Seborrheic keratosis (SK) is the most common benign Benign Fibroadenoma epithelial cutaneous neoplasm. The condition consists of immature keratinocytes Keratinocytes Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Skin: Structure and Functions. Seborrheic keratosis is the most common benign Benign Fibroadenoma skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions tumor Tumor Inflammation in middle-aged and elderly adults and presents as a sharply demarcated, exophytic Exophytic Retinoblastoma, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesion that may be tan or black and has a “stuck-on” appearance. Pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema) or pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can occur if these lesions become secondarily inflamed by trauma, especially if they are within the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions folds. Genetics Genetics Genetics is the study of genes and their functions and behaviors. Basic Terms of Genetics are thought to play a role, but the pathogenesis is uncertain. The most common mutations involve two oncogenes Oncogenes Genes whose gain-of-function alterations lead to neoplastic cell transformation. They include, for example, genes for activators or stimulators of cell proliferation such as growth factors, growth factor receptors, protein kinases, signal transducers, nuclear phosphoproteins, and transcription factors. A prefix of 'v-' before oncogene symbols indicates oncogenes captured and transmitted by retroviruses; the prefix 'c-' before the gene symbol of an oncogene indicates it is the cellular homolog (proto-oncogenes) of a v-oncogene. Carcinogenesis: fibroblast growth factor Fibroblast growth factor A family of small polypeptide growth factors that share several common features including a strong affinity for heparin, and a central barrel-shaped core region of 140 amino acids that is highly homologous between family members. Although originally studied as proteins that stimulate the growth of fibroblasts this distinction is no longer a requirement for membership in the fibroblast growth factor family. X-linked Hypophosphatemic Rickets receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors 3 (FGFR3) and PIK3CA. There is a familial predisposition to develop a high number of seborrheic keratoses. Treatment is not necessary, as this is a benign Benign Fibroadenoma condition, but cryotherapy Cryotherapy A form of therapy consisting in the local or general use of cold. The selective destruction of tissue by extreme cold or freezing is cryosurgery. Chondrosarcoma, curettage Curettage A scraping, usually of the interior of a cavity or tract, for removal of new growth or other abnormal tissue, or to obtain material for tissue diagnosis. It is performed with a curet (curette), a spoon-shaped instrument designed for that purpose. Benign Bone Tumors or electrodesiccation can be performed for discomfort or cosmetic concerns.
Last updated: Dec 21, 2022
Seborrheic keratosis (SK) is a benign Benign Fibroadenoma skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions tumor Tumor Inflammation consisting of proliferating immature keratinocytes Keratinocytes Epidermal cells which synthesize keratin and undergo characteristic changes as they move upward from the basal layers of the epidermis to the cornified (horny) layer of the skin. Successive stages of differentiation of the keratinocytes forming the epidermal layers are basal cell, spinous or prickle cell, and the granular cell. Skin: Structure and Functions.
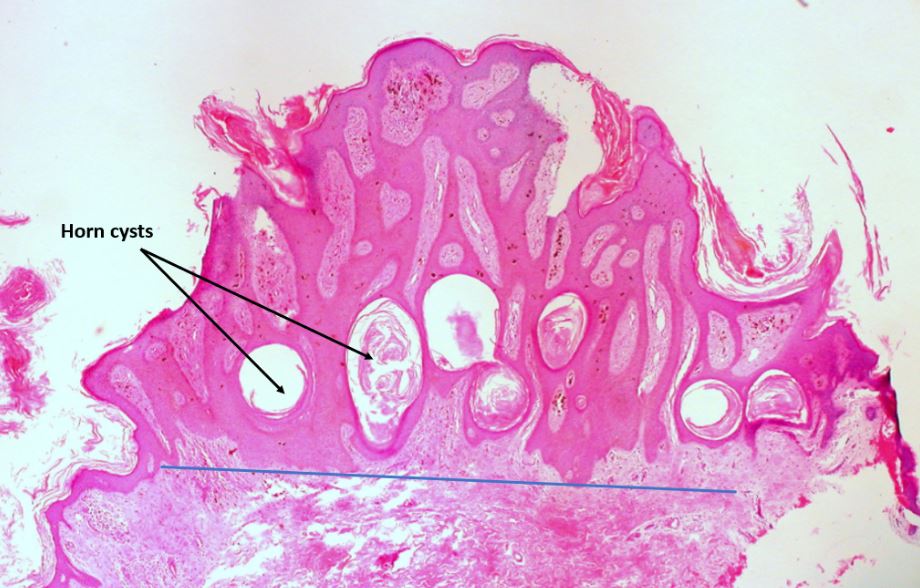
Pigmented seborrheic keratosis of the vulva:
Note the domed shape, sharp circumscription from the surrounding skin, horn cysts, and the brown melanin pigment within the epidermis and in the adjacent dermis (within macrophages).
