The secondary lymphoid organs Lymphoid organs A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs, also called peripheral lymphoid/lymphatic organs, include MALT MALT Colon, Cecum, and Appendix: Anatomy, the lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy, and the spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy. These collections of lymphoid tissues provide constant surveillance Surveillance Developmental Milestones and Normal Growth for pathogens. In their distinct sites, these tissues are filled with immune cells ready to mount a response when antigens are detected. Lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 - 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy are seen along lymphatic vessels Lymphatic Vessels Tubular vessels that are involved in the transport of lymph and lymphocytes. Lymphatic Drainage System: Anatomy and occur as chains or groups ( neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess, groin Groin The external junctural region between the lower part of the abdomen and the thigh. Male Genitourinary Examination, axillae, mesenteries, abdomen). MALTs act as immune sensors situated in locations where the lumen is exposed to the external environment ( oropharynx Oropharynx The middle portion of the pharynx that lies posterior to the mouth, inferior to the soft palate, and superior to the base of the tongue and epiglottis. It has a digestive function as food passes from the mouth into the oropharynx before entering esophagus. Pharynx: Anatomy, GI tract, genitourinary tract). The spleen Spleen The spleen is the largest lymphoid organ in the body, located in the LUQ of the abdomen, superior to the left kidney and posterior to the stomach at the level of the 9th-11th ribs just below the diaphragm. The spleen is highly vascular and acts as an important blood filter, cleansing the blood of pathogens and damaged erythrocytes. Spleen: Anatomy is the site of production of antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions and lymphocytes Lymphocytes Lymphocytes are heterogeneous WBCs involved in immune response. Lymphocytes develop from the bone marrow, starting from hematopoietic stem cells (HSCs) and progressing to common lymphoid progenitors (CLPs). B and T lymphocytes and natural killer (NK) cells arise from the lineage. Lymphocytes: Histology, but it also aids in the breakdown of platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology and erythrocytes Erythrocytes Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology.
Last updated: Mar 31, 2025
The lymphatic system Lymphatic system A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs ( lymph vessels Lymph vessels Tubular vessels that are involved in the transport of lymph and lymphocytes. Lymphatic Drainage System: Anatomy, lymph fluid Lymph fluid The interstitial fluid that is in the lymphatic system. Lymphatic Drainage System: Anatomy, and lymphoid organs Lymphoid organs A system of organs and tissues that process and transport immune cells and lymph. Primary Lymphatic Organs) is part of the body’s immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs.
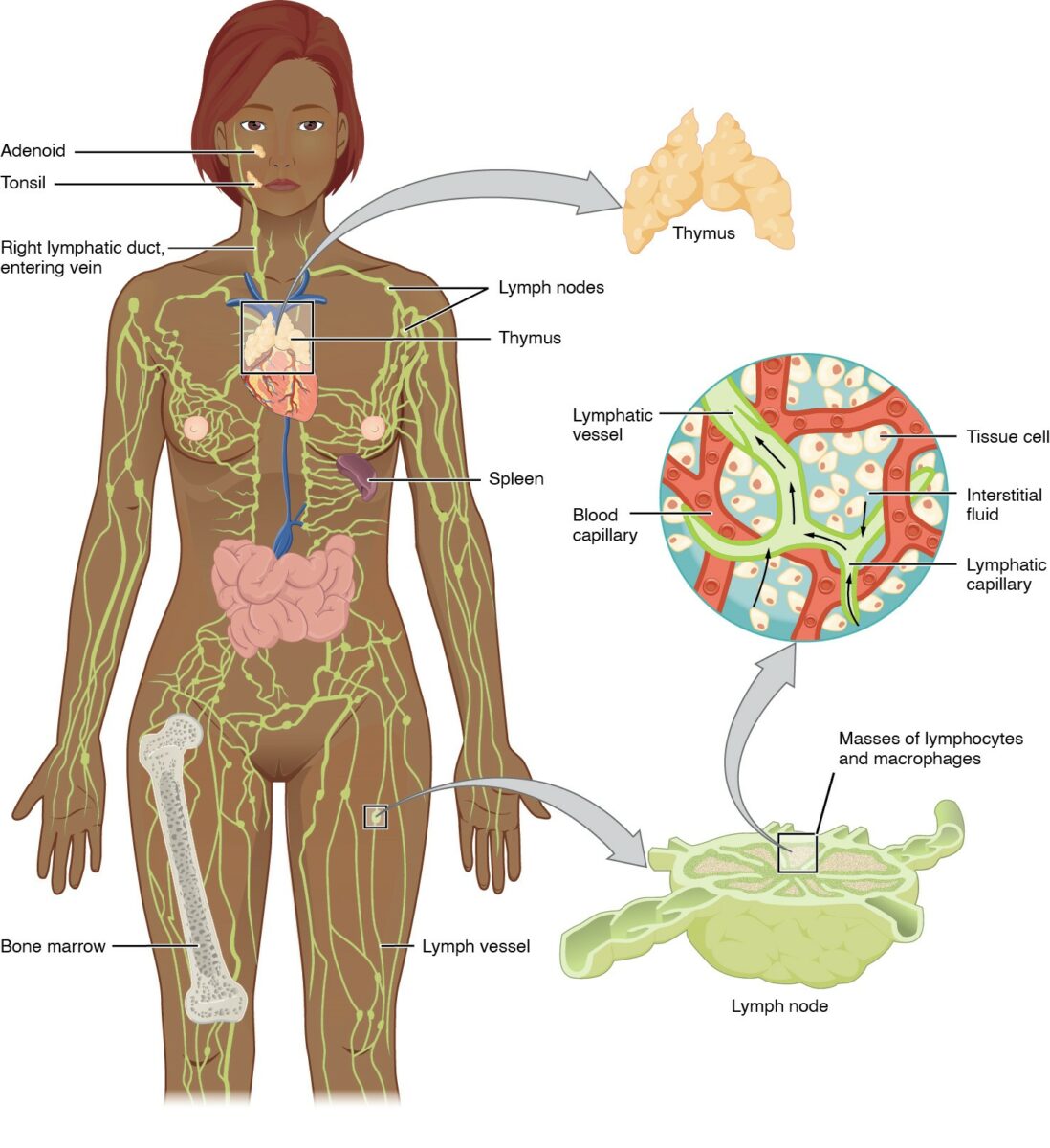
Anatomy of the lymphatic system:
Includes the primary (bone marrow, thymus) and secondary (spleen, lymph nodes, and MALT) lymphoid organs
Lymphatic vessels convey lymph to the larger lymphatic vessels in the torso, transporting fluid back to the venous circulation.
