Small bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis (SBO) is an interruption of the flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of the intraluminal contents through the small intestine Small intestine The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy; it is classified as mechanical (due to physical blockage) or functional (due to disruption of normal motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility). The most common cause of SBO in the Western countries is postsurgical adhesions. Small bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis typically presents with nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, abdominal pain Abdominal Pain Acute Abdomen, distention, constipation Constipation Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic or functional constipation) or secondary, and as acute or chronic. Constipation, and/or obstipation Obstipation Large Bowel Obstruction. The diagnosis is established via imaging. Up to 80% of all cases will resolve with supportive management (bowel rest, intravenous (IV) hydration, and nasogastric decompression). However, surgery is required for persistent or complicated cases.
Last updated: May 17, 2024
Small bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis (SBO) is the interruption of the flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of intraluminal contents through the small bowel Small bowel The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy ( duodenum Duodenum The shortest and widest portion of the small intestine adjacent to the pylorus of the stomach. It is named for having the length equal to about the width of 12 fingers. Small Intestine: Anatomy, jejunum Jejunum The middle portion of the small intestine, between duodenum and ileum. It represents about 2/5 of the remaining portion of the small intestine below duodenum. Small Intestine: Anatomy, or ileum Ileum The distal and narrowest portion of the small intestine, between the jejunum and the ileocecal valve of the large intestine. Small Intestine: Anatomy).
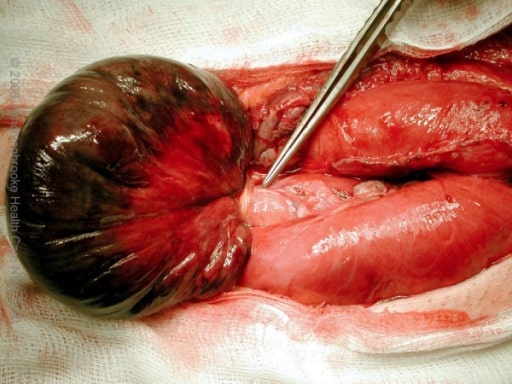
Gangrenous small bowel with closed-loop obstruction caused by an omental band adhesion
Image: “Intra-operative photograph” by the Department of Surgery, Hinchingbrooke Hospital, Hinchingbrooke Healthcare NHS Trust, Huntingdon, Cambridgeshire, UK. License: CC BY 2.0.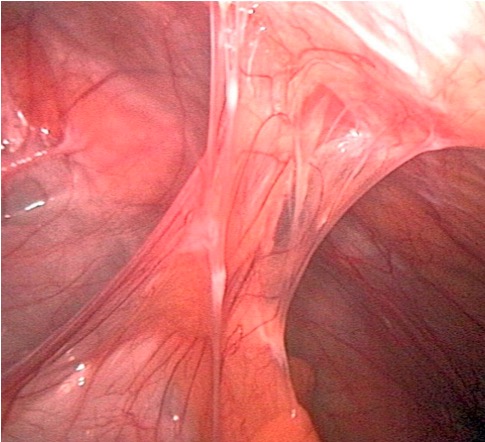
Adhesions that can develop post-surgery are the most common cause of bowel obstruction.
Image by Kevin Pei, PD.
X-ray showing intestinal loops with air-fluid levels consistent with SBO
Image: “X-ray” by the Department of Surgery, University Hospital of Ioannina, Greece. License: CC BY 2.0.
Abdominal X-ray showing dilated small bowel loops consistent with SBO
Image: “Abdominal X-ray” by the Department of General Surgery, Sunderland Royal Hospital, Kayll Road, Sunderland SR4 7TP, UK. License: CC BY 2.0.
A CT scan showing the transition zone (arrow) with proximal bowel dilation and distal bowel decompression
Image: “Abdominal CT Scan” by the 2nd Department of Surgery, Athens University School of Medicine, Aretaieion Hospital, Athens, Greece. License: CC BY 2.0.
A CT scan showing a hernia causing a small obstruction with air-fluid levels
Image: “Abdominal CT scan” by the Service des Urgences Chirurgicales Viscérales, Centre Hospitalier Universitaire Ibn Rochd, Casablanca, Morocco. License: CC BY 2.0.