Large bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis is an interruption in the normal flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure of intestinal contents through the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy and rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy. This obstruction may be mechanical (due to the actual physical occlusion of the lumen) or functional (due to a loss of normal peristalsis Peristalsis A movement, caused by sequential muscle contraction, that pushes the contents of the intestines or other tubular organs in one direction. Gastrointestinal Motility, also known as pseudo-obstruction). Malignancy Malignancy Hemothorax and volvulus Volvulus A volvulus is the twisting or axial rotation of a portion of the bowel around its mesentery. The most common site of volvulus in adults is the colon; most frequently the sigmoid volvulus. Patients typically present with symptoms of bowel obstruction such as abdominal pain, distension, vomiting, and constipation/obstipation. Volvulus are the most common causes of mechanical large bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis. Typical symptoms include intermittent lower abdominal pain Abdominal Pain Acute Abdomen, abdominal distention Abdominal distention Megacolon, and obstipation. Diagnosis is established with imaging. Mechanical large bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis requires surgery in most cases.
Last updated: Dec 29, 2024
A large bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis (LBO) is an interruption in the normal passage of bowel contents through the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy and rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy.
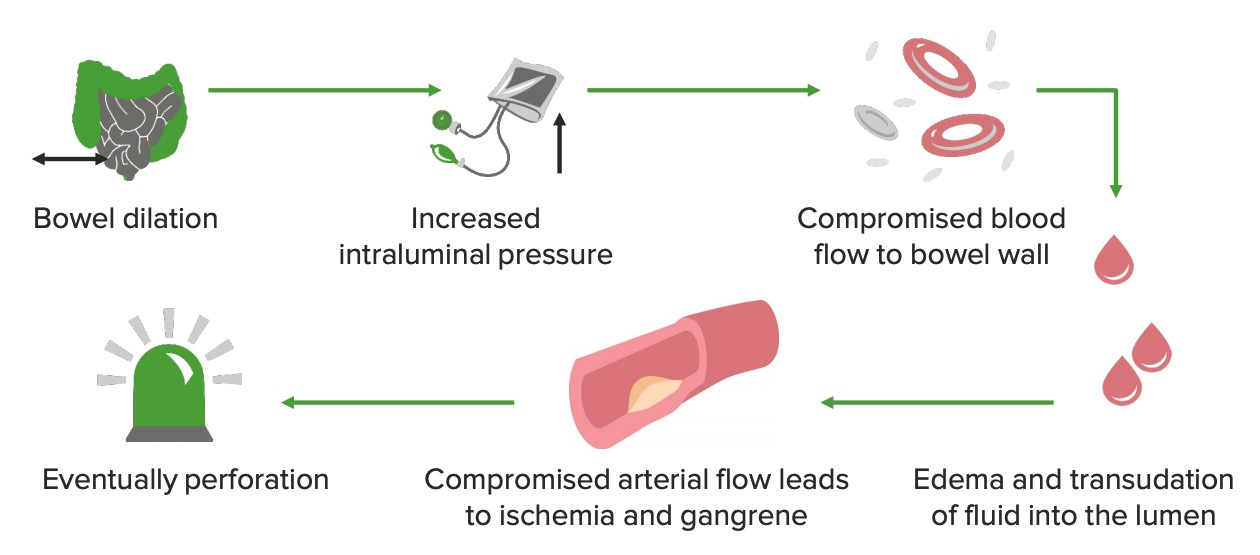
Pathophysiology of LBO
Image by Lecturio.
Abdominal X-ray showing significant colon dilation due to a sigmoid volvulus
Image: “Sigmoidvolvulus” by Mont4nha. License: CC0
Rectal obstruction: Abdominal X-ray shows dilatation of proximal colon.
Image: “X-ray” by Second Department of Surgery, Medical School, Democritus University of Thrace, Dragana, 68100 Alexandroupolis, Greece. License: CC BY 2.0
An abdominal X-ray showing severe colonic dilation due to pseudo-obstruction
Image: “Abdominal X-ray” by Pradhum Ram. License: CC BY 4.0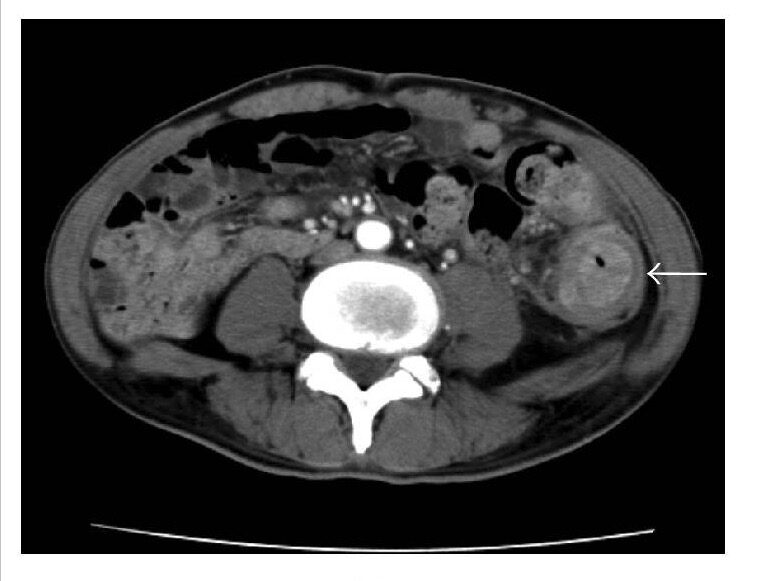
Descending colon cancer (arrow) causing stenosis of the descending colon
Image: “CT” by Department of Surgery 1, School of Medicine, University of Occupational and Environmental Health, 1-1 Iseigaoka, Yahata-nishi-ku, Kitakyushu 807-8555, Japan. License: CC BY 4.0, edited by Lecturio.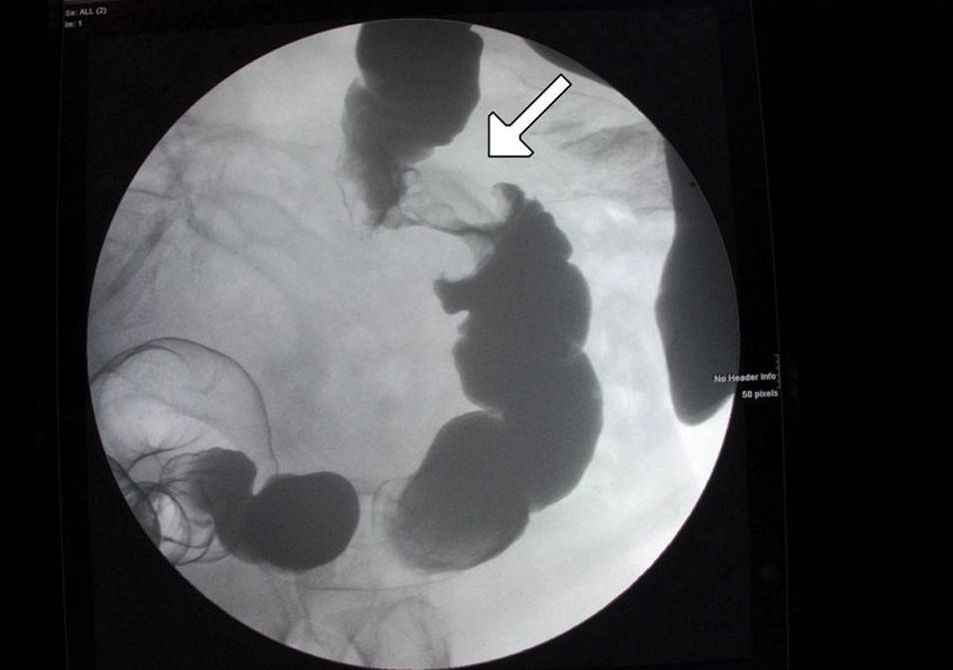
An “apple core” lesion of the colon shown on contrast enema: This is concerning for cancer.
Image: “Figure 6” by Alzaraa et al. License: CC BY 3.0
Operative findings showing a large sigmoid volvulus
Image: “F2” by General Surgery Department, Aga Khan University Hospital, Stadium Road, Karachi 74800, Pakistan. License: CC BY 2.0