The hepatitis E virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology (HEV) is a small nonenveloped virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology that contains linear, single-stranded, positive-sense RNA RNA A polynucleotide consisting essentially of chains with a repeating backbone of phosphate and ribose units to which nitrogenous bases are attached. RNA is unique among biological macromolecules in that it can encode genetic information, serve as an abundant structural component of cells, and also possesses catalytic activity. RNA Types and Structure, making it similar to norovirus Norovirus Norovirus is a nonenveloped, single-stranded, positive-sense RNA virus belonging to the Caliciviridae family. Norovirus infections are transmitted via the fecal-oral route or by aerosols from vomiting. The virus is one of the most common causes of nonbacterial gastroenteritis epidemic worldwide. Symptoms include watery and nonbloody diarrhea, nausea, vomiting, and low-grade fever. Norovirus. Transmission of HEV is via the fecal–oral route and is clinically similar to that of hepatitis A Hepatitis A Hepatitis A is caused by the hepatitis A virus (HAV), a nonenveloped virus of the Picornaviridae family with single-stranded RNA. HAV causes an acute, highly contagious hepatitis with unspecific prodromal symptoms such as fever and malaise followed by jaundice and elevated liver transaminases. Hepatitis A Virus. However, unlike hepatitis A Hepatitis A Hepatitis A is caused by the hepatitis A virus (HAV), a nonenveloped virus of the Picornaviridae family with single-stranded RNA. HAV causes an acute, highly contagious hepatitis with unspecific prodromal symptoms such as fever and malaise followed by jaundice and elevated liver transaminases. Hepatitis A Virus, hepatitis E is quite severe, especially in pregnant women, and may cause fulminant hepatitis Fulminant hepatitis Echovirus along with hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome over a period of approximately 8 weeks. Management is mainly preventive and includes avoiding contaminated drinking water, good sanitation, and adequate personal hygiene.
Last updated: May 16, 2024
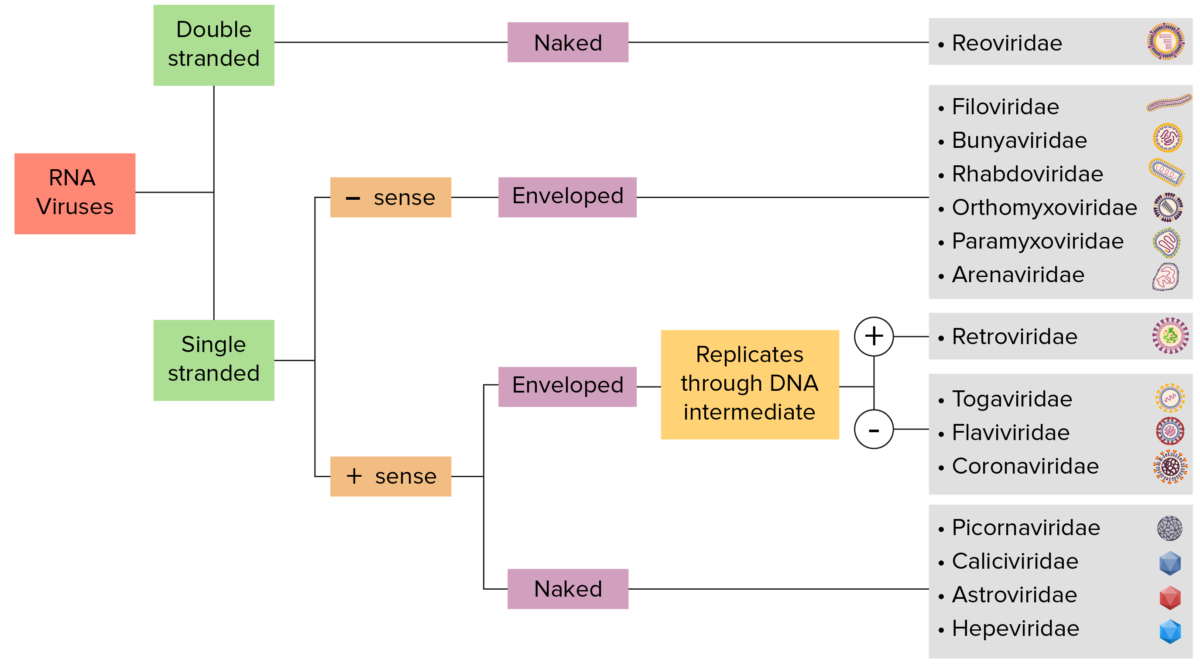
RNA virus identification:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. RNA genome viruses can be further characterized by either a single- or double-stranded RNA. “Enveloped” viruses are covered by a thin coat of cell membrane (usually taken from the host cell). If the coat is absent, the viruses are called “naked” viruses. Viruses with single-stranded genomes are “positive-sense” viruses if the genome is directly employed as messenger RNA (mRNA), which is translated into proteins. “Negative-sense,” single-stranded viruses employ RNA dependent RNA polymerase, a viral enzyme, to transcribe their genome into messenger RNA.
Primary replication:
Table: Comparison of hepatitis viruses Viruses Minute infectious agents whose genomes are composed of DNA or RNA, but not both. They are characterized by a lack of independent metabolism and the inability to replicate outside living host cells. Virology A–E
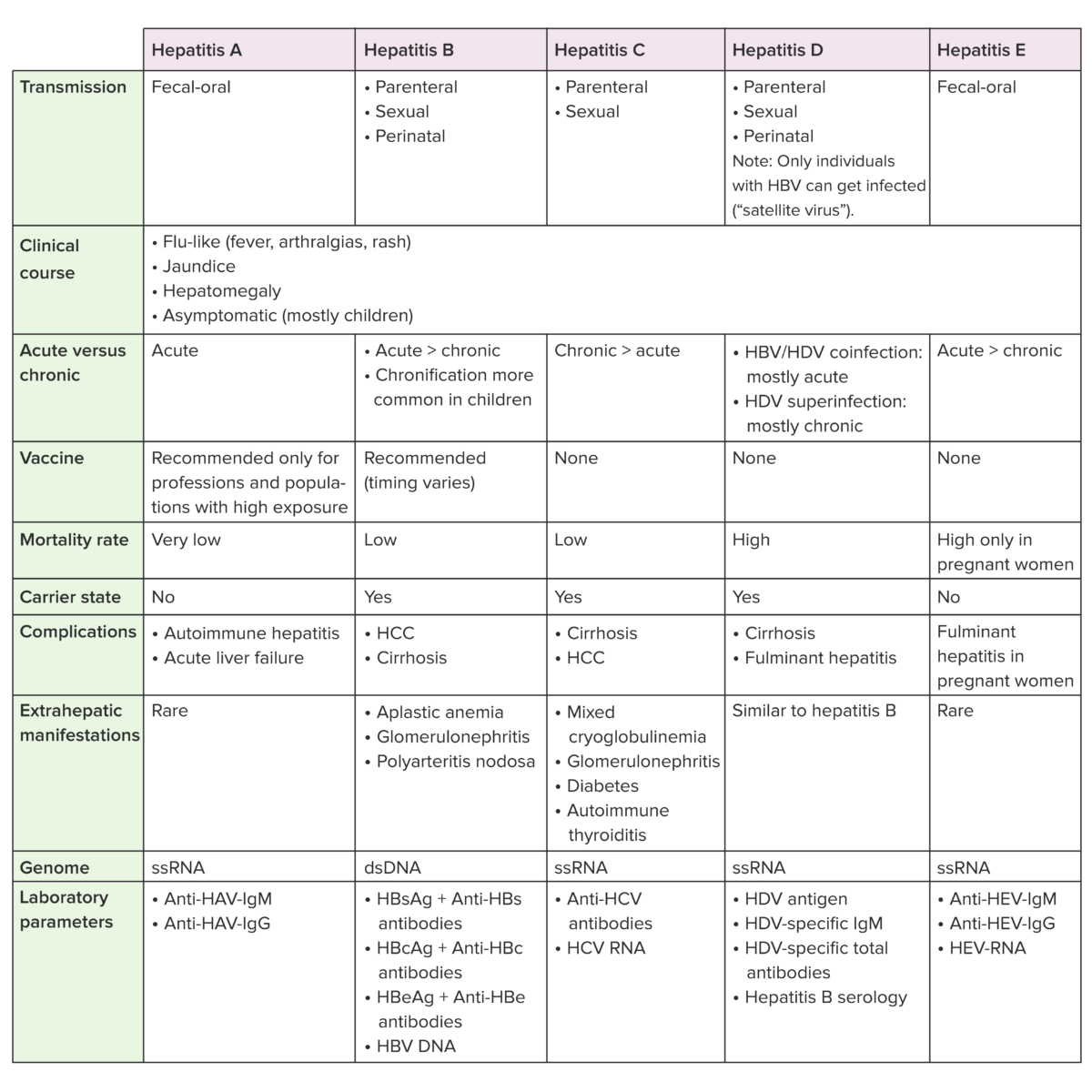
Anti-HBc: hepatitis B core antibody
Anti-HBs: hepatitis B surface antibody
HBcAg: hepatitis B core antigen
HBsAg: hepatitis B surface antigen
HBV: hepatitis B virus
HCC: hepatocellular carcinoma
HAV: hepatitis A virus
HCV: hepatitis C virus
HDV: hepatitis D virus