Pseudomembranous colitis is inflammation of the colon caused by an overgrowth of the bacterium Clostridioides difficile. This condition is associated with antibiotic use and the consequent disruption of the normal colonic microbiota. It is one of the most common healthcare-associated infections and a significant cause of morbidity and mortality, especially in hospitalized older adults. Clinical manifestations of C. difficile infection (CDI) include asymptomatic colonization, diarrheal illness, and fulminant colitis with sepsis in severe cases. The diagnosis is established based on stool studies. Most patients can be treated with antibiotics. Fecal transplantation is considered in a few cases, whereas surgical intervention may be required in severe cases.
Last updated: Mar 24, 2025
Pseudomembranous colitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy caused by overgrowth of the bacterium Clostridioides difficile.
| Characteristics | Mild-to-moderate colitis | Severe colitis | Fulminant colitis |
|---|---|---|---|
| Number of loose stools/day | < 6 | ≥ 6 | ≥ 6 |
| Fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever | – | +/– | +/– |
| WBC count | < 15,000/µL | > 15,000/µL | > 15,000/µL |
| Severe abdominal pain Abdominal Pain Acute Abdomen | – | + | + |
| Rising creatinine levels | – | +/– | +/– |
| Multiorgan dysfunction | – | – | + |
| Complete ileus Ileus A condition caused by the lack of intestinal peristalsis or intestinal motility without any mechanical obstruction. This interference of the flow of intestinal contents often leads to intestinal obstruction. Ileus may be classified into postoperative, inflammatory, metabolic, neurogenic, and drug-induced. Small Bowel Obstruction or toxic megacolon Toxic megacolon An acute form of megacolon, severe pathological dilatation of the colon. It is associated with clinical conditions such as ulcerative colitis; Crohn disease; amebic dysentery; or Clostridium enterocolitis. Megacolon | – | – | + |
| Radiological signs of colitis, ileus Ileus A condition caused by the lack of intestinal peristalsis or intestinal motility without any mechanical obstruction. This interference of the flow of intestinal contents often leads to intestinal obstruction. Ileus may be classified into postoperative, inflammatory, metabolic, neurogenic, and drug-induced. Small Bowel Obstruction, or toxic megacolon Toxic megacolon An acute form of megacolon, severe pathological dilatation of the colon. It is associated with clinical conditions such as ulcerative colitis; Crohn disease; amebic dysentery; or Clostridium enterocolitis. Megacolon | – | +/– | + |
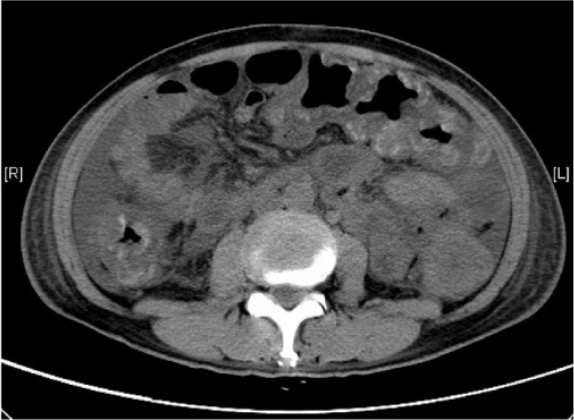
Computed tomography scan of severe pseudomembranous colitis: diffuse colonic wall thickening, with areas suggestive of mucosal hemorrhage
Image: “Abdominal computer tomography” by Division of Gastroenterology and Hepatology, Department of Medicine and Geriatrics, Tuen Mun Hospital, Tsing Chung Koon Road, Tuen Mun, New Territories, Hong Kong. License: CC BY 4.0
Endoscopic view of fulminant pseudomembranous colitis: multiple polypoid lesions covered with yellow pseudomembranes
Image: “Endoscopic view of the sigmoid colon” by Division of Gastroenterology and Hepatology, Department of Medicine and Geriatrics, Tuen Mun Hospital, Tsing Chung Koon Road, Tuen Mun, New Territories, Hong Kong. License: CC BY 4.0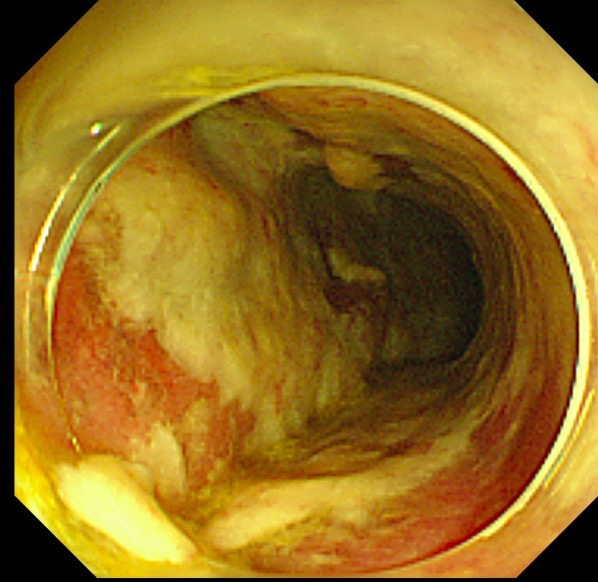
Endoscopy showing thick pseudomembranes typical of pseudomembranous colitis
Image: “Colonoscopy on the 5th postoperative day” by Abe et al. License: CC BY 2.0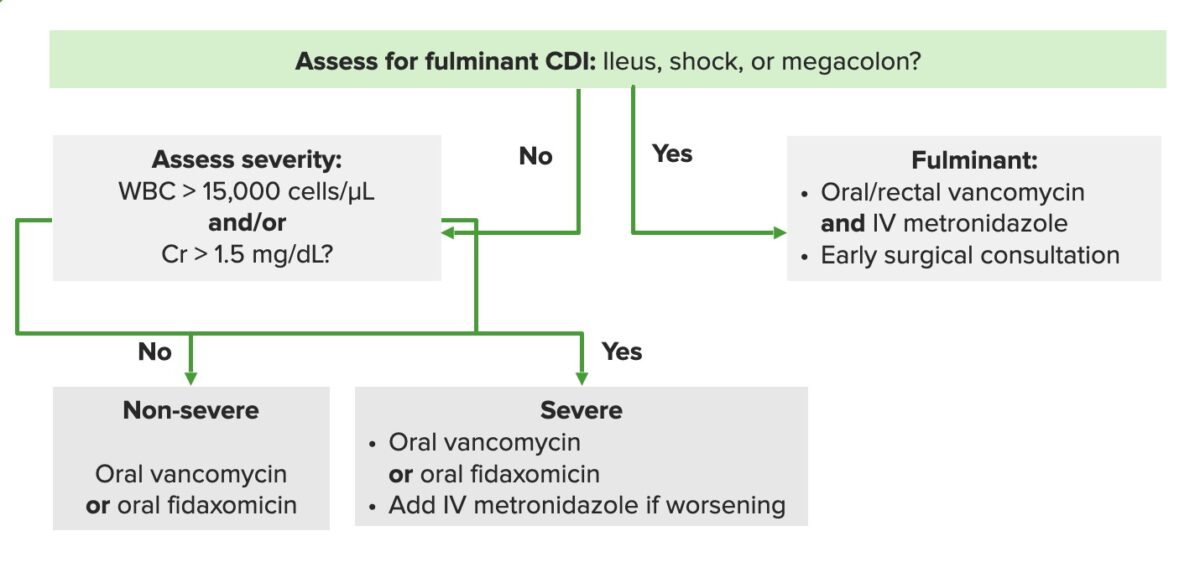
Algorithm for an approach to the management of Clostridium difficile infections (CDIs). Cr: creatinine, IV: intravenous
Image by Lecturio.Possible indications:
Surgical interventions: