The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx Pharynx The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy to the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. The wall of the esophagus is made up of 4 primary layers: mucosa (lined with squamous epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology), submucosa, a thicker muscularis layer, and an outer layer of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology. The esophagus also has a sphincter at each end, which allows it to help control the passage of food into the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy.
Last updated: Nov 19, 2024
Embryologic development of the esophagus:
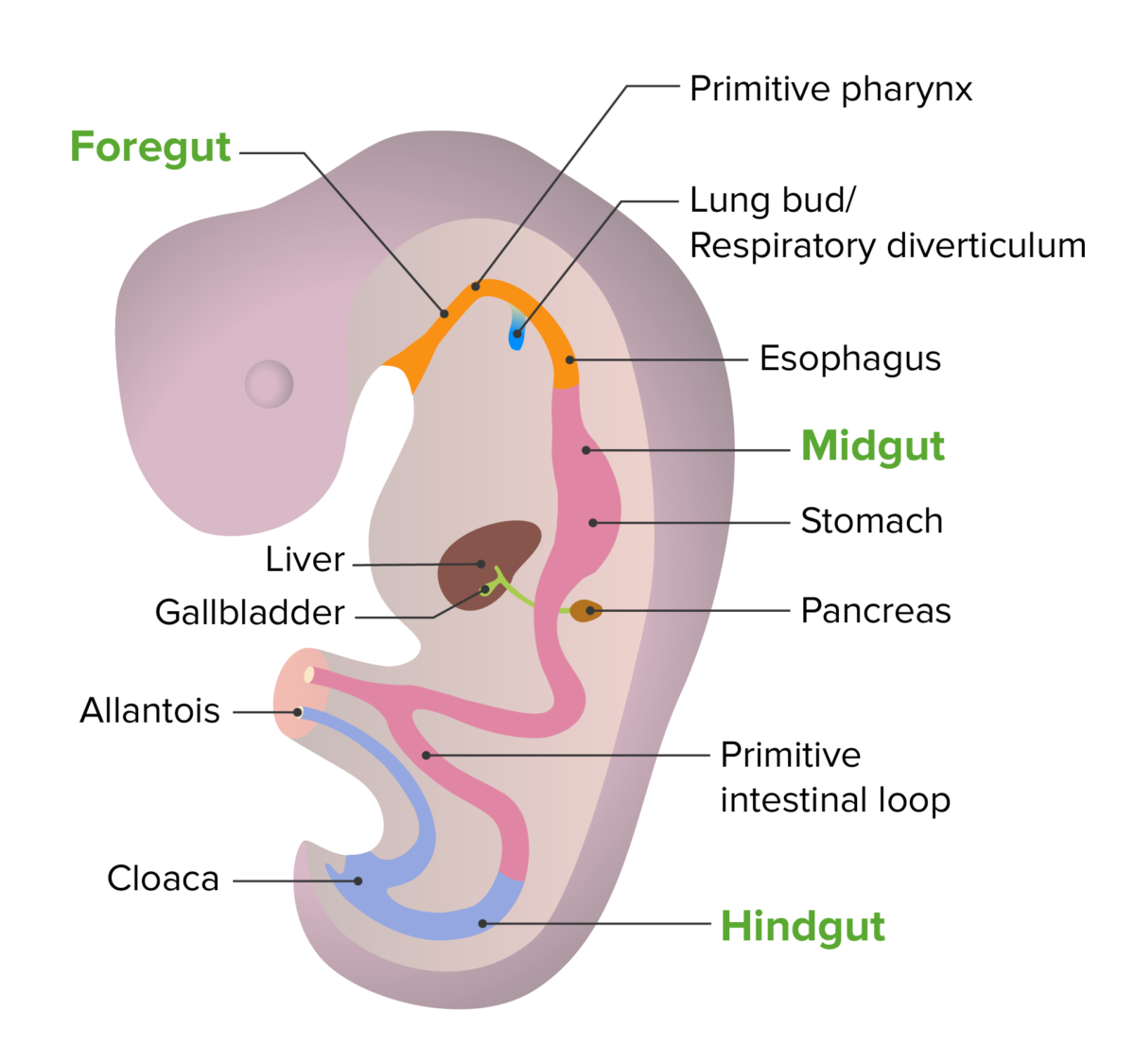
Embryonic development of the gut tube
Image by Lecturio. License: CC BY-NC-SA 4.0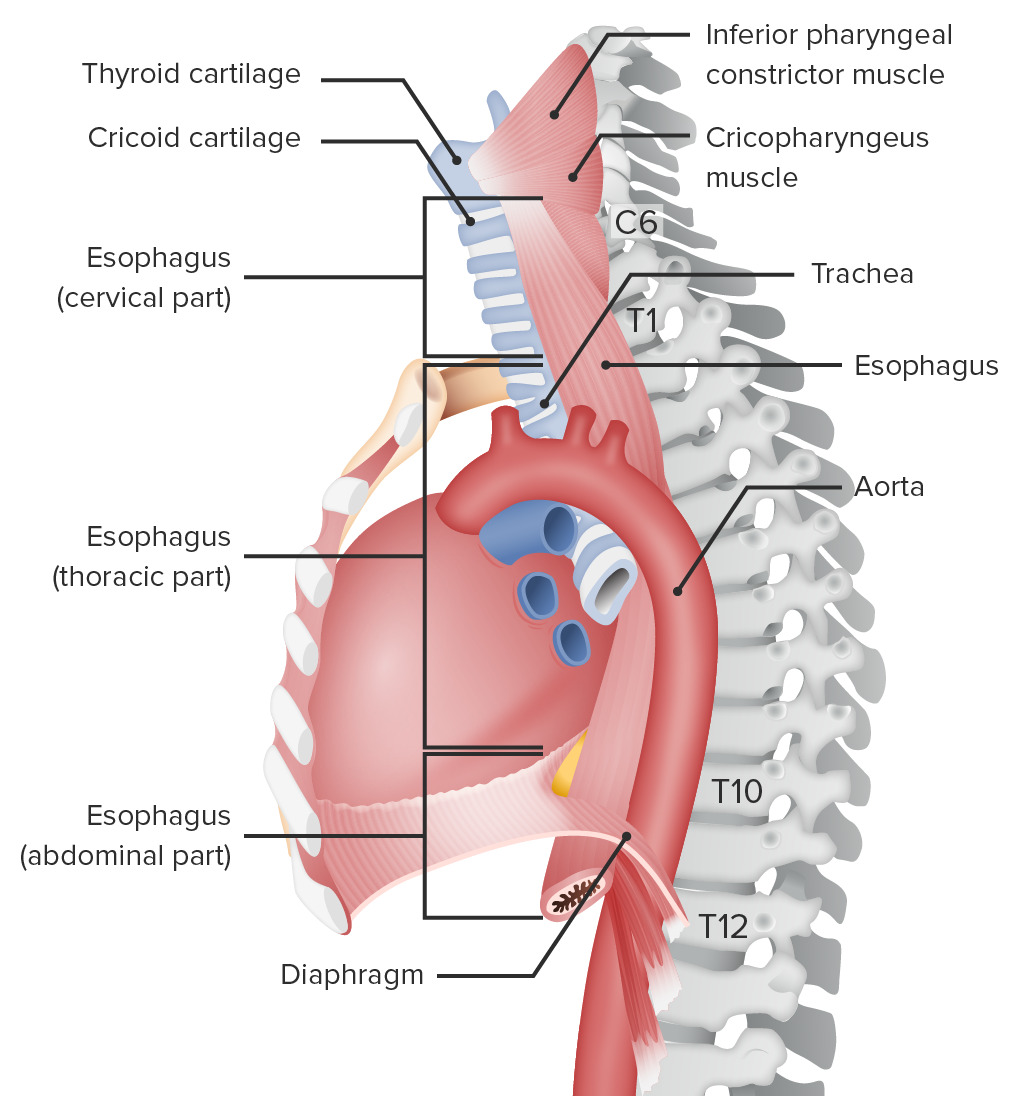
Location of the esophagus
Image by Lecturio.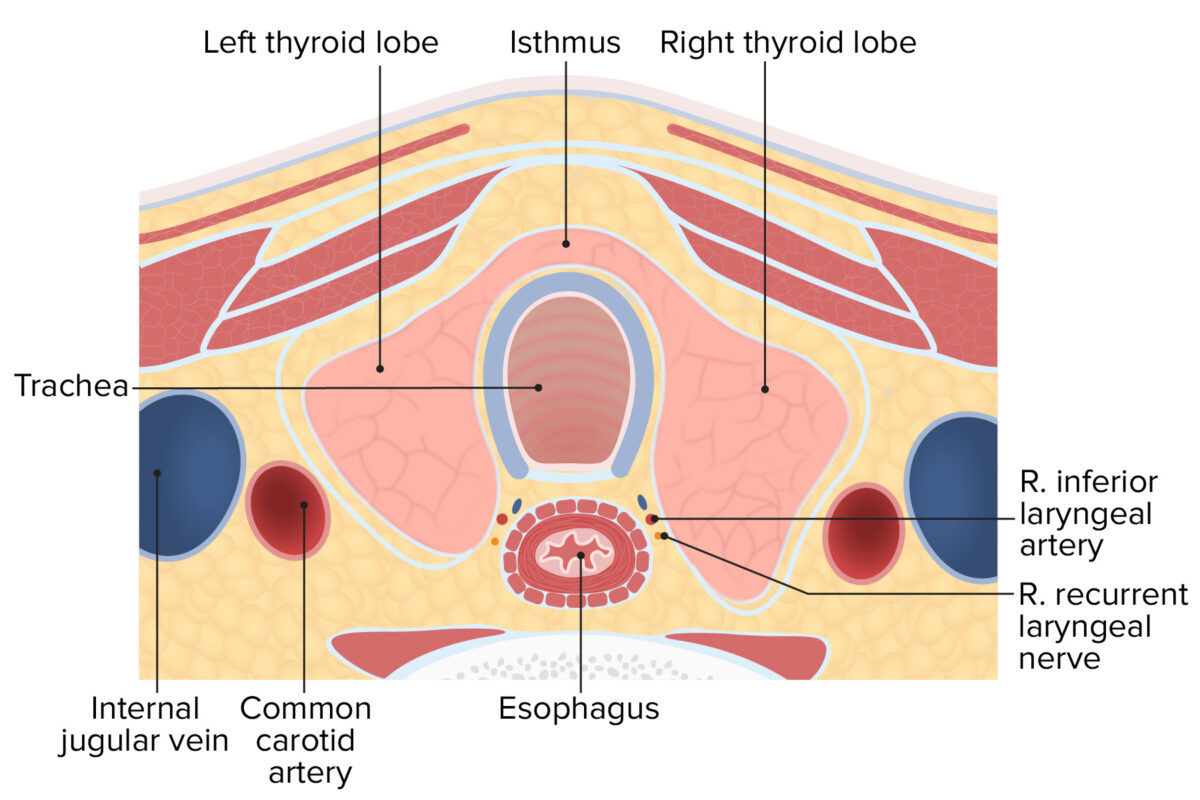
Cross section of the neck displaying the relationship between the thyroid, trachea, esophagus, and carotid sheath
Image by Lecturio.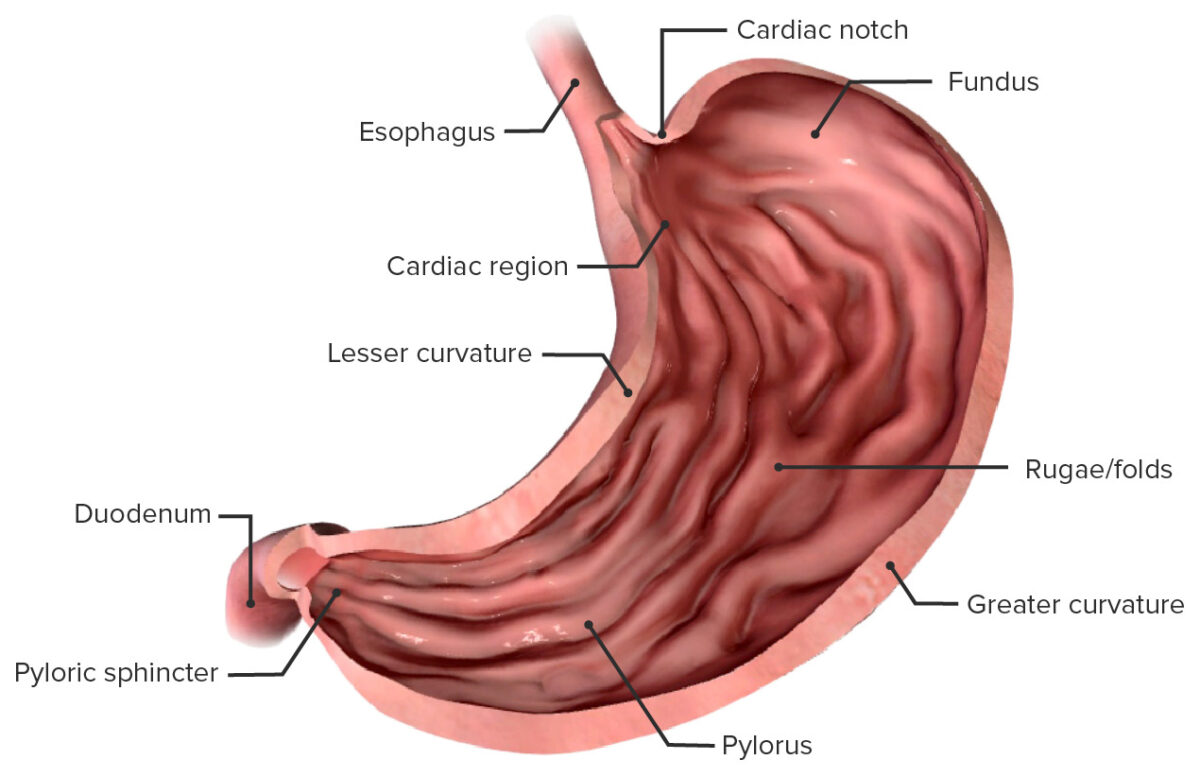
Anatomical components of the stomach and their relationship to the abdominal esophagus
Image by BioDigital, edited by LecturioConstrictions are normal narrowings in the esophagus tube.
The esophageal wall consists of 4 primary layers:
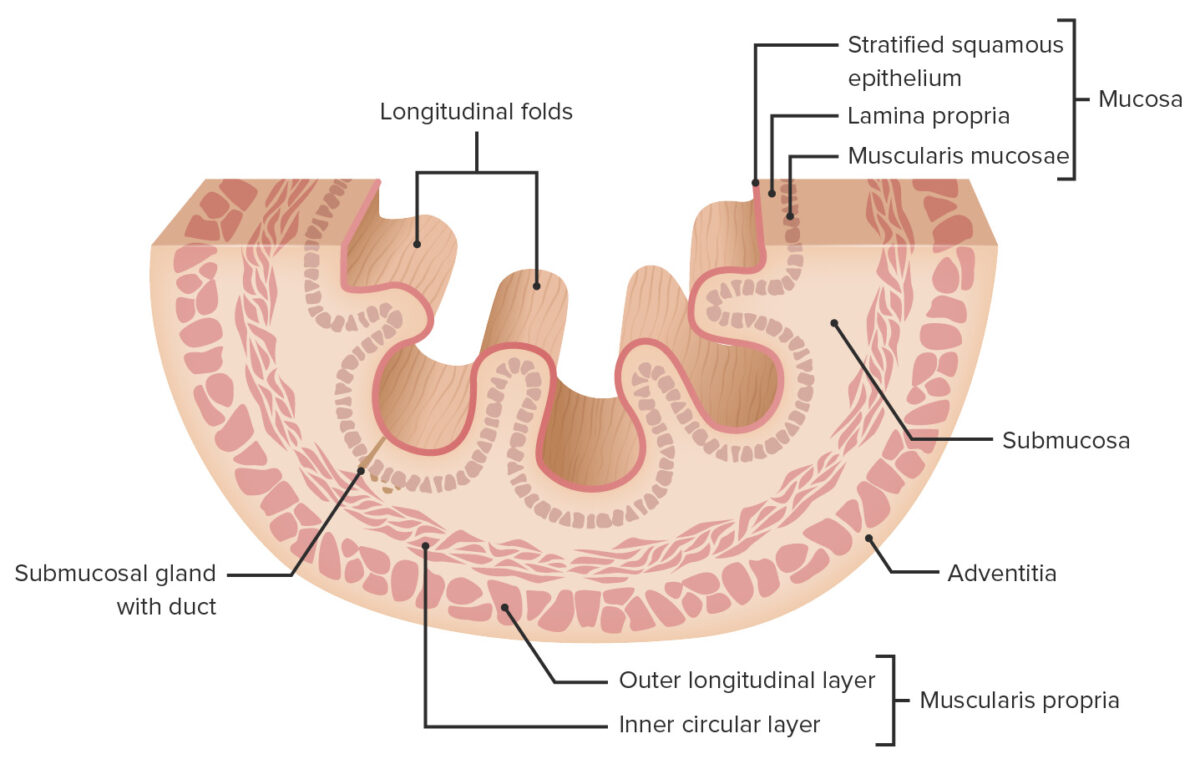
Layers of the esophageal wall
Image by Lecturio.Consists of 3 sublayers:
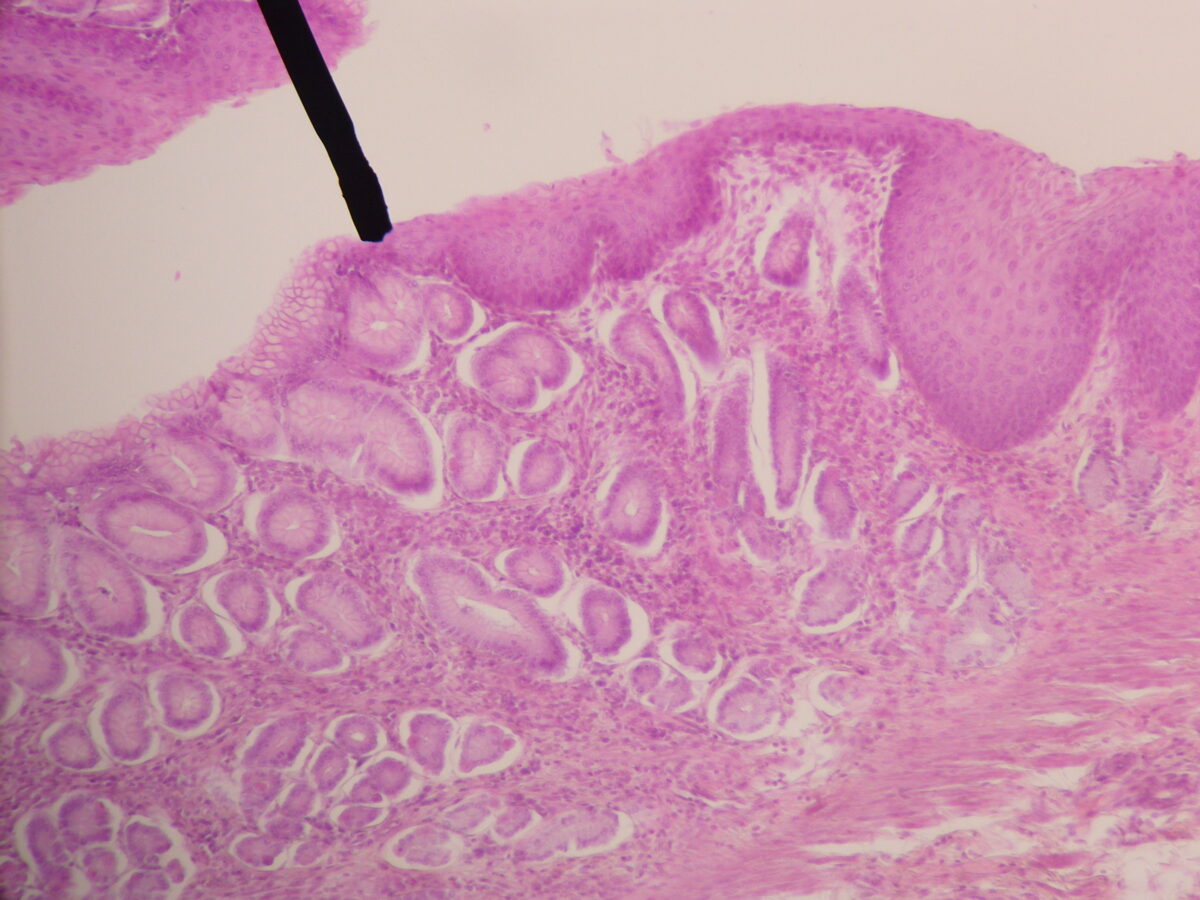
Histological section of the gastroesophageal (GE) junction:
Note the squamous epithelium lining of the esophagus to the right of the black line and columnar epithelium of the stomach to the left.