The blue line below the lesion demonstrates the “string sign” of SK seen at low-power magnification: A horizontal line can be drawn parallel to the epidermal surface underlying the lesion because the SK extends uniformly to one depth.
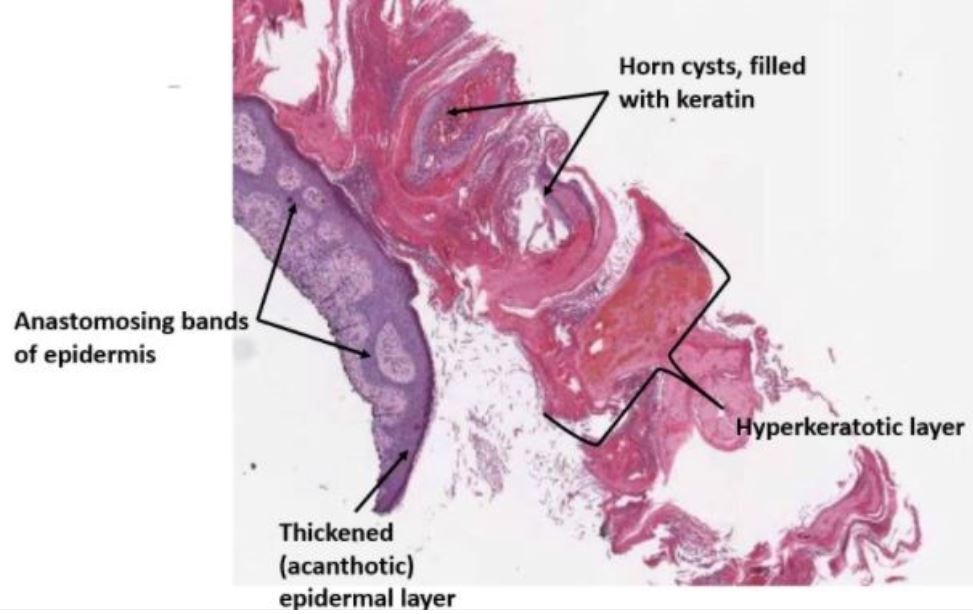
Low-power microphotograph of a shave biopsy of a hyperkeratotic seborrheic keratosis showing the superficial pink-staining keratinous material partially detached from the surface.
Note the thickened epidermis with anastomosing strands of proliferating basaloid cells within the epidermis.

Seborrheic keratosis with rough surface:
Note the typical waxy appearance, the well-circumscribed border, and the superficial stuck-on appearance.
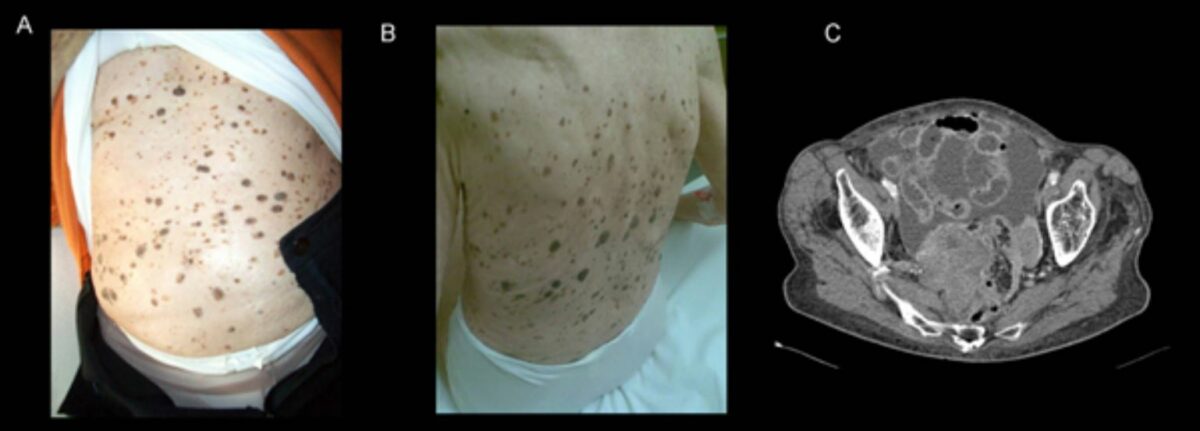
A and B: Leser–Trélat sign in a 92-year-old woman with advanced ovarian cancer. Multiple eruptive seborrheic keratoses had dramatically increased in size and number over the previous 2 years.
C: CT scan showing a necrotic ovarian tumor accompanied by signs of peritoneal carcinomatosis
Physical exam:
Dermoscopy:
Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma: