Rhinitis refers to inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the nasal mucosa Nasal mucosa The mucous lining of the nasal cavity, including lining of the nostril (vestibule) and the olfactory mucosa. Nasal mucosa consists of ciliated cells, goblet cells, brush cells, small granule cells, basal cells (stem cells) and glands containing both mucous and serous cells. Nose Anatomy (External & Internal). The condition is classified into allergic, nonallergic, and infectious rhinitis. Allergic rhinitis is due to a type I hypersensitivity reaction Type I hypersensitivity reaction Type I hypersensitivity reaction is an abnormal immune response triggered by exposure to specific antigens known as allergens. In this type of hypersensitivity reaction, the presentation of the antigen to the T-helper cells (Th cells) initiates a cascade of immunologic events leading to the production of antigen-specific IgE antibodies. Type I Hypersensitivity Reaction. Non-allergic rhinitis is due to increased blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the nasal mucosa Nasal mucosa The mucous lining of the nasal cavity, including lining of the nostril (vestibule) and the olfactory mucosa. Nasal mucosa consists of ciliated cells, goblet cells, brush cells, small granule cells, basal cells (stem cells) and glands containing both mucous and serous cells. Nose Anatomy (External & Internal). Infectious rhinitis is caused by an upper respiratory tract infection. All 3 types present with nasal congestion, rhinorrhea Rhinorrhea Excess nasal drainage. Respiratory Syncytial Virus, and sneezing Sneezing The sudden, forceful, involuntary expulsion of air from the nose and mouth caused by irritation to the mucous membranes of the upper respiratory tract. Rhinovirus. Diagnosis is mainly clinical. Management includes antihistamines Antihistamines Antihistamines are drugs that target histamine receptors, particularly H1 and H2 receptors. H1 antagonists are competitive and reversible inhibitors of H1 receptors. First-generation antihistamines cross the blood-brain barrier and can cause sedation. Antihistamines, decongestants, and immunotherapy.
Last updated: Mar 20, 2024
| Infectious | Allergic | Non-allergic |
|---|---|---|
| Usually caused by a viral or bacterial infection | Type I hypersensitivity reaction Type I hypersensitivity reaction Type I hypersensitivity reaction is an abnormal immune response triggered by exposure to specific antigens known as allergens. In this type of hypersensitivity reaction, the presentation of the antigen to the T-helper cells (Th cells) initiates a cascade of immunologic events leading to the production of antigen-specific IgE antibodies. Type I Hypersensitivity Reaction | An increase in blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the nasal mucosa Nasal mucosa The mucous lining of the nasal cavity, including lining of the nostril (vestibule) and the olfactory mucosa. Nasal mucosa consists of ciliated cells, goblet cells, brush cells, small granule cells, basal cells (stem cells) and glands containing both mucous and serous cells. Nose Anatomy (External & Internal) due to irritants, but not allergens |
Acute:
|
|
|
Type I hypersensitivity reaction Type I hypersensitivity reaction Type I hypersensitivity reaction is an abnormal immune response triggered by exposure to specific antigens known as allergens. In this type of hypersensitivity reaction, the presentation of the antigen to the T-helper cells (Th cells) initiates a cascade of immunologic events leading to the production of antigen-specific IgE antibodies. Type I Hypersensitivity Reaction triggers inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation in the nose Nose The nose is the human body’s primary organ of smell and functions as part of the upper respiratory system. The nose may be best known for inhaling oxygen and exhaling carbon dioxide, but it also contributes to other important functions, such as tasting. The anatomy of the nose can be divided into the external nose and the nasal cavity. Nose Anatomy (External & Internal), which is immunoglobulin E ( IgE IgE An immunoglobulin associated with mast cells. Overexpression has been associated with allergic hypersensitivity. Immunoglobulins: Types and Functions)-mediated.
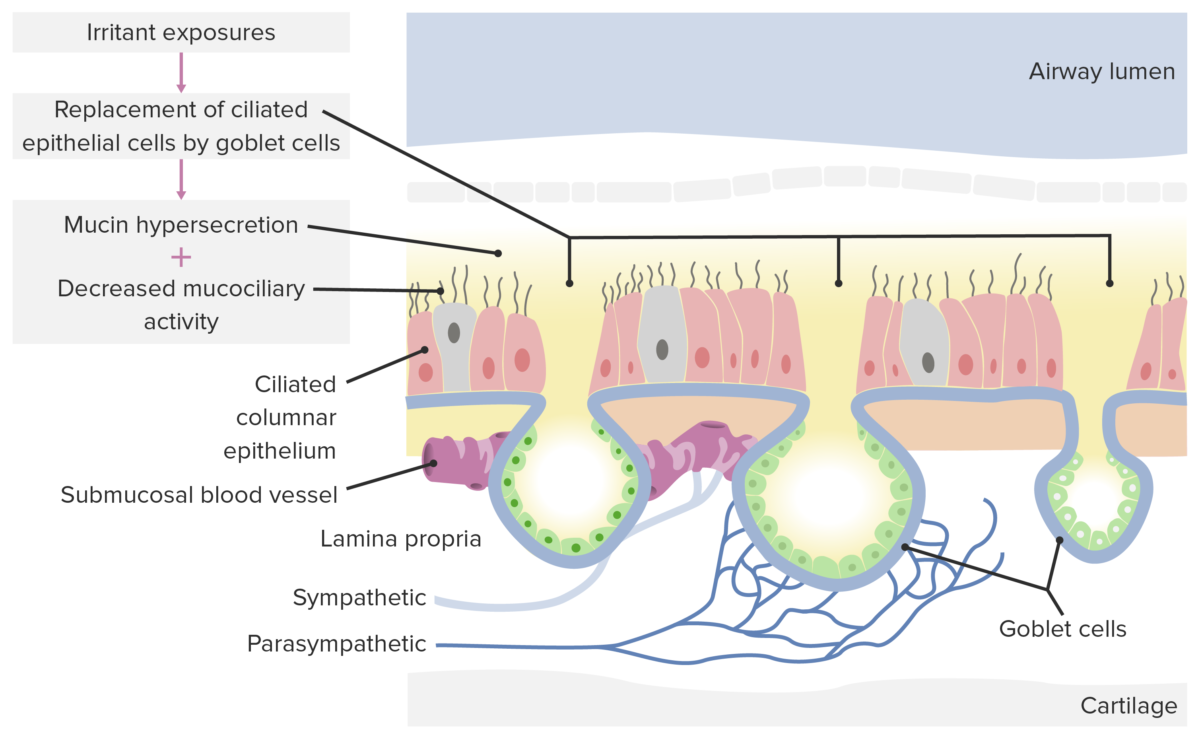
Pathological changes in non-allergic rhinitis: When the nasal mucosa is exposed to irritants, goblet cells overcrowd normal epithelia, causing mucin hypersecretion and decreased mucociliary activity, leading to congestion and other symptoms of rhinitis.
Image by Lecturio.General symptoms of rhinitis include:
Specific symptoms for the individual categories of rhinitis include the following:
Diagnosis is clinical, based on characteristic symptoms, suggestive clinical history, and supportive physical exam findings.