Located between the mucosal and muscular layers, the submucosal layer is a layer of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology that contains:
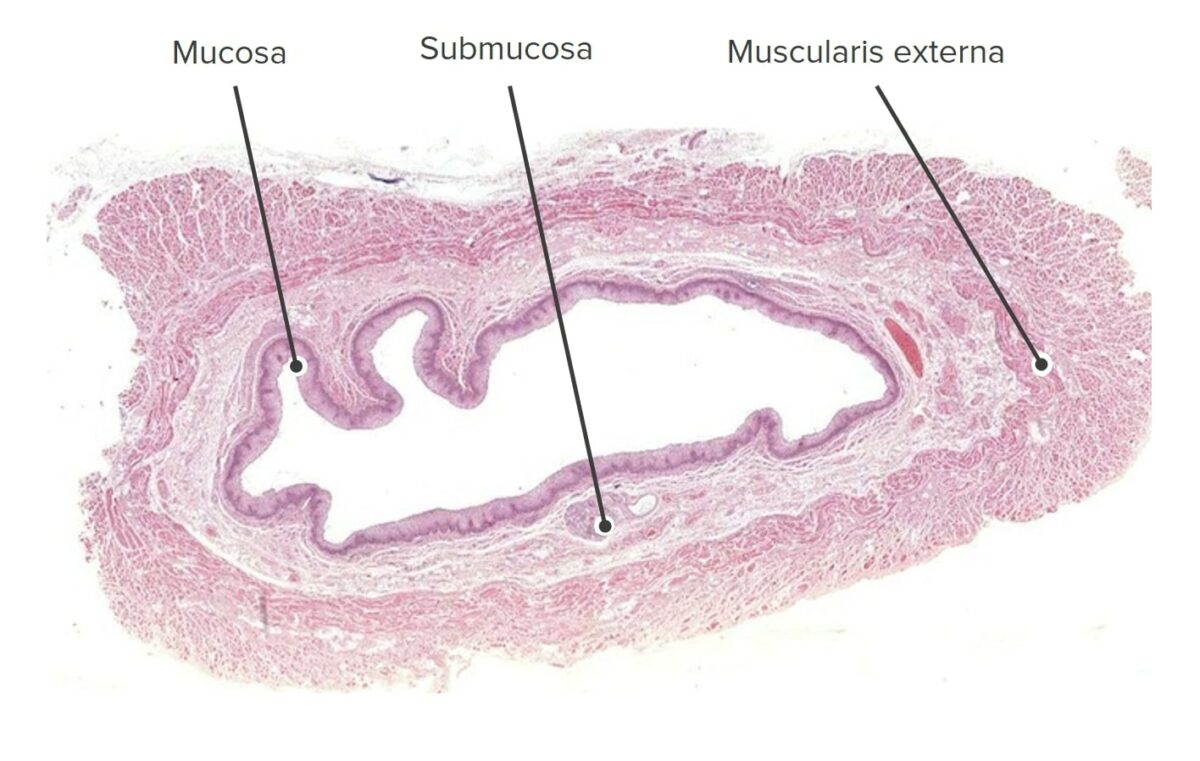
Low-magnification cross-sectional image of the esophagus (H&E stain)
Image by Geoffrey Meyer, PhD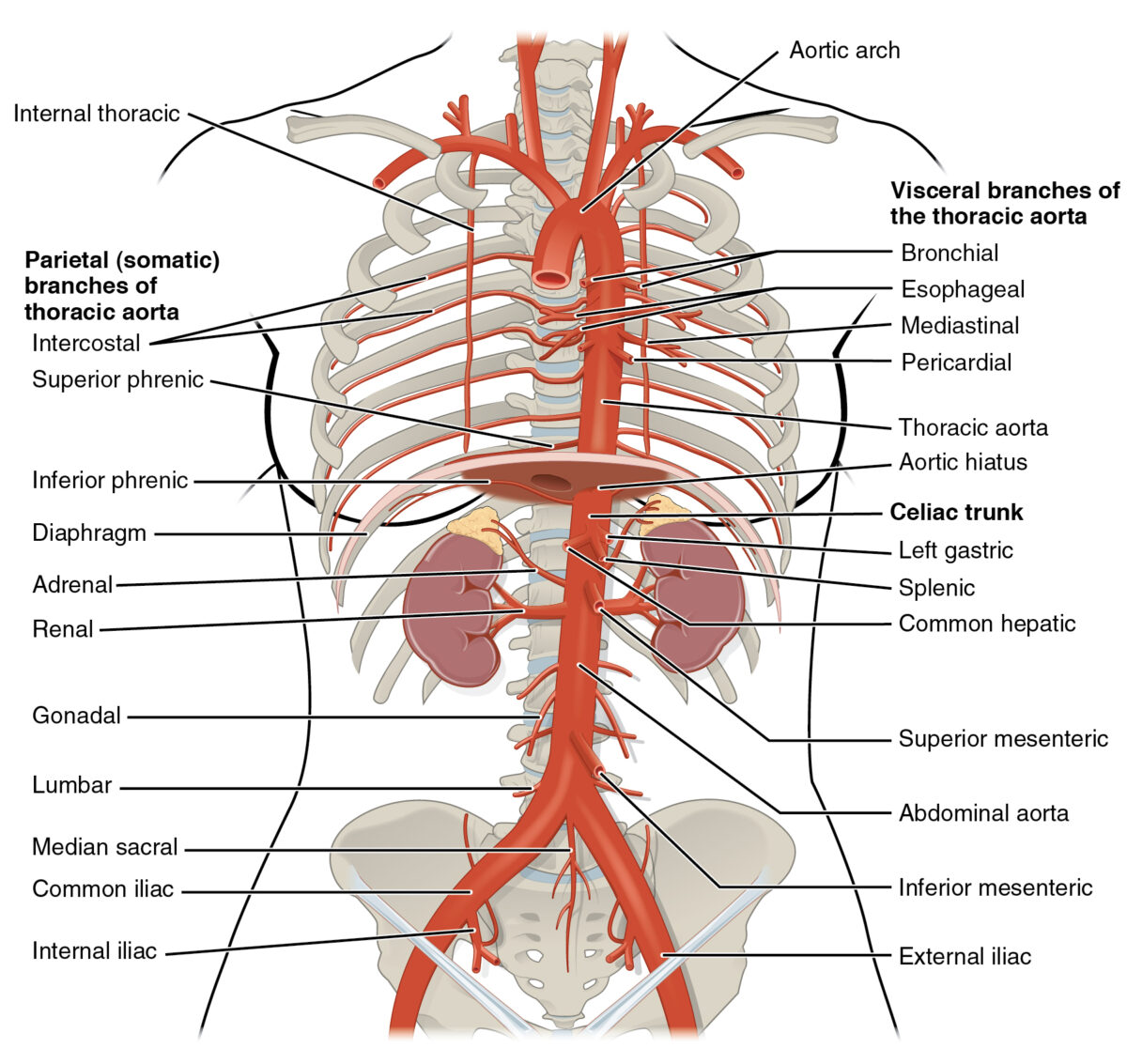
Image displaying some of the arteries responsible for the blood supply of the esophagus
Image: “Thoracic Abdominal Arteries” by OpenStax College. License: CC BY 3.0The primary function of the esophagus is to transport the partially digested food from the pharynx Pharynx The pharynx is a component of the digestive system that lies posterior to the nasal cavity, oral cavity, and larynx. The pharynx can be divided into the oropharynx, nasopharynx, and laryngopharynx. Pharyngeal muscles play an integral role in vital processes such as breathing, swallowing, and speaking. Pharynx: Anatomy to the stomach Stomach The stomach is a muscular sac in the upper left portion of the abdomen that plays a critical role in digestion. The stomach develops from the foregut and connects the esophagus with the duodenum. Structurally, the stomach is C-shaped and forms a greater and lesser curvature and is divided grossly into regions: the cardia, fundus, body, and pylorus. Stomach: Anatomy: