Melanoma is a malignant tumor Tumor Inflammation arising from melanocytes Melanocytes Mammalian pigment cells that produce melanins, pigments found mainly in the epidermis, but also in the eyes and the hair, by a process called melanogenesis. Coloration can be altered by the number of melanocytes or the amount of pigment produced and stored in the organelles called melanosomes. The large non-mammalian melanin-containing cells are called melanophores. Skin: Structure and Functions, the melanin-producing cells of the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions. These tumors are most common in fair-skinned individuals with a history of excessive sun exposure and sunburns. Melanomas usually present as pigmented skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions lesions, but they can occur on mucosal surfaces, such as in the eyes, anal canal, and genital regions. Common findings may include Asymmetry of the lesion, irregular Border, varying Color, > 6 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma Diameter, and Evolving features (ABCDE). Definitive diagnosis is established with biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma. Treatment relies primarily on surgical excision. The prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is very good for early-stage lesions but quite dismal for metastatic disease. Of all the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions malignancies, melanoma generally carries the worst prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas.
Last updated: May 17, 2024
Melanoma is a malignant tumor Tumor Inflammation arising from melanocytes Melanocytes Mammalian pigment cells that produce melanins, pigments found mainly in the epidermis, but also in the eyes and the hair, by a process called melanogenesis. Coloration can be altered by the number of melanocytes or the amount of pigment produced and stored in the organelles called melanosomes. The large non-mammalian melanin-containing cells are called melanophores. Skin: Structure and Functions, the melanin-producing cells of the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions.
Major types:
| Types | Frequency | Growth | Morphology | Common sites |
|---|---|---|---|---|
| Superficial spreading melanoma | 60%–75% |
|
|
|
| Nodular melanoma | 15%–30% |
|
||
| Lentigo maligna Lentigo Maligna Lentigo maligna is melanoma in situ, a precancerous lesion that may progress to an invasive melanoma (specifically lentigo maligna melanoma subtype). This condition typically occurs in sun-damaged areas (e.g., face and neck) of elderly patients. Lentigo Maligna melanoma | 10% |
|
|
|
| Acral lentiginous melanoma | < 5%; most common type in Asian and dark-skinned individuals |
|
|
|
Uncommon variants:
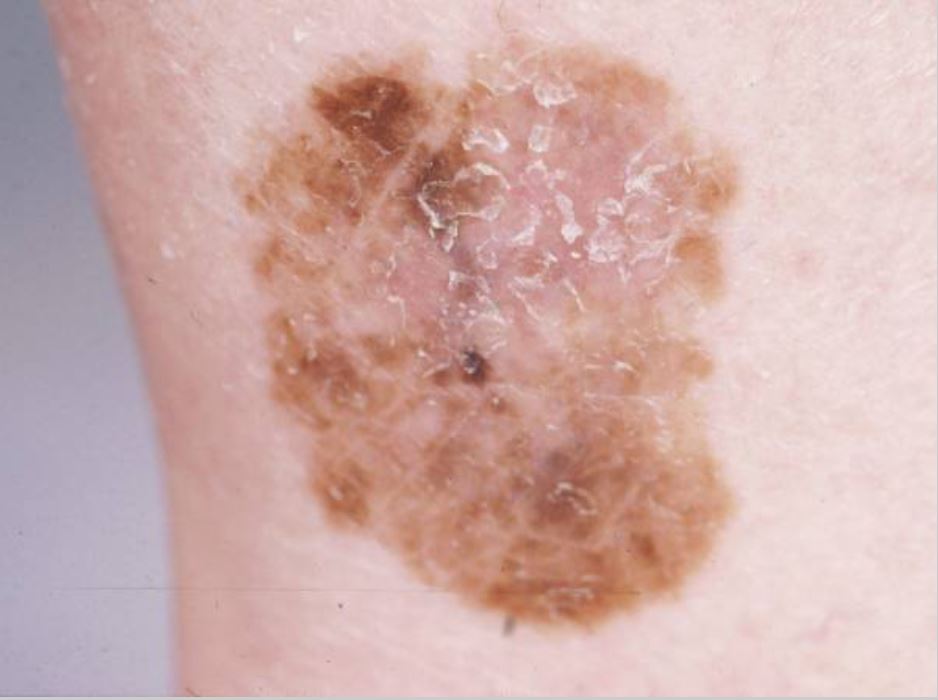
Superficial spreading melanoma: most common type: This melanoma is flat and has horizontal growth and variable pigmentation. Image: “Dermoscopy as a technique for the early identification of foot melanoma” by Bristow IR, Bowling J. License: CC BY 2.0

Multiple large nodular melanomas:
Photograph of the face (A) and the upper back (B) of a woman presenting with multiple large nodular melanomas

Lentigo maligna melanoma on the left cheek:
A 2 x 1 cm brown patch is observed on the patient’s left cheek.

Acral lentiginous melanoma of the foot
Image: “Dermoscopy as a technique for the early identification of foot melanoma” by Bristow IR, Bowling J License: CC BY 2.0Breslow depth:
| Breslow stage | Tumor Tumor Inflammation thickness |
|---|---|
| Stage 1 Stage 1 Trypanosoma brucei/African trypanosomiasis | ≤ 1 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma |
| Stage 2 | 1–2 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma |
| Stage 3 | > 2–4 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma |
| Stage 4 | > 4 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma |

Cutaneous melanoma
Image: “Melanoma” by National Cancer Institute. License: Public Domain
Uveal melanoma showing dark-brown pigments with diffuse extrascleral extension
Image: “Pancreatic metastases from ocular malignant melanoma: the use of endoscopic ultrasound-guided fine-needle aspiration to establish a definitive cytologic diagnosis” by Journal of Medical Case Reports. License: CC BY 4.0Adjunctive studies are used for evaluation of metastatic disease.
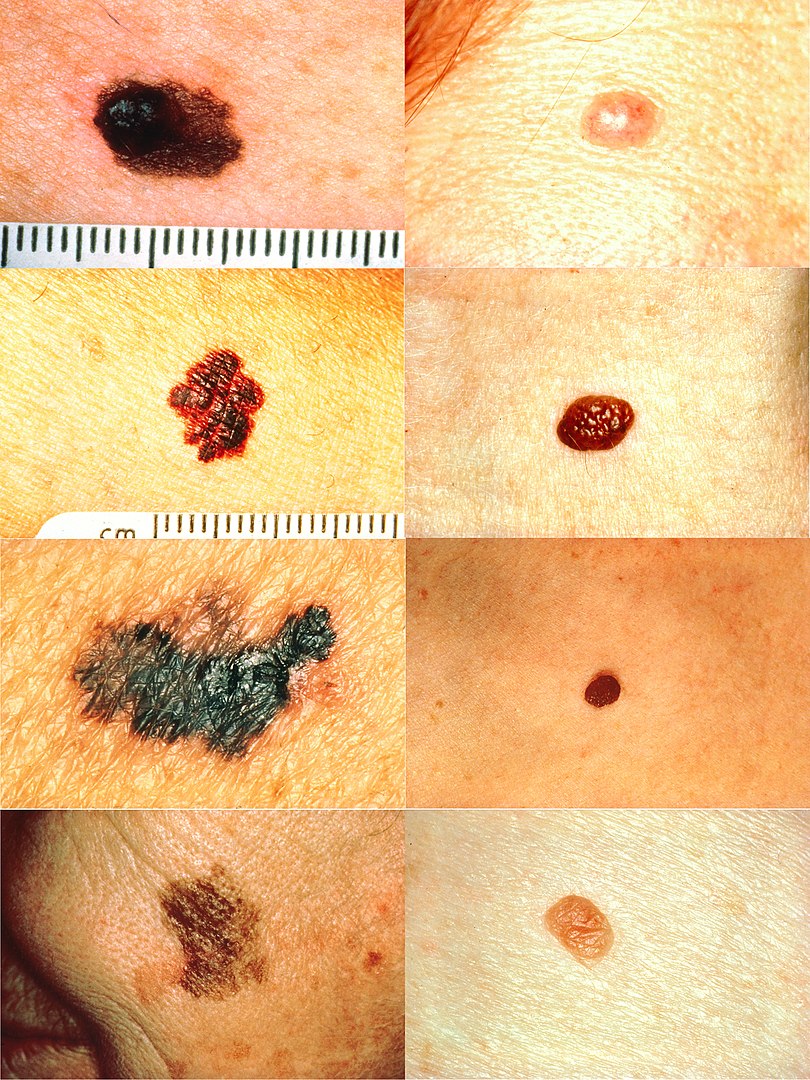
Part of the ABCDs for detection of melanoma:
In the left column (top to bottom): melanomas showing (A) asymmetry; (B) a border that is uneven, ragged, or notched; (C) coloring of different shades of brown, black, or tan; and (D) diameter that has changed in size. In the right column (top to bottom): Normal moles do not have abnormal characteristics (all lesions have no asymmetry or change in diameter and have even border and color).
| TNM | Description | Substages |
|---|---|---|
| Tumor Tumor Inflammation (T) |
|
|
| Lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node (N) |
|
|
| Metastases (M) |
|
|
| Stage | Tumor Tumor Inflammation (T) | Lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node (N) | Metastases (M) |
|---|---|---|---|
| 0 | Tis | N0 | M0 |
| IA | T1a | N0 | M0 |
| IB | T2a, T1b | N0 | M0 |
| IIA | T2b, T3a | N0 | M0 |
| IIB | T3b, T4a | N0 | M0 |
| IIC | T4b | N0 | M0 |
| III | Any T | ≥ N1 | M0 |
| IV | Any T | Any N | M1 |
Wide local excision:
Mohs micrographic surgery:
| Invasion depth | Tumor Tumor Inflammation stage | Margins |
|---|---|---|
| Tis | 0.51 cm | |
| 1 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma | T1 | 1 cm |
| > 1–2 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma | T2 | 1–2 cm |
| > 2–4 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma | T3 T3 A T3 thyroid hormone normally synthesized and secreted by the thyroid gland in much smaller quantities than thyroxine (T4). Most T3 is derived from peripheral monodeiodination of T4 at the 5′ position of the outer ring of the iodothyronine nucleus. The hormone finally delivered and used by the tissues is mainly t3. Thyroid Hormones | 2 cm |
| > 4 mm MM Multiple myeloma (MM) is a malignant condition of plasma cells (activated B lymphocytes) primarily seen in the elderly. Monoclonal proliferation of plasma cells results in cytokine-driven osteoclastic activity and excessive secretion of IgG antibodies. Multiple Myeloma | T4 T4 The major hormone derived from the thyroid gland. Thyroxine is synthesized via the iodination of tyrosines (monoiodotyrosine) and the coupling of iodotyrosines (diiodotyrosine) in the thyroglobulin. Thyroxine is released from thyroglobulin by proteolysis and secreted into the blood. Thyroxine is peripherally deiodinated to form triiodothyronine which exerts a broad spectrum of stimulatory effects on cell metabolism. Thyroid Hormones |
Sentinel lymph node biopsy Lymph Node Biopsy Lymphadenopathy (SLNB):
Regional lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node dissection:
Surgical metastasectomy Metastasectomy Surgery to remove one or more neoplasm metastases. Hepatocellular Carcinoma (HCC) and Liver Metastases:
Negative prognostic factors:
5-year survival rate: