Megacolon is a severe, abnormal dilatation of the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy, and is classified as acute or chronic. There are many etiologies of megacolon, including neuropathic and dysmotility conditions, severe infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage, and inflammatory bowel disease. Toxic megacolon is an acute form of megacolon with systemic toxicity Toxicity Dosage Calculation, and carries the highest morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status. Common symptoms include abdominal distention, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, bloody diarrhea Bloody diarrhea Diarrhea, or obstipation Obstipation Large Bowel Obstruction. Diagnosis depends on the underlying cause, and is usually established with a combination of the patient’s history, laboratory findings, and imaging studies. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with chronic megacolon may require laxatives Laxatives Laxatives are medications used to promote defecation. Most often, laxatives are used to treat constipation or for bowel preparation for certain procedures. There are 4 main classes of laxatives: bulk-forming, stimulant, osmotic, and emollient. Laxatives, enemas, and bowel training. Management for acute megacolon includes supportive care, decompression, and potential surgery.
Last updated: Jun 17, 2025
Megacolon is a severe dilatation of the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy secondary to impaired motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility or an inflammatory process. The condition is classified based on the time course and duration:
These studies help evaluate the severity of the disease, complications, and potential causes.
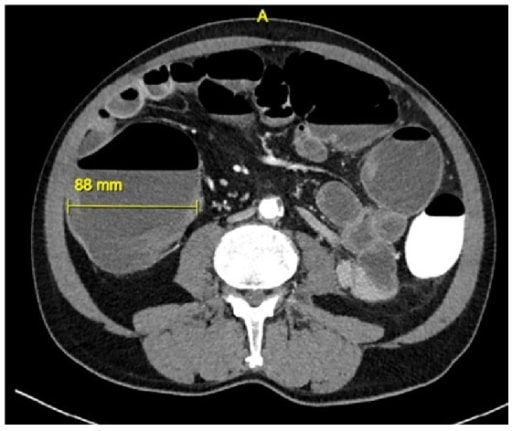
Computed tomography image of toxic megacolon secondary to C. difficile infection
This CT shows colonic distension of 8.8 cm.

Abdominal X-ray of a 2-month-old patient with congenital aganglionic megacolon (Hirschsprung’s disease)
This image shows dilated loops of the small bowel and colon.
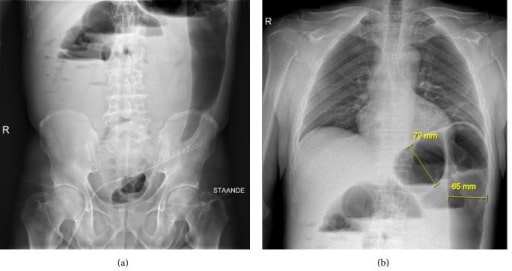
X-ray image of a patient with toxic megacolon
The X-ray was performed in the standing position, and shows colonic air-fluid levels in the epigastric region and the splenic flexure.
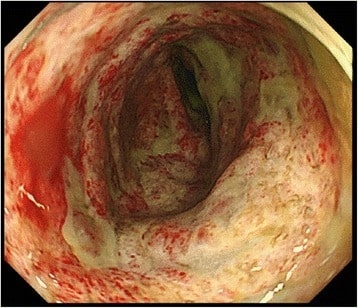
Colonoscopy image showing a severe ulcer and pseudomembrane at the descending colon in a patient with toxic megacolon
Image: “Colonoscopy” by Department of Gastroenterological Surgery, Clinical Research Institute Cancer Research Division, National Kyushu Medical Center, Fukuoka, Japan. License: CC BY 4.0
Surgical findings for toxic megacolon related to C. difficile colitis
Image: “Toxic megacolon” by University of Pittsburgh Department of Pathology. License: CC BY 3.0