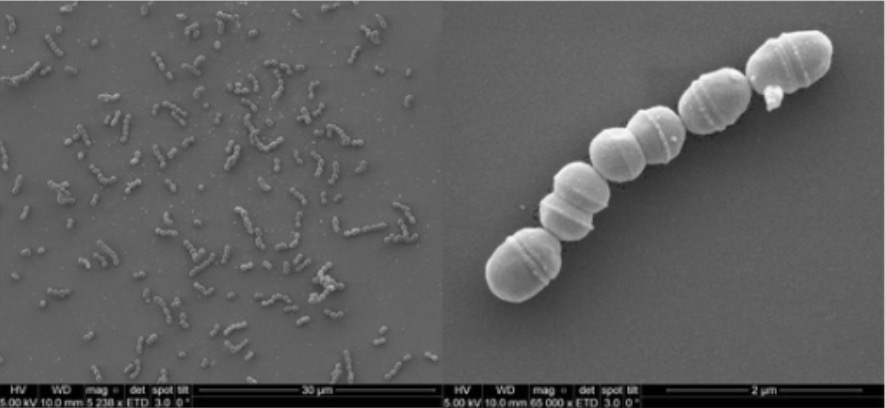
Scanning electron photomicrograph of S. agalactiae
Image: “SEM photomicrograph of S. agalactiae” by Laboratory of Cellular and Molecular Genetics (LGCM), Federal University of Minas Gerais, Belo Horizonte, Brazil. License: CC BY 4.0Streptococci have the ability to form biofilms Biofilms Encrustations formed from microbes (bacteria, algae, fungi, plankton, or protozoa) embedded in an extracellular polymeric substance matrix that is secreted by the microbes. They occur on body surfaces such as teeth (dental deposits); inanimate objects, and bodies of water. Biofilms are prevented from forming by treating surfaces with dentifrices; disinfectants; anti-infective agents; and anti-fouling agents. Proteus:
Significance:
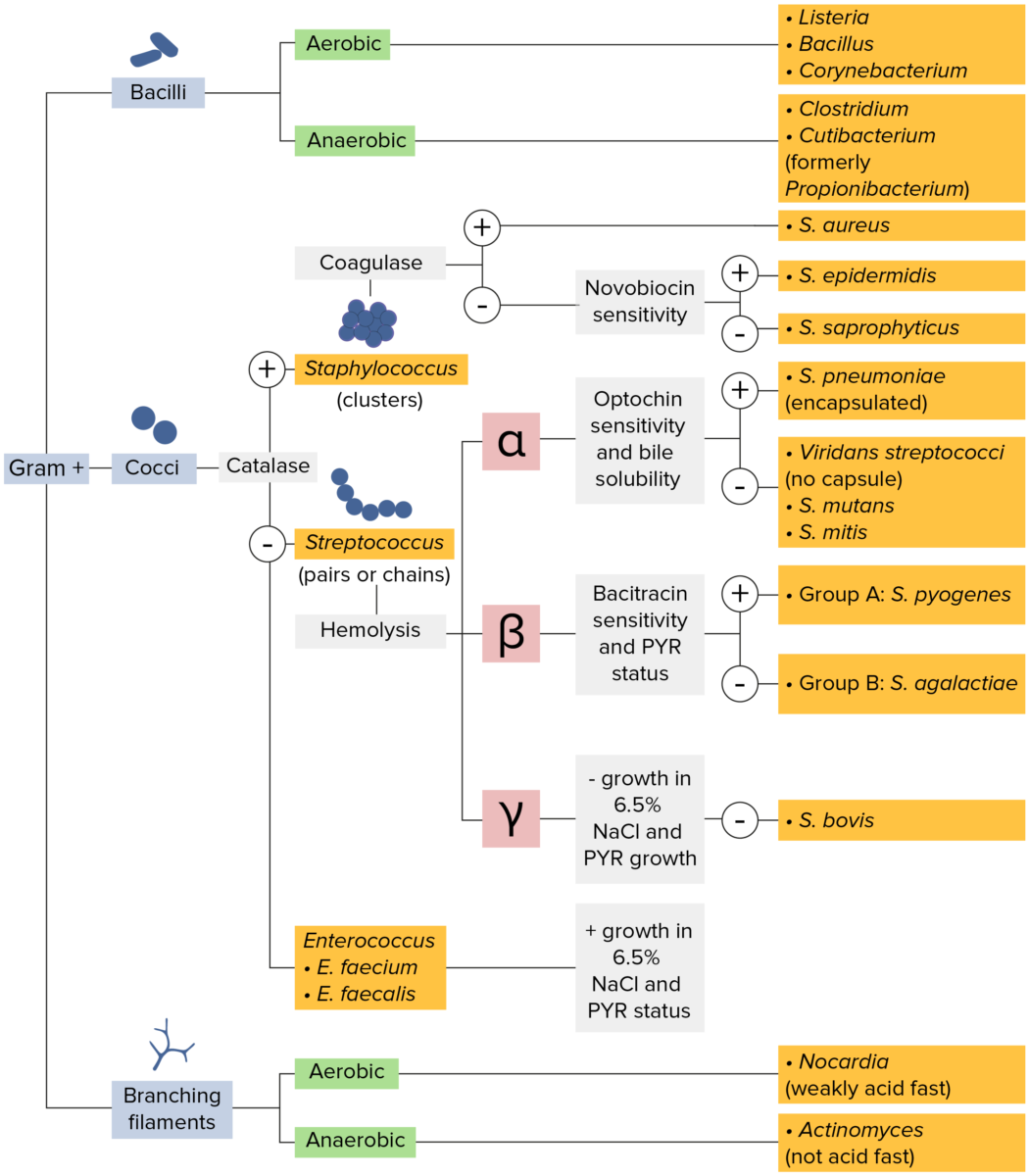
Gram-positive bacteria:
Most bacteria can be classified according to a lab procedure called Gram staining.
Bacteria with cell walls that have a thick layer of peptidoglycan retain the crystal violet stain utilized in Gram staining but are not affected by the safranin counterstain. These bacteria appear as purple-blue on the stain, indicating that they are gram positive. The bacteria can be further classified according to morphology (branching filaments, bacilli, and cocci in clusters or chains) and their ability to grow in the presence of oxygen (aerobic versus anaerobic). The cocci can also be further identified. Staphylococci can be narrowed down on the basis of the presence of the enzyme coagulase and on their sensitivity to the antibiotic novobiocin. Streptococci are grown on blood agar and classified on the basis of which form of hemolysis they employ (α, β, or γ). Streptococci are further narrowed on the basis of their response to the pyrrolidonyl-β-naphthylamide (PYR) test, their sensitivity to specific antimicrobials (optochin and bacitracin), and their ability to grow on sodium chloride (NaCl) media.
