Esophageal cancer is 1 of the most common causes of cancer-related deaths worldwide. Nearly all esophageal cancers are either adenocarcinoma (commonly affecting the distal esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy) or squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC) (affecting the proximal two-thirds of the esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy). Major risk factors for adenocarcinoma include smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity, and Barrett’s esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy. For squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC), risk factors include smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, alcohol consumption, and certain dietary factors. Early-stage cancer is often asymptomatic, with dysphagia Dysphagia Dysphagia is the subjective sensation of difficulty swallowing. Symptoms can range from a complete inability to swallow, to the sensation of solids or liquids becoming "stuck." Dysphagia is classified as either oropharyngeal or esophageal, with esophageal dysphagia having 2 sub-types: functional and mechanical. Dysphagia and weight loss Weight loss Decrease in existing body weight. Bariatric Surgery presenting as the disease progresses. Diagnosis is by endoscopic biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma or image-guided biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma of the metastatic site. Management depends on the disease stage. Options include surgical resection, chemotherapy Chemotherapy Osteosarcoma, and radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma. For unresectable esophageal cancers, palliative measures are provided for symptom relief and to prolong survival.
Last updated: May 22, 2025
| Adenocarcinoma | Squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC) | |
|---|---|---|
| Sex Sex The totality of characteristics of reproductive structure, functions, phenotype, and genotype, differentiating the male from the female organism. Gender Dysphoria | Male | Male |
| Race | Caucasians | African Americans, Asians |
| Major risk factors | Barrett’s esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy, smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity | Smoking Smoking Willful or deliberate act of inhaling and exhaling smoke from burning substances or agents held by hand. Interstitial Lung Diseases, alcohol consumption, low vegetable and fruit intake, drinking hot liquids, caustic strictures, achalasia Achalasia Achalasia is a primary esophageal motility disorder that develops from the degeneration of the myenteric plexus. This condition results in impaired lower esophageal sphincter relaxation and absence of normal esophageal peristalsis. Patients typically present with dysphagia to solids and liquids along with regurgitation. Achalasia |
| Adenocarcinoma | Squamous cell carcinoma Squamous cell carcinoma Cutaneous squamous cell carcinoma (cSCC) is caused by malignant proliferation of atypical keratinocytes. This condition is the 2nd most common skin malignancy and usually affects sun-exposed areas of fair-skinned patients. The cancer presents as a firm, erythematous, keratotic plaque or papule. Squamous Cell Carcinoma (SCC) | |
|---|---|---|
| Location (major distinguishing factor) | Distal ⅓ of esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy Esophagogastric junction Esophagogastric junction The area covering the terminal portion of esophagus and the beginning of stomach at the cardiac orifice. Esophagus: Anatomy (EGJ) | Proximal two-thirds of esophagus Esophagus The esophagus is a muscular tube-shaped organ of around 25 centimeters in length that connects the pharynx to the stomach. The organ extends from approximately the 6th cervical vertebra to the 11th thoracic vertebra and can be divided grossly into 3 parts: the cervical part, the thoracic part, and the abdominal part. Esophagus: Anatomy |
| Early lesions |
|
|
| Advanced lesions | Ulcerated or exophytic Exophytic Retinoblastoma mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast with obstruction | Infiltrating or ulcerated mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast, may be circumferential |
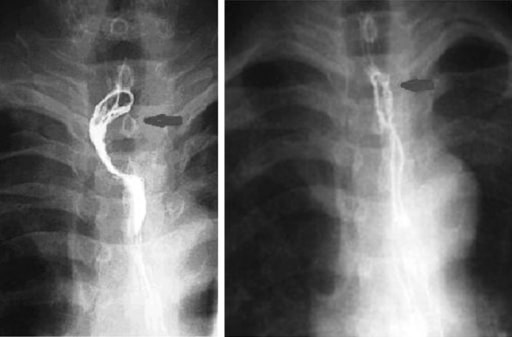
Barium esophagogram: Left image shows an upper esophageal carcinoma (arrow). Right image shows the carcinoma downstaged effectively after neoadjuvant chemotherapy.
Image: “Upper esophageal carcinoma” by Department of Thoracic Surgery, Beijing Tongren Hospital, Capital Medical University, Beijing, China. License: CC BY 4.0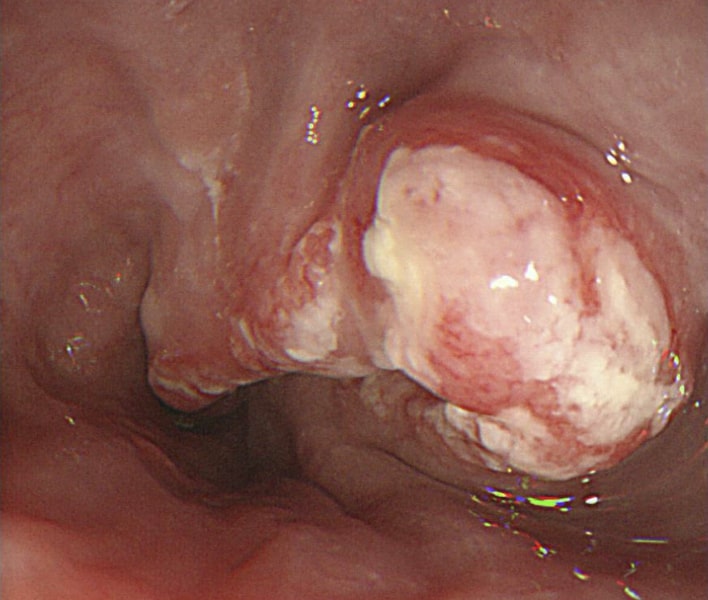
Esophagogastroduodenoscopy (EGD) showing cancer outgrowth (squamous cell carcinoma), causing a narrowing of the lumen
Image: “A Late-Stage Squamous Cell Carcinoma” by Brooks PJ, Enoch M-A, Goldman D, Li T-K, Yokoyama A. License: C BY 2.5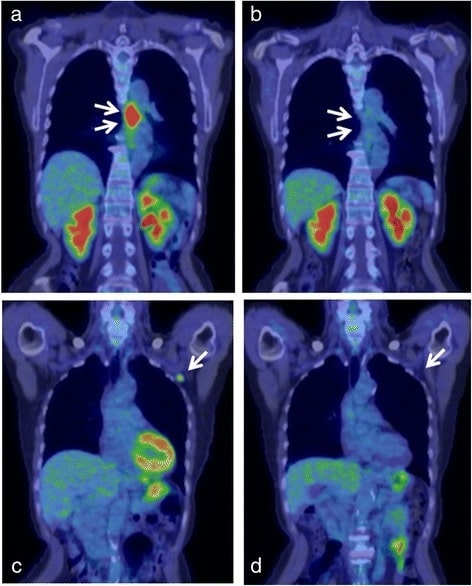
PET–CT findings of esophageal cancer.
a. PET–CT scan showing accumulation in the middle esophagus, representing the squamous cell carcinoma (arrows).
b. PET–CT scan after 4 courses of chemotherapy showing the disappearance of accumulation in the primary tumor (arrows).
c. PET–CT scan showing accumulation in the left axillary lymph node (arrow).
d. PET–CT scan after 4 courses of treatment showing the disappearance of accumulation in the left axillary lymph node (arrow).
Tumor Tumor Inflammation, node, metastasis Metastasis The transfer of a neoplasm from one organ or part of the body to another remote from the primary site. Grading, Staging, and Metastasis (TNM) staging Staging Methods which attempt to express in replicable terms the extent of the neoplasm in the patient. Grading, Staging, and Metastasis:
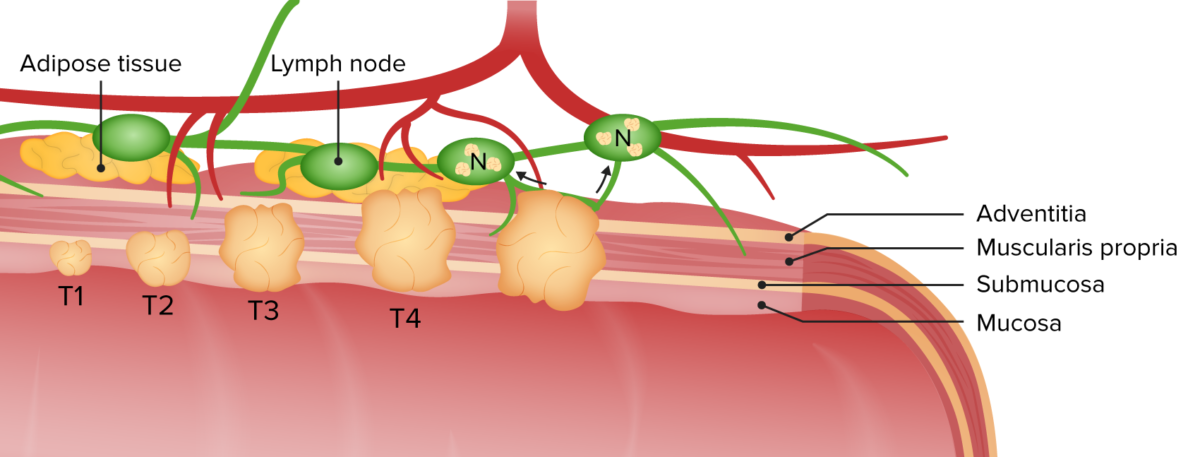
Locoregional esophageal cancer staging: The cancer is seen as the lesion penetrating the esophageal wall. Illustration depicts the staging from T1 (mucosa and submucosa) to advanced disease, involving adjacent structures in T4 and the lymph nodes (N).
Image by Lecturio.