The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology. The skin is composed of surface epithelium Surface epithelium Epithelium is classified according to the cells (squamous, cuboidal, columnar), the number of layers, and other unique characteristics either due to function (transitional epithelium allowing distention) or appearance (pseudostratified epithelium giving a false impression of multiple layers). Surface epithelium has multiple functions, which include protection, secretion, filtration, and sensory reception. Surface Epithelium: Histology, exocrine components, connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology, muscles, and nerves. The primary role of the skin is to serve as a protective barrier between the internal body and the external environment; it also protects the body from excessive fluid loss.
Last updated: Apr 18, 2023
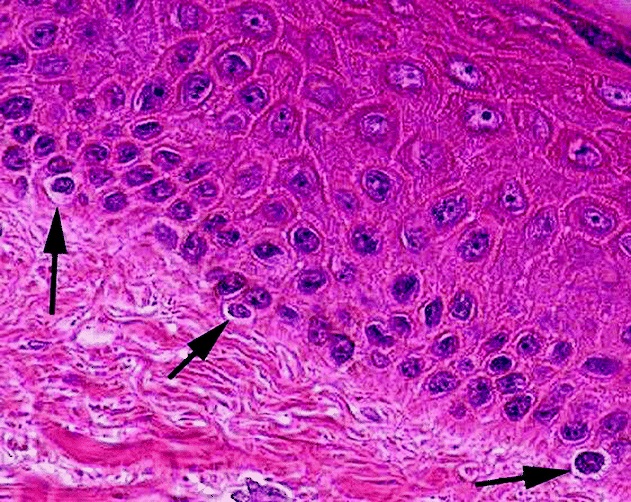
Micrograph of melanocytes in the epidermis
Image: “Micrograph of melanocytes in the epidermis” by Setijanti, H.B., et al. License: CC BY 4.0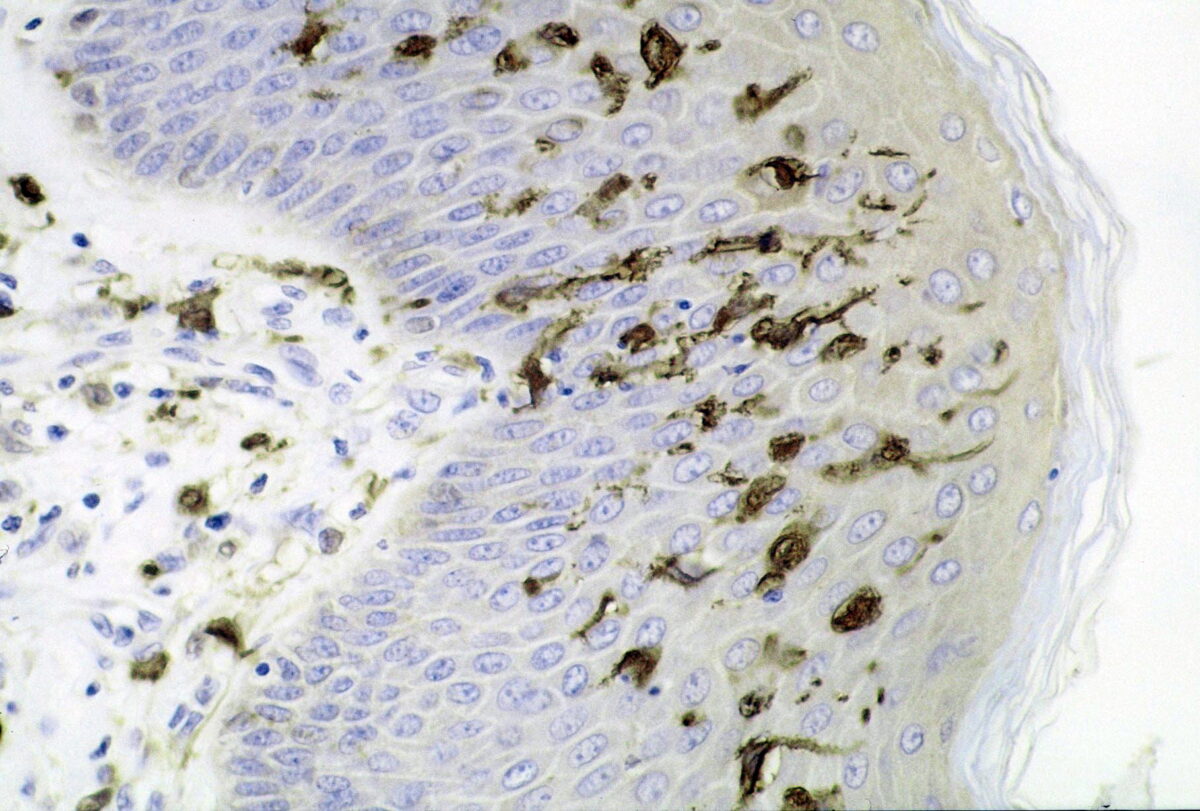
Section of skin showing large numbers of dendritic (Langerhans) cells in the epidermis:
Mycobacterium ulcerans infection, S100 immunoperoxidase stain
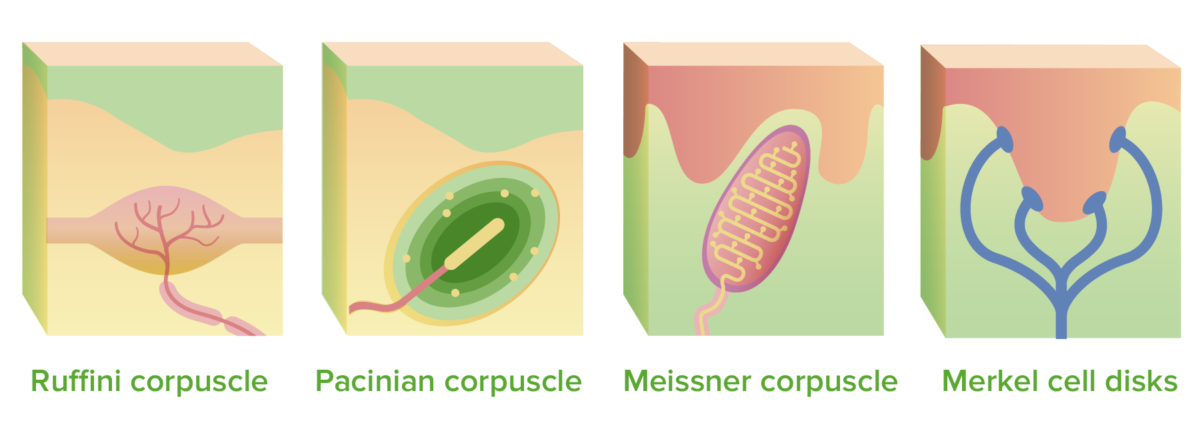
Mechanoreceptors:
The Ruffini and Pacinian corpuscles are located in the deep dermis, the Meissner corpuscles extend into the dermal papillae, and the Merkel cell disks connect to the epidermis.
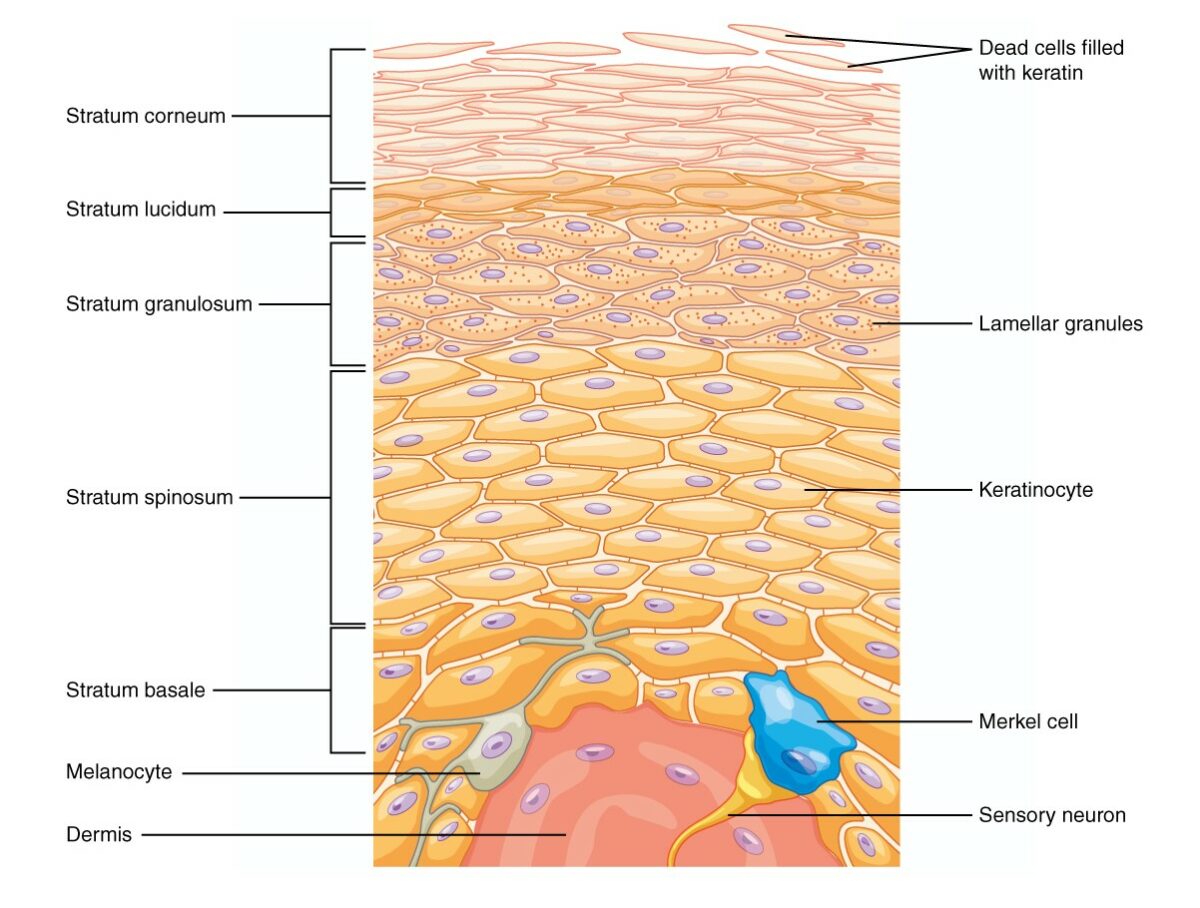
There are 5 layers of epidermis:
Beginning from the cells located in the stratum basale, they differentiate and proliferate toward the skin surface and integrate themselves into the other layers, the last layer being the stratum corneum, which is composed of dead keratinized cells.

The dermis is made up of 2 layers:
The papillary layer is made up of collagen and elastin fibers and contains phagocytes, fibroblasts, and adipocytes. The reticular layer gives the skin its elasticity and helps to toughen the skin. Sweat glands and hair follicles are found at this layer. This layer is also well vascularized.
Each layer of the skin has a unique function.
Epidermis and dermis:
Hypodermis:

Structure of the follicular unit:
The hair bulb is located in the deep dermis/hypodermis, and the hair shaft extends through the dermis before exiting the epidermis. The arrector pili muscle is located in the dermis and is responsible for piloerection.
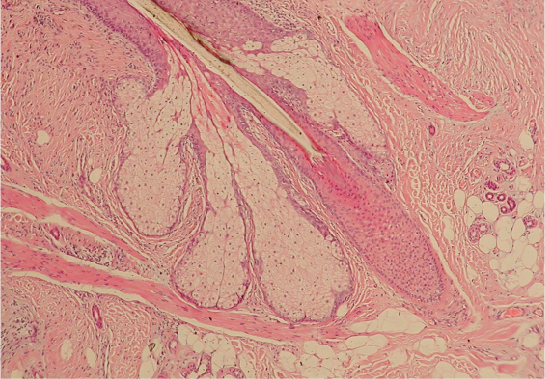
Cross section of a hair follicle:
The hair is composed of keratinized cells that emerge and migrate upward inside the hair follicle. When the hair shaft emerges from the skin surface, it does so at a slightly slanted angle. For every hair follicle, there is an adjacent sebaceous gland.
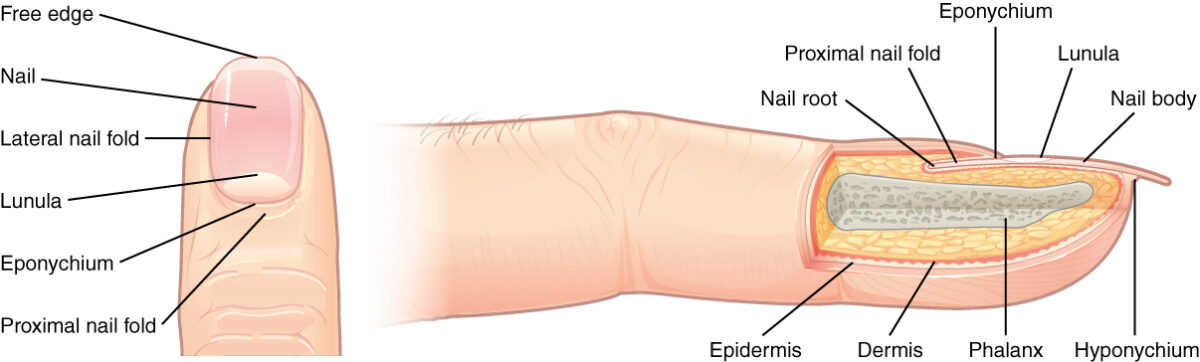
Structure of the nail:
The whitish crescent-shaped end of the nail (toward the body) is referred to as the lunula (“small moon”). Between the lunula and skin, there is a protective layer, called the cuticle, that keeps pathogens from entering beneath the skin. Behind the cuticle (toward the body), is the nail root, which forms keratinized cells that push the nail forward.
Fingernails grow faster than toenails. The typical growth rate of a fingernail is 1 mm per week; a toenail grows 0.5 mm per week.