Function of the GI system is highly regulated through neural and hormonal signaling. Much of this regulation comes from the ANS. Parasympathetic stimulation is excitatory, triggering digestive secretions, an increase in GI blood flow, and movement of material through the tract, while sympathetic stimulation is inhibitory and has the opposite effects. The GI tract also has its own enteric nervous system, which controls numerous local GI reflexes. For example, the presence of a particular nutrient may be detected by chemoreceptors and may trigger release of a particular digestive enzyme, which is coordinated entirely by the enteric nervous system (without input from the brain). In addition, there are numerous hormones and paracrine signaling molecules released by GI organs that similarly affect GI function.
Last updated: Dec 12, 2022
The GI system is constantly working to meet human energy demands. To achieve this end, the GI system has several major functions:
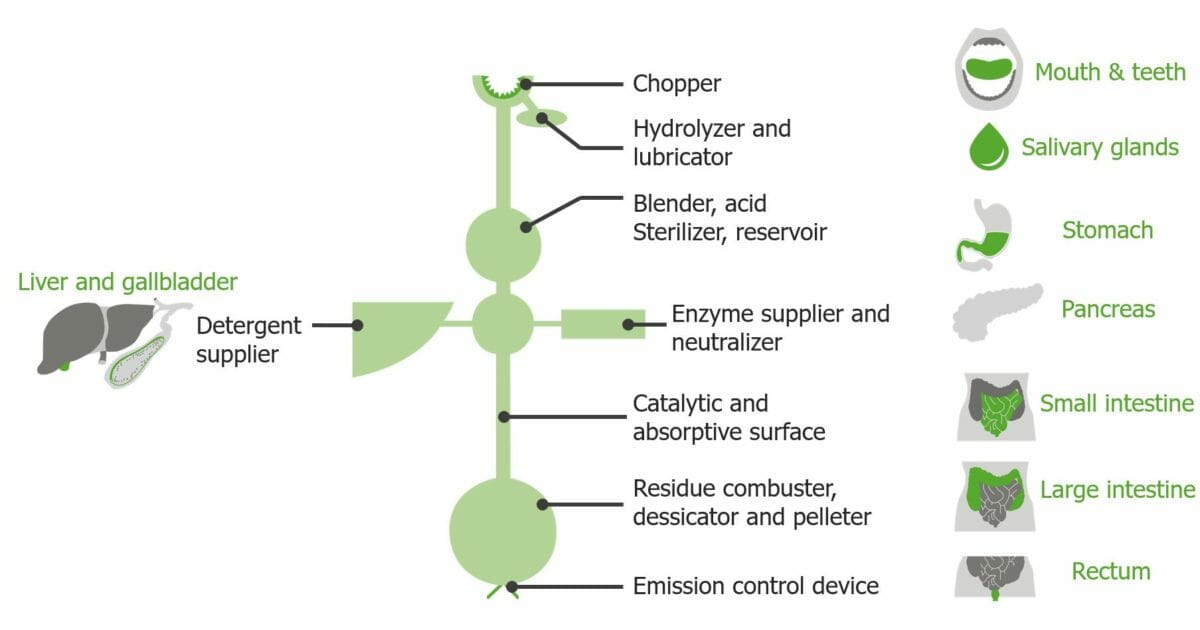
As a way of understanding the GI system, the GI tract can be envisioned as an “engineering tube,” as shown here, with different segments having specialized functions.
Image by Lecturio.Autonomic control of the GI tract relies on the enteric, parasympathetic, and sympathetic nervous systems.
A specialized portion of the autonomic nervous system Autonomic nervous system The ANS is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ANS consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy located within the walls of the GI tract.