Streptococci grow well on blood agar Blood agar Nocardia/Nocardiosis. Streptococcus species are divided into 3 groups on the basis of their hemolysis pattern:

Blood agar plate showing β-hemolytic colonies of S. pyogenes:
Note the complete (beta-type) hemolysis around each colony.
| Species | Morphology | Usual habitat | Distinguishing features |
|---|---|---|---|
| S. pyogenes (group A strep) | Appear in pairs or chains | Throat Throat The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions |
|
| S. agalactiae (group B strep) | Appear in pairs or chains | Vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy, lower gastrointestinal tract |
|
| S. pneumoniae | Lancet-shaped diplococci | Nasopharynx Nasopharynx The top portion of the pharynx situated posterior to the nose and superior to the soft palate. The nasopharynx is the posterior extension of the nasal cavities and has a respiratory function. Pharynx: Anatomy |
|
| Viridans streptococci: S. mutans, S. mitis, S. sanguinis | Appear in pairs or chains | Oral cavity, colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy (S. bovis) |
|
| Enterococci (formerly group D strep, reclassified as the distinct genus
Enterococcus
Enterococcus
Enterococcus is a genus of oval-shaped gram-positive cocci that are arranged in pairs or short chains. Distinguishing factors include optochin resistance and the presence of pyrrolidonyl arylamidase (PYR) and Lancefield D antigen. Enterococcus is part of the normal flora of the human GI tract.
Enterococcus): E. faecalis, E. faecium S. gallolyticus (in group D and a member of the S. bovis group) |
Appear in pairs, short chains, or singly | Mostly in intestine, but oral cavity and vagina Vagina The vagina is the female genital canal, extending from the vulva externally to the cervix uteri internally. The structures have sexual, reproductive, and urinary functions and a rich blood supply, mainly arising from the internal iliac artery. Vagina, Vulva, and Pelvic Floor: Anatomy can be colonized |
|
Each pathogenic species of streptococci has key virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus that relate to their spread and clinical manifestations. See the charts below for a summary of these features in selected species:
| Virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus | Function |
|---|---|
| Capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides | Inhibits phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation |
| M protein (involved in rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever) |
|
| Streptolysin O | Lyses RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology |
| Streptokinase Streptokinase Streptococcal fibrinolysin. An enzyme produced by hemolytic streptococci. It hydrolyzes amide linkages and serves as an activator of plasminogen. It is used in thrombolytic therapy and is used also in mixtures with streptodornase (streptodornase and streptokinase). Thrombolytics ( fibrinolysin Fibrinolysin A product of the lysis of plasminogen (profibrinolysin) by plasminogen activators. It is composed of two polypeptide chains, light (b) and heavy (a), with a molecular weight of 75, 000. It is the major proteolytic enzyme involved in blood clot retraction or the lysis of fibrin and quickly inactivated by antiplasmins. Hemostasis) | Converts plasminogen Plasminogen Precursor of plasmin (fibrinolysin). It is a single-chain beta-globulin of molecular weight 80-90, 000 found mostly in association with fibrinogen in plasma; plasminogen activators change it to fibrinolysin. It is used in wound debriding and has been investigated as a thrombolytic agent. Hemostasis to plasmin Plasmin A product of the lysis of plasminogen (profibrinolysin) by plasminogen activators. It is composed of two polypeptide chains, light (b) and heavy (a), with a molecular weight of 75, 000. It is the major proteolytic enzyme involved in blood clot retraction or the lysis of fibrin and quickly inactivated by antiplasmins. Hemostasis and lyses blood clots, allowing bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology to escape from the clot |
| DNAse |
|
| Hyaluronidase Hyaluronidase Bacteroides | Aids in spread by splitting Splitting Defense Mechanisms hyaluronic acid Hyaluronic acid A natural high-viscosity mucopolysaccharide with alternating beta (1-3) glucuronide and beta (1-4) glucosaminidase bonds. It is found in the umbilical cord, in vitreous body and in synovial fluid. A high urinary level is found in progeria. Connective Tissue: Histology, an important component of the ground substance Ground substance Connective Tissue: Histology of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology |
| Lipoteichoic acid (covers hairlike pili Pili Filamentous or elongated proteinaceous structures which extend from the cell surface in gram-negative bacteria that contain certain types of conjugative plasmid. These pili are the organs associated with genetic transfer and have essential roles in conjugation. Normally, only one or a few pili occur on a given donor cell. This preferred use of ‘pili’ refers to the sexual appendage, to be distinguished from bacterial fimbriae, also known as common pili, which are usually concerned with adhesion. Salmonella that project through capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides) | Adhere to epithelial cells |
3 types of streptococcal
pyrogenic exotoxins
Pyrogenic Exotoxins
Scarlet Fever:
|
SpeA and SpeC are called
superantigens
Superantigens
Microbial antigens that have in common an extremely potent activating effect on T-cells that bear a specific variable region. Superantigens cross-link the variable region with class II mhc proteins regardless of the peptide binding in the t-cell receptor’s pocket. The result is a transient expansion and subsequent death and anergy of the T-cells with the appropriate variable regions.
Staphylococcus because they stimulate
T cells
T cells
Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen.
T cells: Types and Functions to produce
cytokines
Cytokines
Non-antibody proteins secreted by inflammatory leukocytes and some non-leukocytic cells, that act as intercellular mediators. They differ from classical hormones in that they are produced by a number of tissue or cell types rather than by specialized glands. They generally act locally in a paracrine or autocrine rather than endocrine manner.
Adaptive Immune Response by binding to the V-beta region of the T-cell
receptor
Receptor
Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell.
Receptors.
|
2 types of
hemolysins
Hemolysins
Proteins from bacteria and fungi that are soluble enough to be secreted to target erythrocytes and insert into the membrane to form beta-barrel pores. Biosynthesis may be regulated by hemolysin factors.
Leptospira/Leptospirosis:
|
Lyse RBCs RBCs Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology and also damage the membranes of other cells |
| Virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus | Function |
|---|---|
| Capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides | Inhibits phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation |
| Virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus | Function |
|---|---|
| Capsule Capsule An envelope of loose gel surrounding a bacterial cell which is associated with the virulence of pathogenic bacteria. Some capsules have a well-defined border, whereas others form a slime layer that trails off into the medium. Most capsules consist of relatively simple polysaccharides but there are some bacteria whose capsules are made of polypeptides. Bacteroides | Inhibits phagocytosis Phagocytosis The engulfing and degradation of microorganisms; other cells that are dead, dying, or pathogenic; and foreign particles by phagocytic cells (phagocytes). Innate Immunity: Phagocytes and Antigen Presentation |
| IgA IgA Represents 15-20% of the human serum immunoglobulins, mostly as the 4-chain polymer in humans or dimer in other mammals. Secretory iga is the main immunoglobulin in secretions. Immunoglobulins: Types and Functions protease Protease Enzyme of the human immunodeficiency virus that is required for post-translational cleavage of gag and gag-pol precursor polyproteins into functional products needed for viral assembly. HIV protease is an aspartic protease encoded by the amino terminus of the pol gene. HIV Infection and AIDS | Mucosal invasion |
| Virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus | Function |
|---|---|
| Dextrans | Platelet adhesion Adhesion The process whereby platelets adhere to something other than platelets, e.g., collagen; basement membrane; microfibrils; or other ‘foreign’ surfaces. Coagulation Studies |
| In vivo biofilm Biofilm Encrustations formed from microbes (bacteria, algae, fungi, plankton, or protozoa) embedded in an extracellular polymeric substance matrix that is secreted by the microbes. They occur on body surfaces such as teeth (dental deposits); inanimate objects, and bodies of water. Biofilms are prevented from forming by treating surfaces with dentifrices; disinfectants; anti-infective agents; and anti-fouling agents. Staphylococcus production | Adhesion Adhesion The process whereby platelets adhere to something other than platelets, e.g., collagen; basement membrane; microfibrils; or other ‘foreign’ surfaces. Coagulation Studies |
Streptococcus pyogenes is the most virulent pathogen in the Streptococcus family.
Pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis:

Streptococcal pharyngitis:
Redness and edema of the throat and palatal petechiae
Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and soft tissue Soft Tissue Soft Tissue Abscess infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease:

Impetigo in a child:
The image shows characteristic “honey-crusted” lesions around the mouth.
Puerperal fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever: occurs when S. pyogenes enters uterus Uterus The uterus, cervix, and fallopian tubes are part of the internal female reproductive system. The uterus has a thick wall made of smooth muscle (the myometrium) and an inner mucosal layer (the endometrium). The most inferior portion of the uterus is the cervix, which connects the uterine cavity to the vagina. Uterus, Cervix, and Fallopian Tubes: Anatomy after delivery, causing endometritis Endometritis Endometritis is an inflammation of the endometrium, the inner layer of the uterus. The most common subtype is postpartum endometritis, resulting from the ascension of normal vaginal flora to the previously aseptic uterus. Postpartum Endometritis and bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides
Bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides or sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock caused by:
Scarlet fever Scarlet fever Infection with group a Streptococci that is characterized by tonsillitis and pharyngitis. An erythematous rash is commonly present. Scarlet Fever:

Rash of scarlet fever
Image: “The rash of scarlet fever” by Alicia Williams. License: CC BY 2.5Toxic shock syndrome Toxic Shock Syndrome Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing. Toxic Shock Syndrome ( TSS TSS Toxic shock syndrome (TSS) is an acute, multi-systemic disease caused by the toxin-producing bacteria, Staphylococcus aureus and Streptococcus pyogenes. Staphylococcal TSS is more common and associated with tampons and nasal packing. Toxic Shock Syndrome):
Rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever:
Poststreptococcal glomerulonephritis Poststreptococcal Glomerulonephritis Post-streptococcal glomerulonephritis (PSGN) is a type of nephritis that is caused by a prior infection with group A beta-hemolytic Streptococcus (GAS). The clinical presentation of PSGN can range from asymptomatic, microscopic hematuria to full-blown acute nephritic syndrome, which is characterized by red-to-brown urine, proteinuria, edema, and acute kidney injury. Postinfectious Glomerulonephritis ( PSGN PSGN Post-streptococcal glomerulonephritis (PSGN) is a type of nephritis that is caused by a prior infection with group A beta-hemolytic Streptococcus (GAS). The clinical presentation of PSGN can range from asymptomatic, microscopic hematuria to full-blown acute nephritic syndrome, which is characterized by red-to-brown urine, proteinuria, edema, and acute kidney injury. Postinfectious Glomerulonephritis):
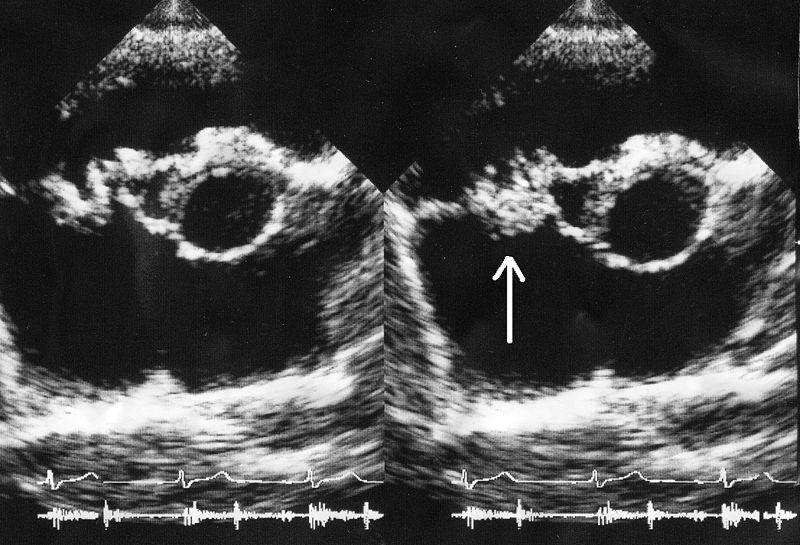
Infective endocarditis:
A bacterial vegetation (arrow) is seen on the tricuspid valve on an echocardiogram.
| Species | Identification Identification Defense Mechanisms | Prevention |
|---|---|---|
| S. pyogenes Group A strep (GAS) |
|
Early (before day 8) antibiotic treatment of pharyngitis Pharyngitis Pharyngitis is an inflammation of the back of the throat (pharynx). Pharyngitis is usually caused by an upper respiratory tract infection, which is viral in most cases. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, and hoarseness. Pharyngitis to prevent rheumatic fever Rheumatic fever Acute rheumatic fever (ARF) is an autoimmune inflammatory process that usually follows Streptococcal pharyngitis. Acute rheumatic fever usually occurs 2-4 weeks after an untreated infection and affects the heart, skin, joints, and nervous system. Rheumatic Fever ( RF RF Rheumatoid Arthritis) and continued chemoprophylaxis Chemoprophylaxis Meningitis in Children for years in persons who have had an attack of RF RF Rheumatoid Arthritis to prevent relapse Relapse Relapsing Fever of RF RF Rheumatoid Arthritis activity |
| S. agalactiae group B strep ( GBS GBS An acute inflammatory autoimmune neuritis caused by t cell- mediated cellular immune response directed towards peripheral myelin. Demyelination occurs in peripheral nerves and nerve roots. The process is often preceded by a viral or bacterial infection, surgery, immunization, lymphoma, or exposure to toxins. Common clinical manifestations include progressive weakness, loss of sensation, and loss of deep tendon reflexes. Weakness of respiratory muscles and autonomic dysfunction may occur. Polyneuropathy) |
|
Screen all pregnant women at 35–37 weeks for GBS GBS An acute inflammatory autoimmune neuritis caused by t cell- mediated cellular immune response directed towards peripheral myelin. Demyelination occurs in peripheral nerves and nerve roots. The process is often preceded by a viral or bacterial infection, surgery, immunization, lymphoma, or exposure to toxins. Common clinical manifestations include progressive weakness, loss of sensation, and loss of deep tendon reflexes. Weakness of respiratory muscles and autonomic dysfunction may occur. Polyneuropathy and administer IV antibiotics ( penicillin Penicillin Rheumatic Fever) during labor to prevent neonatal infection Neonatal infection Chikungunya Virus |
| S. pneumoniae |
|
Immunization, following U.S. Advisory Committee on Immunization Practices (ACIP) guidelines for different ages and medical conditions, with:
|
| Viridans streptococci: S. mutans, S. bovis, S. mitis | Blood cultures, then biochemical testing (often unreliable for viridans species, so molecular testing or a mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast spectrometry method increasingly being used) | Prophylactic antibiotics in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with high-risk conditions (e.g., prosthetic heart valves, unrepaired cyanotic congenital heart disease) who are undergoing a dental procedure |
| Enterococcus Enterococcus Enterococcus is a genus of oval-shaped gram-positive cocci that are arranged in pairs or short chains. Distinguishing factors include optochin resistance and the presence of pyrrolidonyl arylamidase (PYR) and Lancefield D antigen. Enterococcus is part of the normal flora of the human GI tract. Enterococcus | Cultures (growth in 6.5% NaCl), then biochemical testing, molecular testing, or mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast spectrometry methods |