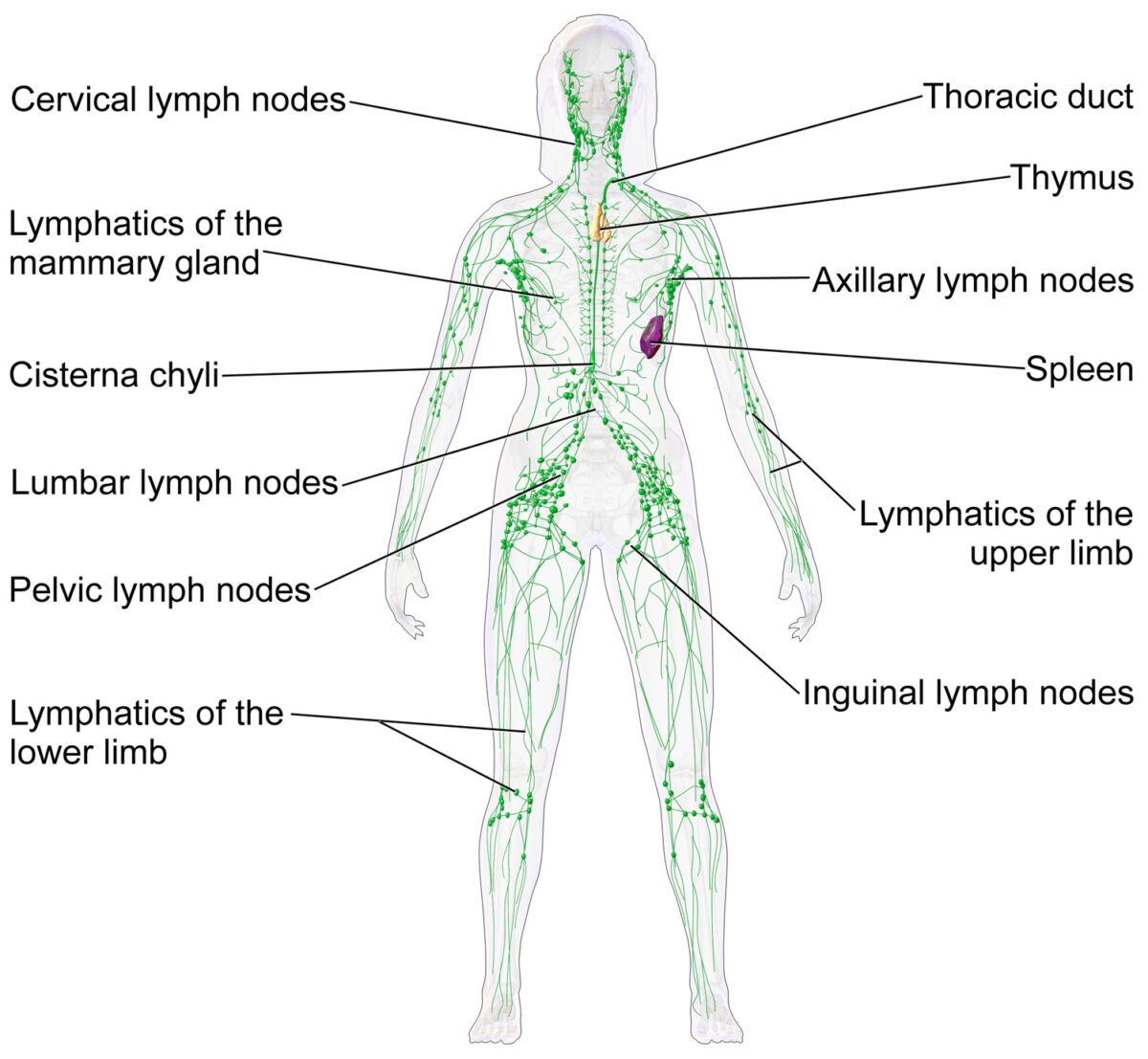
Lymph nodes and the lymphatic system
Image: “Blausen 0623 LymphaticSystem Female” by Blausen. License: CC BY 3.0The main function of lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy is defense against the spread of microorganisms and tumor Tumor Inflammation cells:
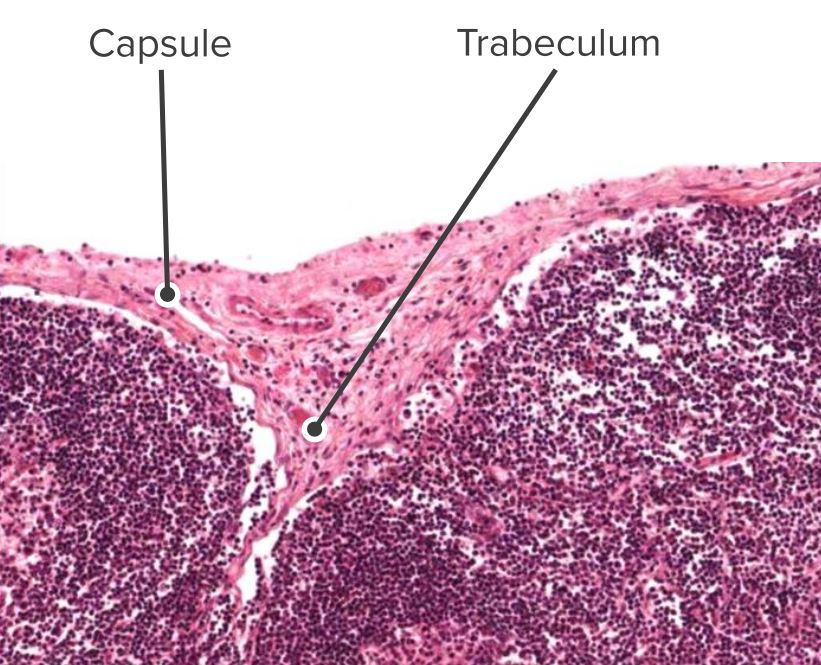
Histologic section of a lymph node, identifying the capsule and the trabeculae
Image by Geoffrey Meyer, edited by Lecturio.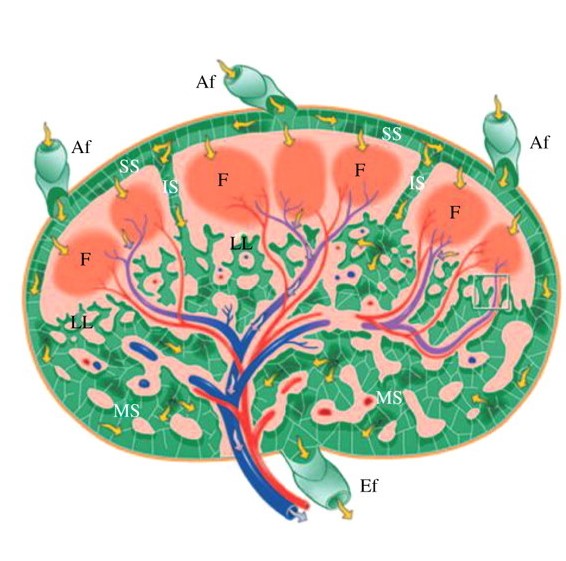
Illustration of a lymph node cross section:
Red and blue denote arteries and veins, respectively. Yellow arrows indicate lymph flow.
Af: afferent vessels
Ef: efferent vessels
F: follicle
IS: intermediate sinuses
LL: lymphatic labyrinth
MS: medullary sinuses
SS: subcapsular sinuses
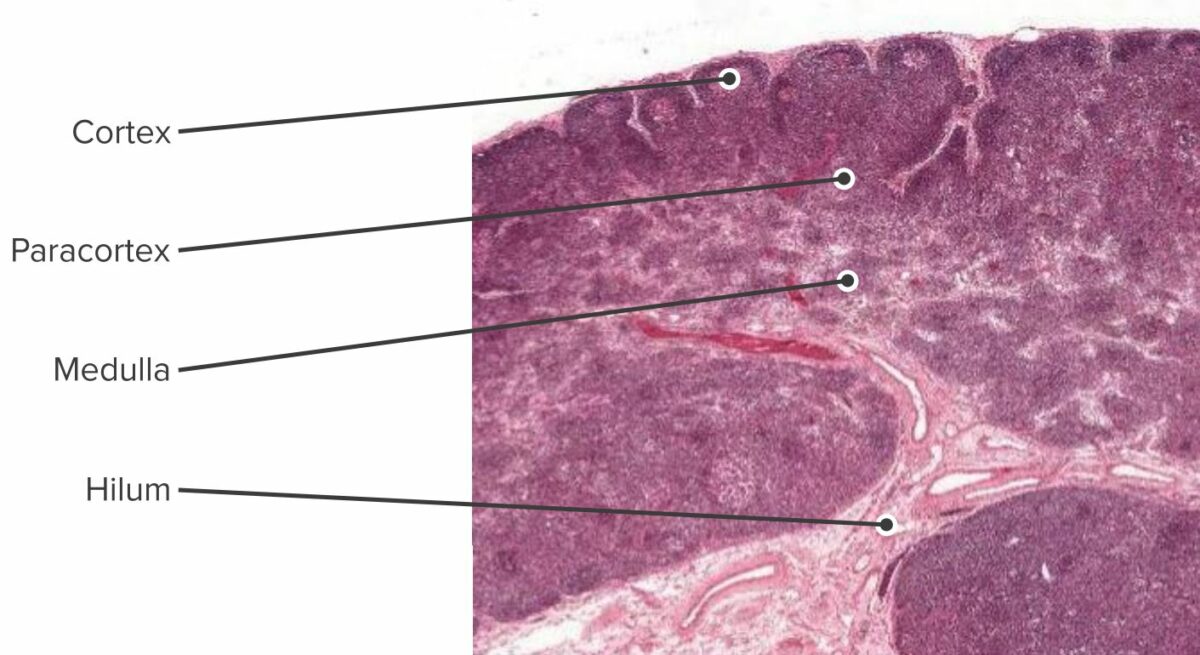
Histologic section of the lymph node showing the cortex, paracortex, and medulla
Image by Geoffrey Meyer, edited by Lecturio.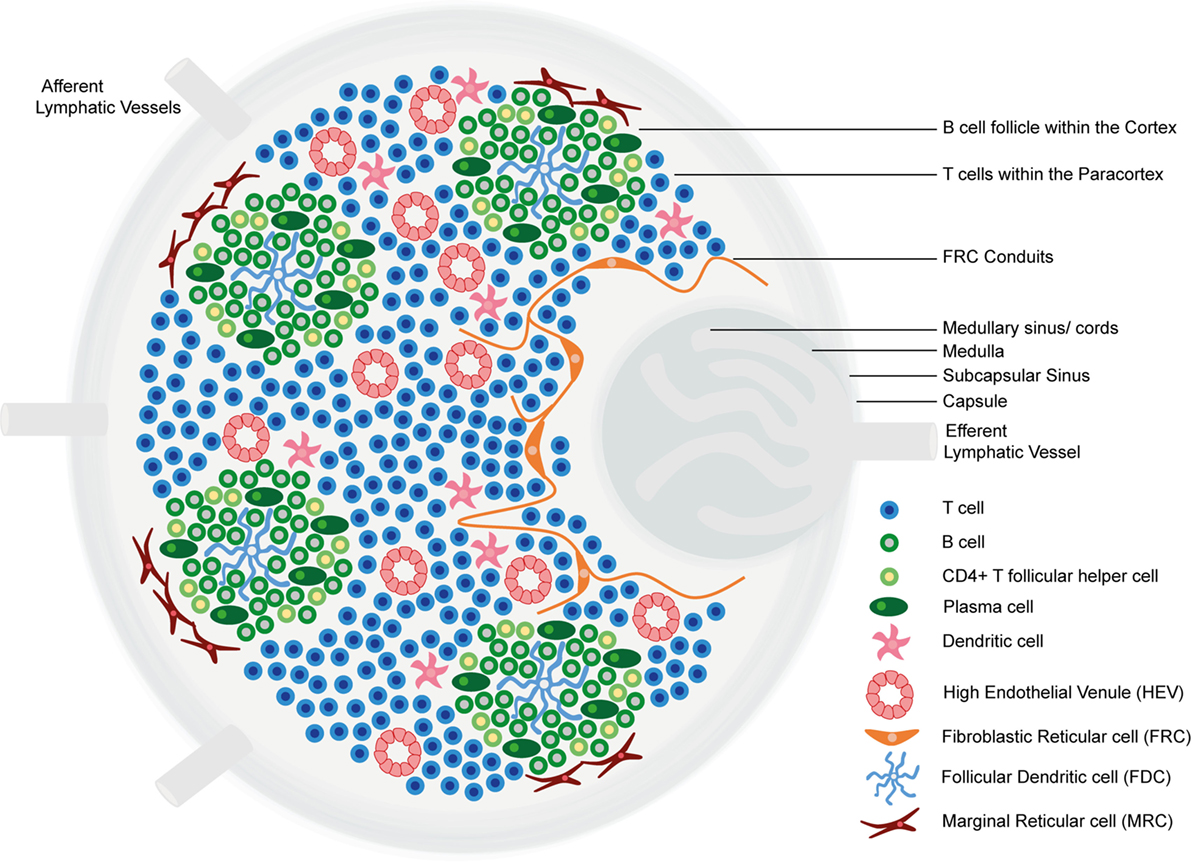
Structure and functional regions of a lymph node comprising a collagen-rich fibrous capsule and an underlying subcapsular sinus (SCS).
Cells are segregated into (1) the cortex (consisting of B cells, T follicular helper cells, and follicular dendritic cells arranged in primary follicles, in which B cells survey antigens presented on the follicular dendritic cell stromal network); and (2) the paracortex (accommodates T cells, dendritic cells, and fibroblastic reticular cells, which form stromal cell networks and reticular fibers).
The inner medulla is composed of lymphatic tissues (medullary cords) separated by medullary sinuses consisting of lymph.
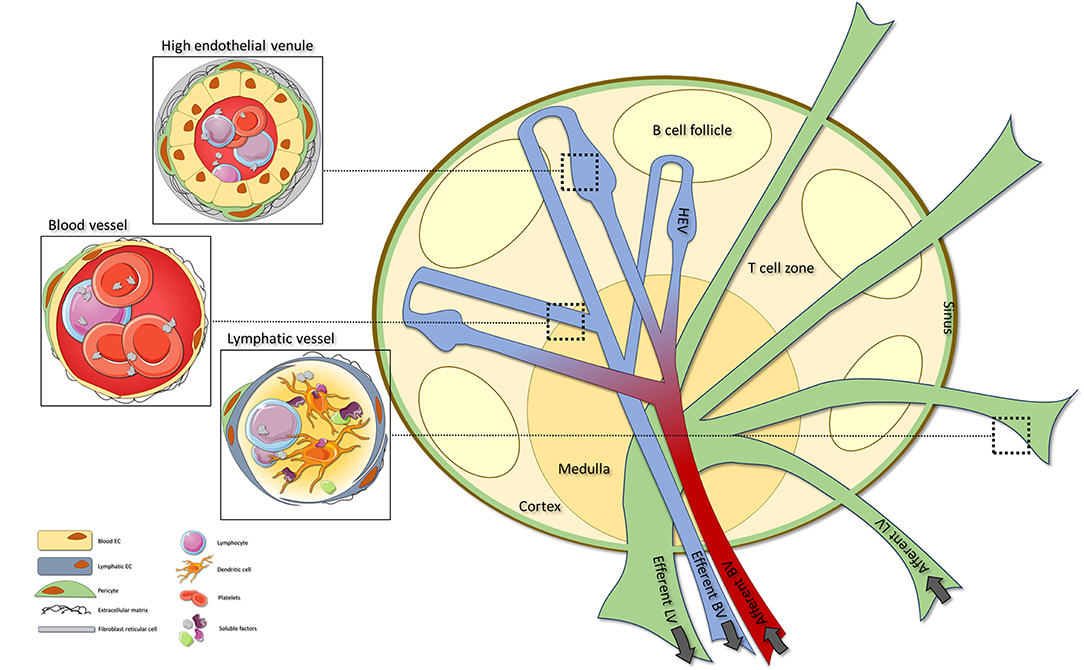
Lymph node vascular structure:
Consists of blood vessels (BVs), high endothelial venules (HEVs), and lymphatic vessels (LVs).
Blood vessels can be found throughout the whole lymph node, with specialized HEVs located within the T-cell areas. High endothelial venules are specialized BVs that orchestrate extravasation of lymphocytes into the lymph node. Afferent LVs enter the lymph node, where they transit into sinuses that ultimately exit via the efferent LV.
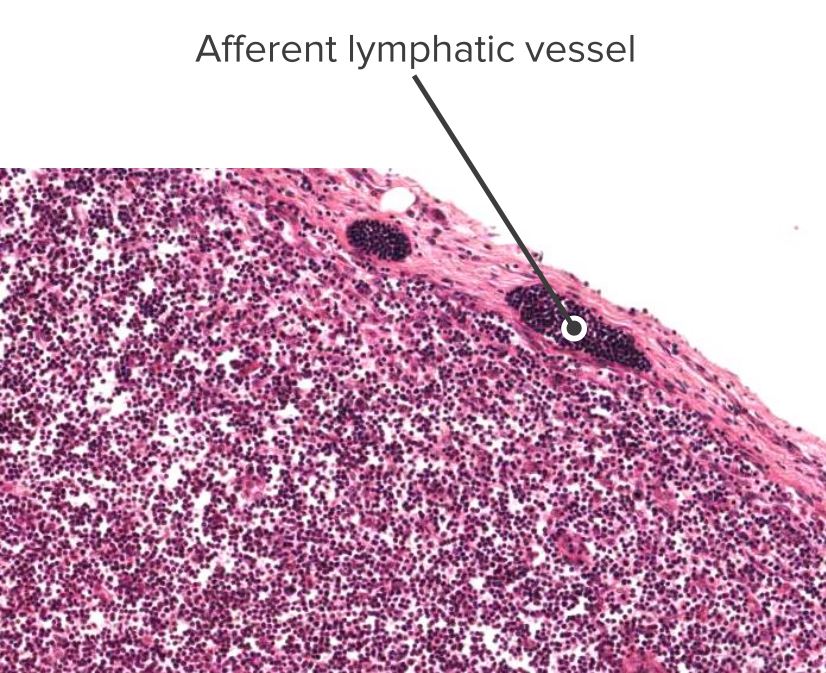
Histologic section of a lymph node showing an afferent vessel
Image by Geoffrey Meyer, edited by Lecturio.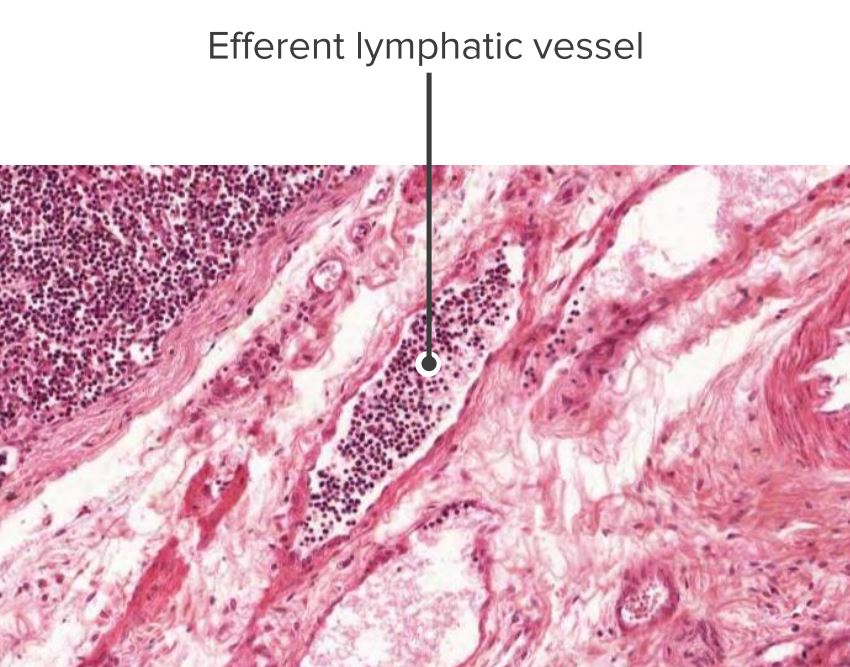
Histologic section of a lymph node showing an efferent vessel
Image by Geoffrey Meyer, edited by Lecturio.Mount an immune response against pathogens encountered in the mucosa of the GI, respiratory, and genitourinary tracts.
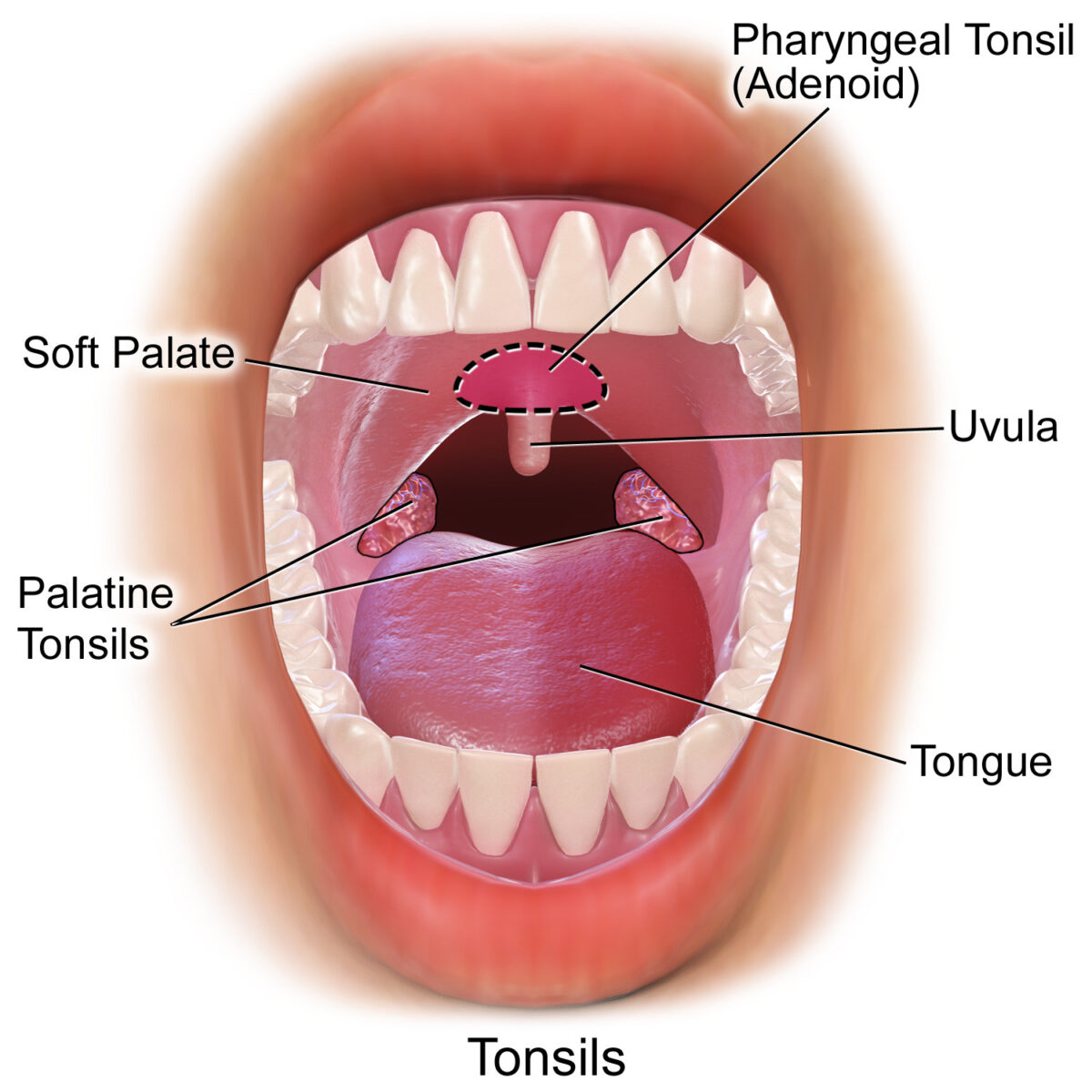
Tonsils in the oropharyngeal area, front view:
Pharyngeal, palatine and lingual tonsils
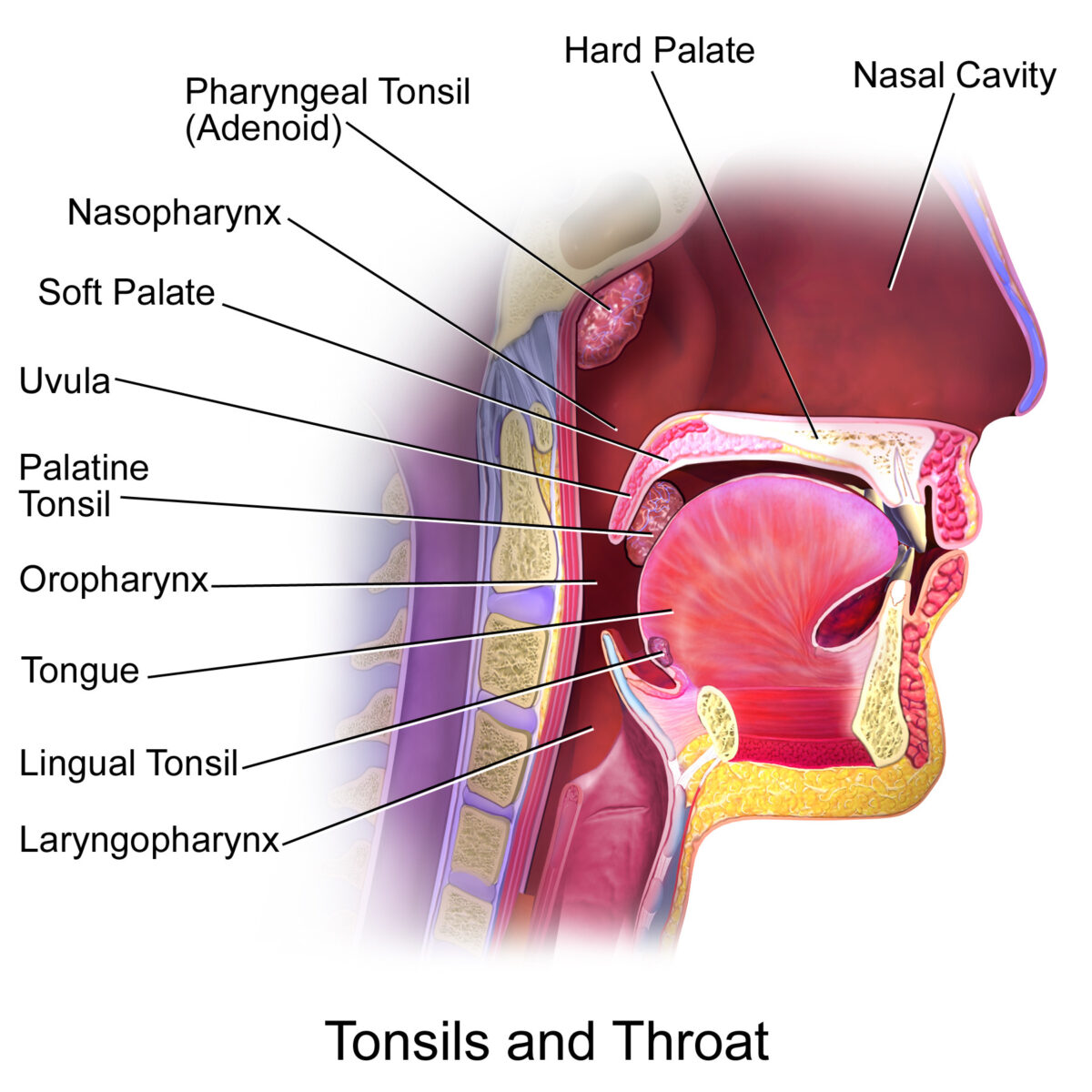
Tonsils in the oropharyngeal area, side view:
Pharyngeal, palatine, and lingual tonsils.
The tubal tonsils (not pictured) are in the area of the nasopharynx.
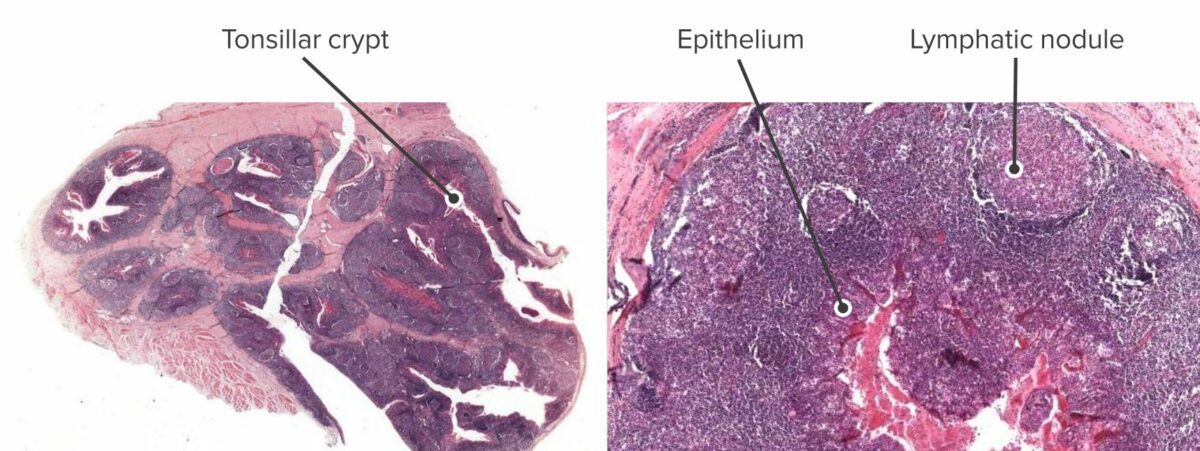
Cross section of a tonsil (left) and close up of the bottom of a tonsillar crypt (right).
On the right, a lymphatic nodule (activated lymphoid tissue) can be seen very close to the bottom of the crypt.
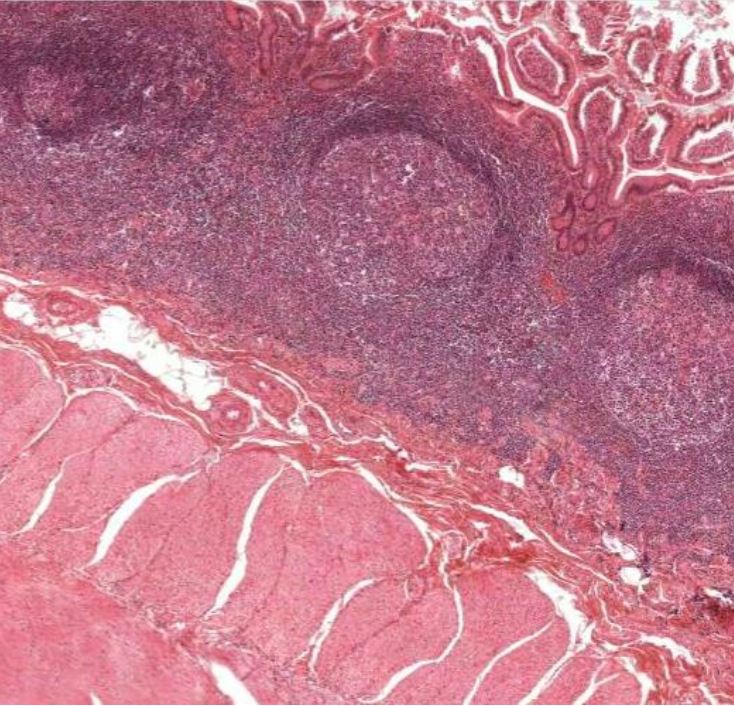
Histologic section of the ileum showing Peyer’s patches
Image by Geoffrey Meyer.
Cross section of an appendix:
Lymphoid nodules can be seen reacting to an antigen from the lumen.
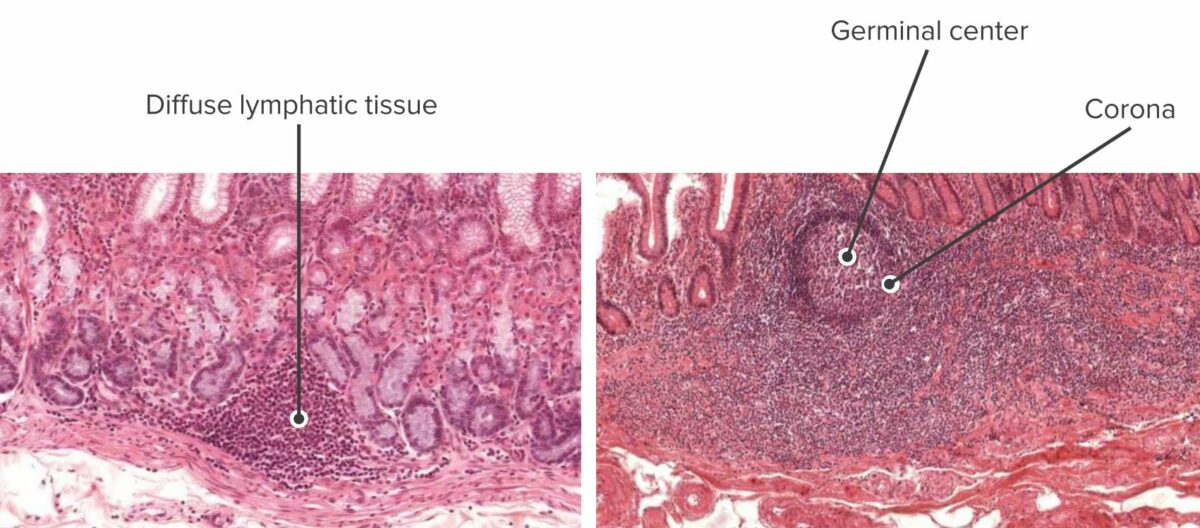
Cross section of stomach mucosa showing inactive lymphoid tissue (left) and cross section of intestine mucosa showing active lymphoid tissue (right):
Lymphoid tissues stand guard until they are activated and form nodules, with germinal centers.
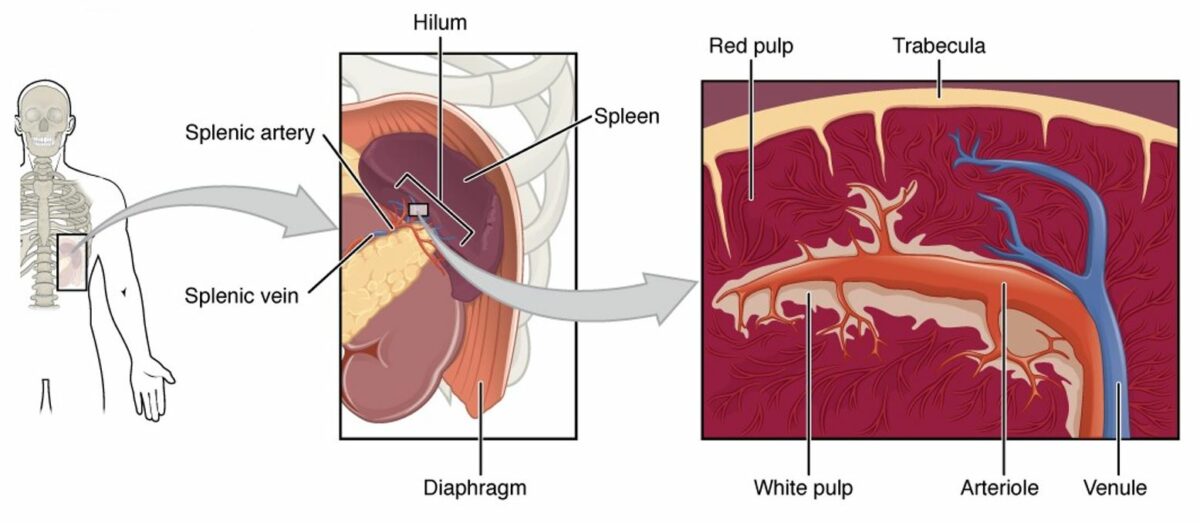
Diagram of the spleen (from left to right):
The spleen is a highly vascularized organ in the LUQ of the abdomen.
The hilum is the area where the splenic artery enters and the splenic vein leaves the spleen. A cross section of the spleen would show that the majority of the splenic parenchyma contains the red pulp (filled with all types of blood cells). The white pulp contains mainly lymphoid nodules and the periarteriolar lymphoid sheaths (PALS), which surround the central arteriole.
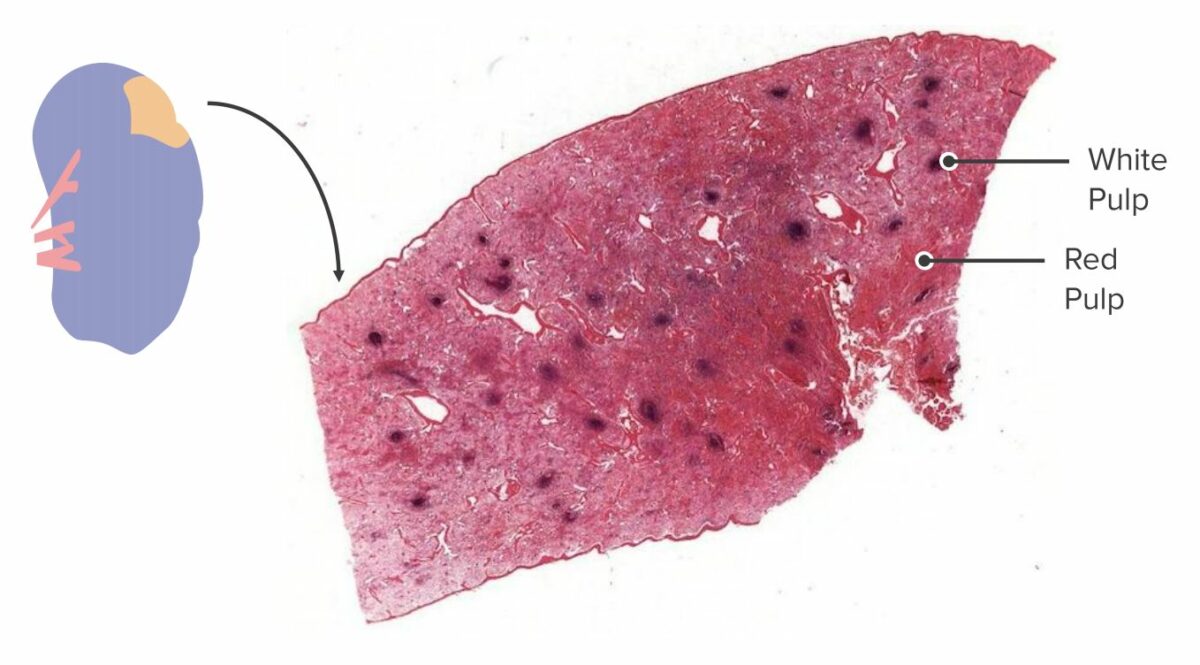
Cross section of a spleen:
In a gross specimen, the white pulp and red pulp can be identified and differentiated owing to their difference in color and placement. White pulp agglomerates around blood vessels, while red pulp makes up the rest of the parenchyma.

Histologic section of the spleen:
The periarterial lymphoid sheath (PALS) engulfs a central arteriole. A lymphoid nodule has formed, surrounded by T cells, indicating that an antigen was detected in the splenic blood supply and an immune response was initiated.