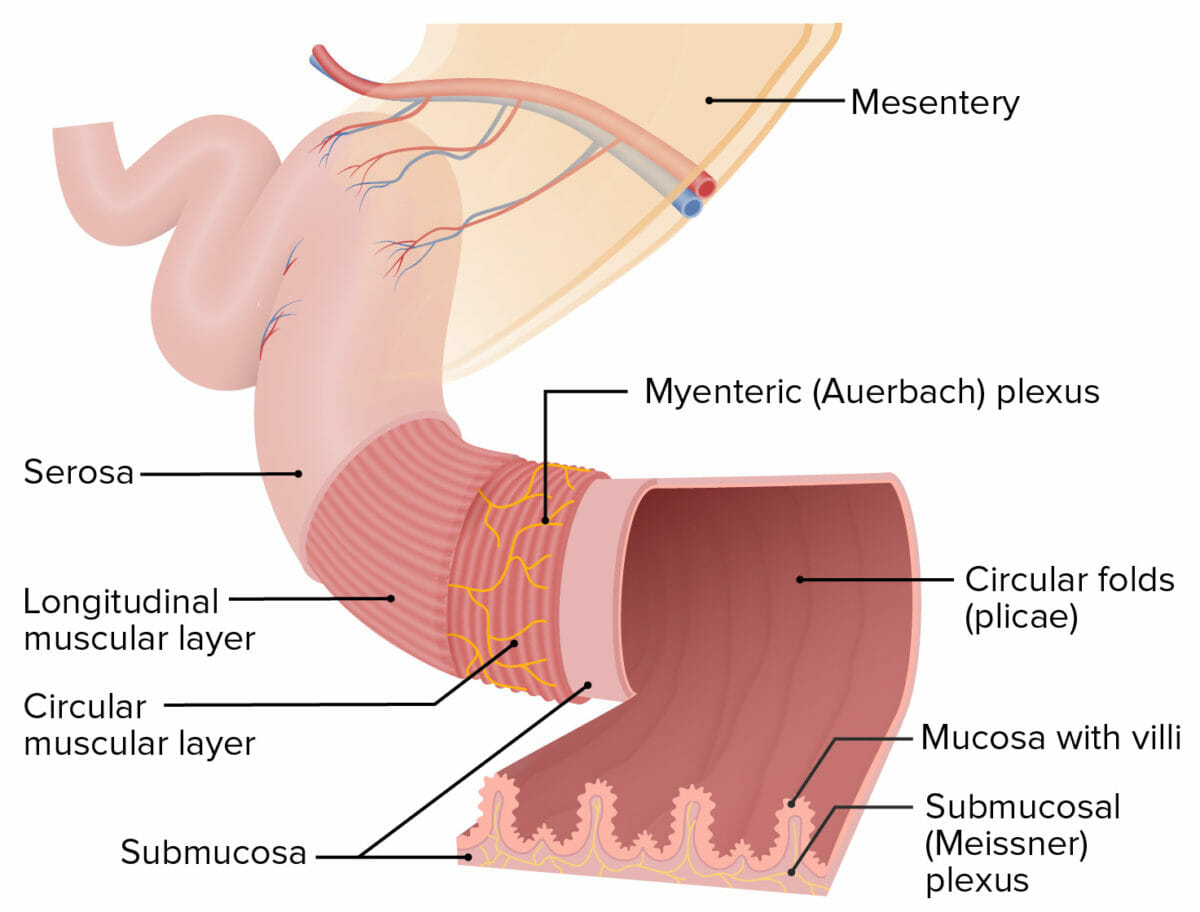
Structure of the intestinal walls:
The Meissner plexus is located within the submucosa, and the Auerbach plexus (also known as the myenteric plexus) is located between the circular and longitudinal muscular layers.
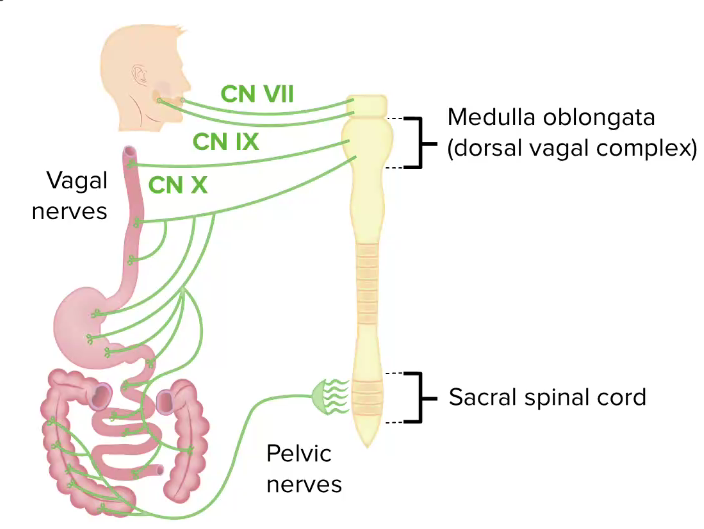
Parasympathetic influence on the GI tract:
Note the vast reach of the vagus nerve.
CN: cranial nerve
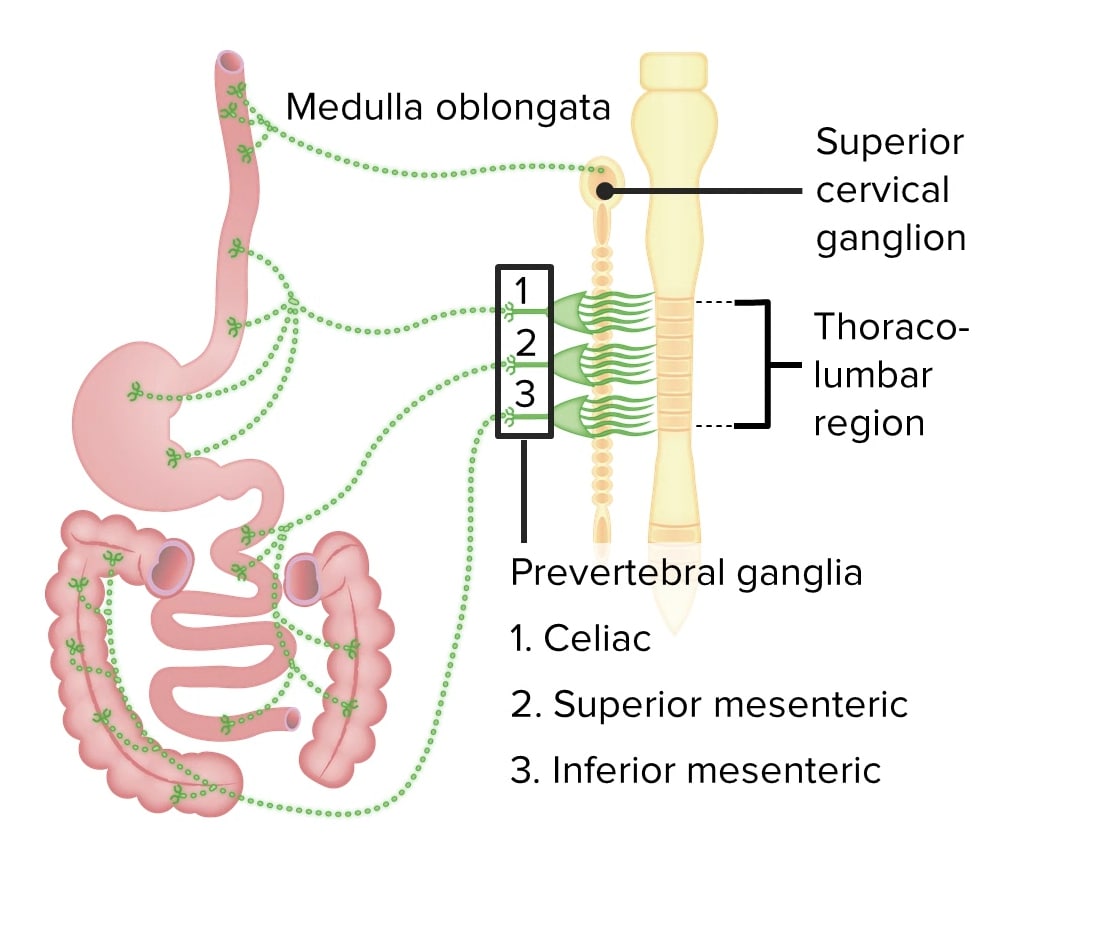
Sympathetic nervous system influence on the GI tract
Image by Lecturio.Vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs:
Vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure:
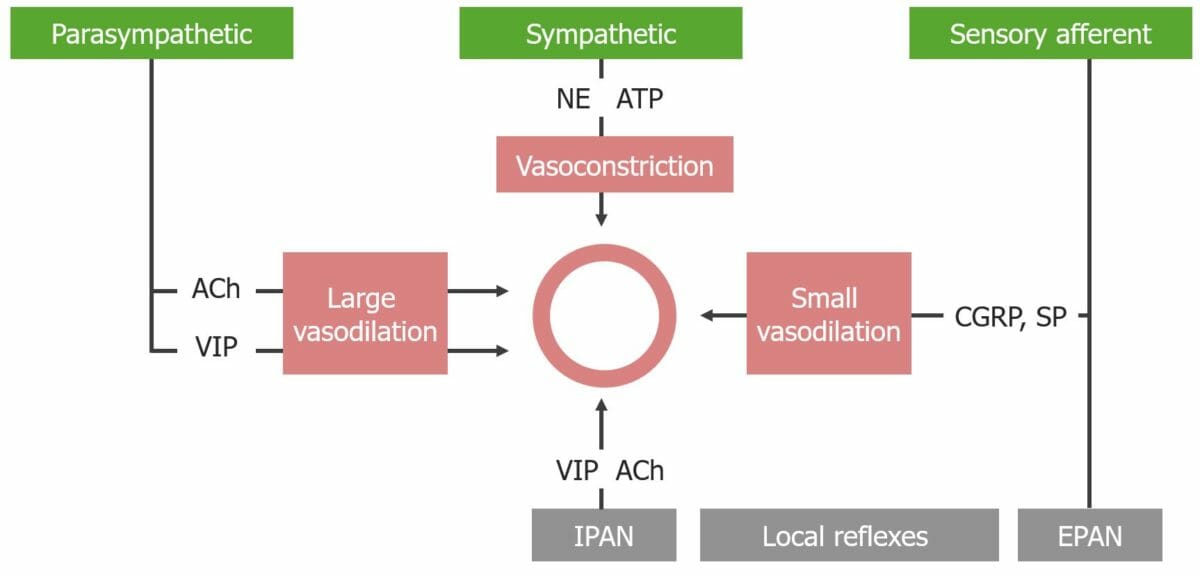
Flowchart detailing the regulation of blood flow to the GI tract
ACh: acetylcholine
CGRP: calcitonin gene–related peptide
EPAN: extrinsic primary afferent neuron
IPAN : intrinsic primary afferent
NE: norepinephrine
SP: substance P
VIP: vasoactive intestinal
The nervous system Nervous system The nervous system is a small and complex system that consists of an intricate network of neural cells (or neurons) and even more glial cells (for support and insulation). It is divided according to its anatomical components as well as its functional characteristics. The brain and spinal cord are referred to as the central nervous system, and the branches of nerves from these structures are referred to as the peripheral nervous system. Nervous System: Anatomy, Structure, and Classification sends signals to mediate activity in the GI tract. Nerves in the PNS, SNS, ENS, and sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology afferent Afferent Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology nerves release different types of signaling molecules Signaling molecules Second Messengers, which have different effects on their target tissue.
| Molecule | Primary releasing nerve(s) | Structure(s) acted on | Primary function |
|---|---|---|---|
| Acetylcholine Acetylcholine A neurotransmitter found at neuromuscular junctions, autonomic ganglia, parasympathetic effector junctions, a subset of sympathetic effector junctions, and at many sites in the central nervous system. Receptors and Neurotransmitters of the CNS | PNS |
|
Increases secretions, motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility, and blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure |
| VIP | PNS and ENS |
|
Increase motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility and blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure |
| GRP | PNS and ENS | Glands | Increase gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions secretion Secretion Coagulation Studies |
| Enkephalins Enkephalins One of the three major families of endogenous opioid peptides. The enkephalins are pentapeptides that are widespread in the central and peripheral nervous systems and in the adrenal medulla. Receptors and Neurotransmitters of the CNS (related to opioids Opioids Opiates are drugs that are derived from the sap of the opium poppy. Opiates have been used since antiquity for the relief of acute severe pain. Opioids are synthetic opiates with properties that are substantially similar to those of opiates. Opioid Analgesics) | ENS | Smooth muscle | Constrict sphincters (prevents forward movement) |
| CGRP | Sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology afferents | Blood vessels | Increase blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure via vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs |
| Substance P | Sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology afferents and PNS |
|
Increase blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure |
| Norepinephrine Norepinephrine Precursor of epinephrine that is secreted by the adrenal medulla and is a widespread central and autonomic neurotransmitter. Norepinephrine is the principal transmitter of most postganglionic sympathetic fibers, and of the diffuse projection system in the brain that arises from the locus ceruleus. Receptors and Neurotransmitters of the CNS | SNS |
|
Decrease secretions, motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility, and blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure |
| ATP | SNS | Blood vessels | Decrease blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure via vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure |
The GI hormones GI Hormones Hormones secreted by the gastrointestinal mucosa that affect the timing or the quality of secretion of digestive enzymes, and regulate the motor activity of the digestive system organs. Gastrointestinal Secretions are secreted by enteroendocrine cells Enteroendocrine cells Cells found throughout the lining of the gastrointestinal tract that contain and secrete regulatory peptide hormones and/or biogenic amines. Gastrointestinal Secretions and modulate function of the GI tract. Enteroendocrine cells Enteroendocrine cells Cells found throughout the lining of the gastrointestinal tract that contain and secrete regulatory peptide hormones and/or biogenic amines. Gastrointestinal Secretions are spread throughout the GI tract.
| Molecule | Primarily released from | Structure(s) acted on | Primary function |
|---|---|---|---|
| Gastrin Gastrin A family of gastrointestinal peptide hormones that excite the secretion of gastric juice. They may also occur in the central nervous system where they are presumed to be neurotransmitters. Gastrointestinal Secretions | G cells in the:
|
Stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy |
|
| Cholecystokinin Cholecystokinin A peptide, of about 33 amino acids, secreted by the upper intestinal mucosa and also found in the central nervous system. It causes gallbladder contraction, release of pancreatic exocrine (or digestive) enzymes, and affects other gastrointestinal functions. Cholecystokinin may be the mediator of satiety. Gastrointestinal Secretions | I cells in the:
|
