Lymphadenopathy is lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node enlargement (> 1 cm) and is benign Benign Fibroadenoma and self-limited in most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Etiologies include malignancy Malignancy Hemothorax, infection, and autoimmune disorders, as well as iatrogenic Iatrogenic Any adverse condition in a patient occurring as the result of treatment by a physician, surgeon, or other health professional, especially infections acquired by a patient during the course of treatment. Anterior Cord Syndrome causes such as the use of certain medications. Generalized lymphadenopathy often indicates underlying systemic disease. Diagnosis relies on a thorough medical history and physical examination, which usually identify the underlying cause. When the cause is unknown, a biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma may be necessary. Management is directed at the underlying infection, malignancy Malignancy Hemothorax, or other cause.
Last updated: Jan 10, 2023
Lymphadenopathy is lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node enlargement of usually > 1 cm. It is considered localized if the enlargement is limited to lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy of 1 anatomic region and generalized when ≥ 2 regions are involved.
Most often, lymphadenopathy is a reaction to a local infection. Less frequently, it may be due to a malignant process or chronic, systemic disease. The following conditions include lymphadenopathy in their clinical presentation:
To recall the various causes of lymphadenopathy, remember MIAMI:
The immune and lymphatic systems are highly interrelated. Lymphocytes Lymphocytes Lymphocytes are heterogeneous WBCs involved in immune response. Lymphocytes develop from the bone marrow, starting from hematopoietic stem cells (HSCs) and progressing to common lymphoid progenitors (CLPs). B and T lymphocytes and natural killer (NK) cells arise from the lineage. Lymphocytes: Histology are transported via the lymphatic vessels Lymphatic Vessels Tubular vessels that are involved in the transport of lymph and lymphocytes. Lymphatic Drainage System: Anatomy to lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy. Humans have about 500–600 lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy throughout the body. Lymphadenopathy, or swelling Swelling Inflammation of lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy, may occur in response to infection, malignancy Malignancy Hemothorax, or chronic disease.
Cells, plasma Plasma The residual portion of blood that is left after removal of blood cells by centrifugation without prior blood coagulation. Transfusion Products, and foreign particles in the interstitial space become lymphatic fluid upon entering the lymphatic vessels Lymphatic Vessels Tubular vessels that are involved in the transport of lymph and lymphocytes. Lymphatic Drainage System: Anatomy. Within the lymph nodes Lymph Nodes They are oval or bean shaped bodies (1 – 30 mm in diameter) located along the lymphatic system. Lymphatic Drainage System: Anatomy, this fluid is filtered of excess fluid and abnormal cells (e.g., infected, malignant, damaged, presenting antigens). This triggers an immune response that involves cellular proliferation, causing the nodes to enlarge (reactive lymphadenopathy).
Lymphadenopathy results from 1 of the pathologic processes:
The signs and symptoms associated with lymphadenopathy will depend on the cause and the type (localized versus generalized).
History:
Physical examination:
Laboratory testing:
Ordered based on the patient’s relevant history and physical exam findings to confirm the suspected diagnosis:
Imaging:
The type of test ordered is guided by history, physical exam, and risk factors.
Lymph Lymph The interstitial fluid that is in the lymphatic system. Secondary Lymphatic Organs node biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma:

Chest X-ray of pulmonary TB showing bilateral hilar lymphadenopathy and patchy opacification on the right upper lung zone and the middle lung zone with fibrotic shadows
Image: “Chest X-ray of patchy opacities of pulmonary tuberculosis” by Basem Abbas Al Ubaidi. License: CC BY 4.0
Axillary lymphadenopathy on thoracic CT with contrast (arrow)
Image: “Axillary-lymphadenopathy-on-CT-thorax-with-contrast” by Yu Zuo, Michelle Foshat, You-wen Qian, Brent Kelly, Brock Harper, Bernard Karnath. License: CC BY 4.0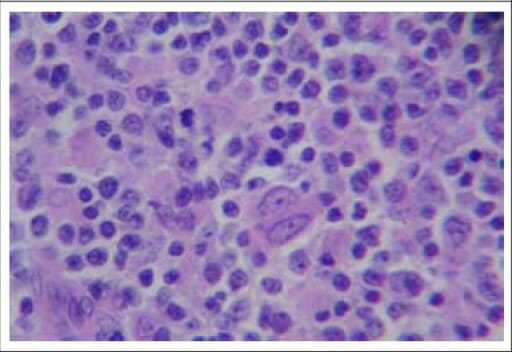
Histopathological picture of a left cervical lymph node showing evidence of non-Hodgkin lymphoma (H&E stain, 400x)
Image: “F2: Histopathological picture of left cervical lymph node showing evidence of non-Hodgkin lymphoma (H&E stain, ×400)” by Sudipta Pandit et al. License: CC BY 2.5