Exocrine pancreas Exocrine pancreas The major component (about 80%) of the pancreas composed of acinar functional units of tubular and spherical cells. The acinar cells synthesize and secrete several digestive enzymes such as trypsinogen; lipase; amylase; and ribonuclease. Secretion from the exocrine pancreas drains into the pancreatic ductal system and empties into the duodenum. Pancreas: Anatomy, gallbladder Gallbladder The gallbladder is a pear-shaped sac, located directly beneath the liver, that sits on top of the superior part of the duodenum. The primary functions of the gallbladder include concentrating and storing up to 50 mL of bile. Gallbladder and Biliary Tract: Anatomy, and stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy |
|
| Gastric inhibitory peptide (GIP) | K cells in the:
|
Stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy, endocrine pancreas Endocrine pancreas Pancreas: Anatomy |
|
| Motilin Motilin A peptide of about 22-amino acids isolated from the duodenum. At low ph it inhibits gastric motor activity, whereas at high ph it has a stimulating effect. Gastrointestinal Secretions |
M cells
M cells
Salmonella in the:
|
Smooth muscle |
|
| Secretin Secretin A peptide hormone of about 27 amino acids from the duodenal mucosa that activates pancreatic secretion and lowers the blood sugar level. Gastrointestinal Secretions | S cells in the:
|
Pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy and stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy |
|
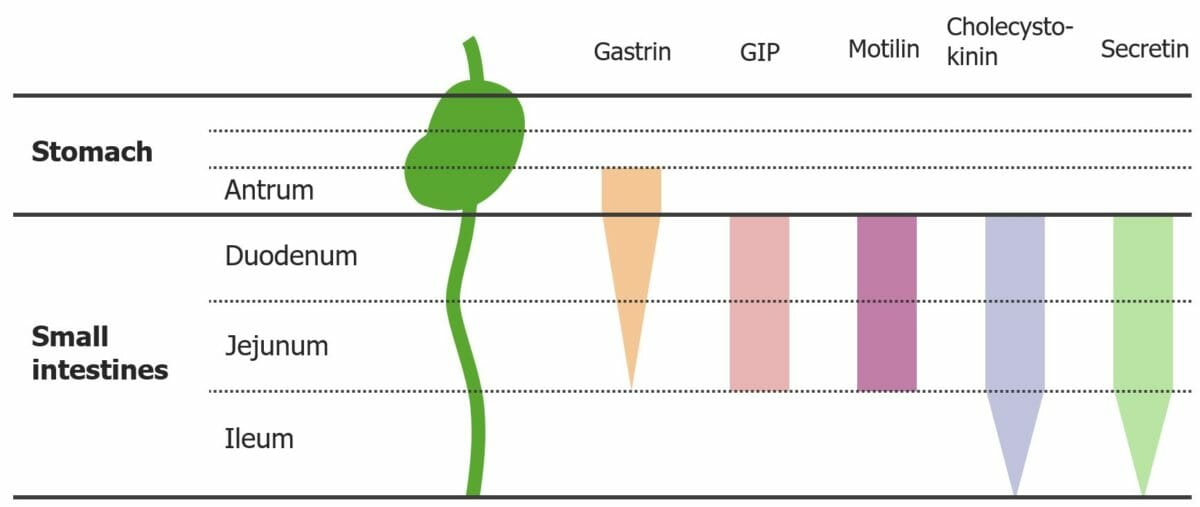
Diagram showing the locations from which GI hormones are released:
The tapered ends on the gastrin, cholecystokinin, and secretin bars represent the decreasing amounts of hormone secretion in these locations.
GIP: gastric inhibitory peptide
Paracrine signaling molecules Signaling molecules Second Messengers are similar to hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types; however, instead of traveling to different tissues via the blood, paracrine signaling molecules Signaling molecules Second Messengers affect cells close to the site of their release. The major paracrine signaling molecules Signaling molecules Second Messengers in the GI system are histamine, NO, prostaglandins Prostaglandins A group of compounds derived from unsaturated 20-carbon fatty acids, primarily arachidonic acid, via the cyclooxygenase pathway. They are extremely potent mediators of a diverse group of physiological processes. Eicosanoids, and somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions.
| Molecule | Released from | Structure(s) acted on | Primary function |
|---|---|---|---|
| Histamine |
|
Stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy | Increase acid secretion Secretion Coagulation Studies |
| Somatostatin Somatostatin A 14-amino acid peptide named for its ability to inhibit pituitary growth hormone release, also called somatotropin release-inhibiting factor. It is expressed in the central and peripheral nervous systems, the gut, and other organs. SRIF can also inhibit the release of thyroid-stimulating hormone; prolactin; insulin; and glucagon besides acting as a neurotransmitter and neuromodulator. In a number of species including humans, there is an additional form of somatostatin, srif-28 with a 14-amino acid extension at the n-terminal. Gastrointestinal Secretions | D cells | Stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy and pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy | Inhibit secretion Secretion Coagulation Studies |
| Prostaglandins Prostaglandins A group of compounds derived from unsaturated 20-carbon fatty acids, primarily arachidonic acid, via the cyclooxygenase pathway. They are extremely potent mediators of a diverse group of physiological processes. Eicosanoids (PGs) | Numerous | Mucosa | Increase mucus and bicarbonate Bicarbonate Inorganic salts that contain the -HCO3 radical. They are an important factor in determining the ph of the blood and the concentration of bicarbonate ions is regulated by the kidney. Levels in the blood are an index of the alkali reserve or buffering capacity. Electrolytes secretion Secretion Coagulation Studies |
| NO | Numerous | Smooth muscle, blood vessels | Relax smooth muscle and increase blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure |