Hepatitis B virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology (HBV) is a partially double-stranded DNA DNA A deoxyribonucleotide polymer that is the primary genetic material of all cells. Eukaryotic and prokaryotic organisms normally contain DNA in a double-stranded state, yet several important biological processes transiently involve single-stranded regions. DNA, which consists of a polysugar-phosphate backbone possessing projections of purines (adenine and guanine) and pyrimidines (thymine and cytosine), forms a double helix that is held together by hydrogen bonds between these purines and pyrimidines (adenine to thymine and guanine to cytosine). DNA Types and Structure virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology, which belongs to the Orthohepadnavirus genus and the Hepadnaviridae family. Hepatitis B virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology is transmitted by exposure to infectious blood or body fluids. Examples of types of exposure include sexual intercourse, IV drug use, and childbirth. The virus Virus Viruses are infectious, obligate intracellular parasites composed of a nucleic acid core surrounded by a protein capsid. Viruses can be either naked (non-enveloped) or enveloped. The classification of viruses is complex and based on many factors, including type and structure of the nucleoid and capsid, the presence of an envelope, the replication cycle, and the host range. Virology can cause potentially life-threatening liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease. Most individuals with acute HBV infection are asymptomatic or have mild, self-limiting Self-Limiting Meningitis in Children symptoms. Chronic infection can be asymptomatic or create hepatic inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation, leading to liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis and hepatocellular carcinoma Hepatocellular carcinoma Hepatocellular carcinoma (HCC) typically arises in a chronically diseased or cirrhotic liver and is the most common primary liver cancer. Diagnosis may include ultrasound, CT, MRI, biopsy (if inconclusive imaging), and/or biomarkers. Hepatocellular Carcinoma (HCC) and Liver Metastases ( HCC HCC Hepatocellular carcinoma (HCC) typically arises in a chronically diseased or cirrhotic liver and is the most common primary liver cancer. Diagnosis may include ultrasound, CT, MRI, biopsy (if inconclusive imaging), and/or biomarkers. Hepatocellular Carcinoma (HCC) and Liver Metastases). Management of acute hepatitis Acute Hepatitis Autoimmune Hepatitis is typically supportive. Administration of antivirals or liver transplantation Liver transplantation The transference of a part of or an entire liver from one human or animal to another. Hepatocellular Carcinoma (HCC) and Liver Metastases may be necessary in fulminant and chronic cases.
Last updated: May 16, 2024
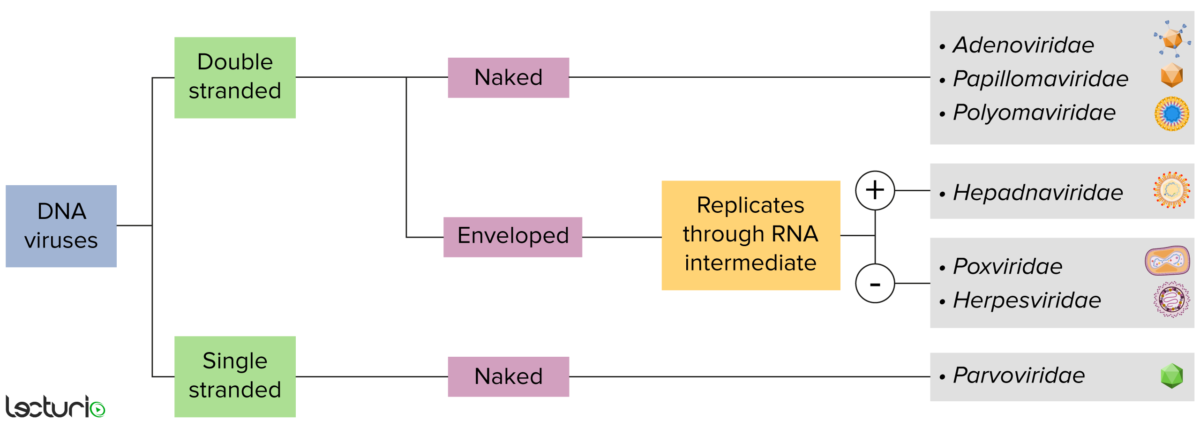
Identification of DNA viruses:
Viruses can be classified in many ways. Most viruses, however, will have a genome formed by either DNA or RNA. Viruses with a DNA genome can be further characterized as single or double stranded. “Enveloped” viruses are covered by a thin coat of cell membrane, which is usually taken from the host cell. If the coat is absent, however, the viruses are called “naked” viruses. Some enveloped viruses translate DNA into RNA before incorporating into the genome of the host cell.
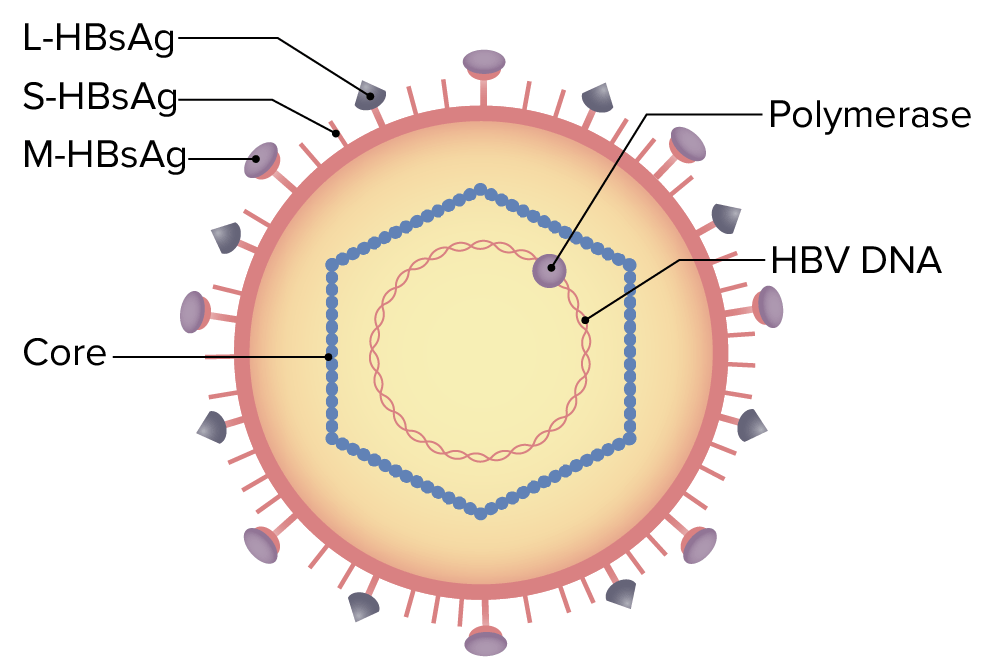
Structure of hepatitis B virus (HBV):
The virus particle (virion) is made up of an outer lipid envelope. The nucleocapsid (core) encloses the viral DNA and a DNA polymerase that has reverse transcriptase activity. The outer envelope contains proteins that help the virus bind to and enter target cells.
Electron micrograph of the hepatitis B virus (HBV)
Image: “Hepatitis-B virions” by CDC. License: Public Domain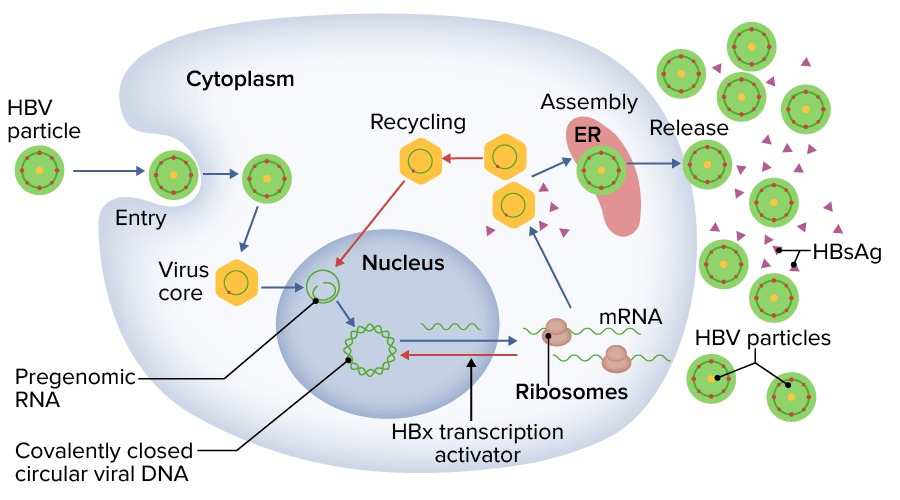
Hepatitis B virus (HBV) replication:
The HBV is phagocytosed to replicate by utilizing machinery of host cell replication.
HBsAg: hepatitis B surface antigen
Screening Screening Preoperative Care for HBV infection:
Acute hepatitis Acute Hepatitis Autoimmune Hepatitis B:
Past HBV infection (inactive):
HBV-vaccinated individuals:
Chronic hepatitis B Chronic Hepatitis B Inflammation of the liver in humans caused by hepatitis C virus, a single-stranded RNA virus. Its incubation period is 30-90 days. Hepatitis c is transmitted primarily by contaminated blood parenterally, and is often associated with transfusion and intravenous drug abuse. However, in a significant number of cases, the source of hepatitis C infection is unknown. Antivirals for Hepatitis B:
| HBsAg | Anti-HBc-IgM | Anti-HBc-IgG | Anti-HBs | |
|---|---|---|---|---|
| Susceptible | Negative | Negative | Negative | Negative |
| Acute infection | Positive | Positive | Negative | Negative |
| Previous infection (inactive) | Negative | Negative | Positive | Positive |
| HBV vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination | Negative | Negative | Negative | Positive |
| Chronic infection | Positive | Negative | Positive | Negative |
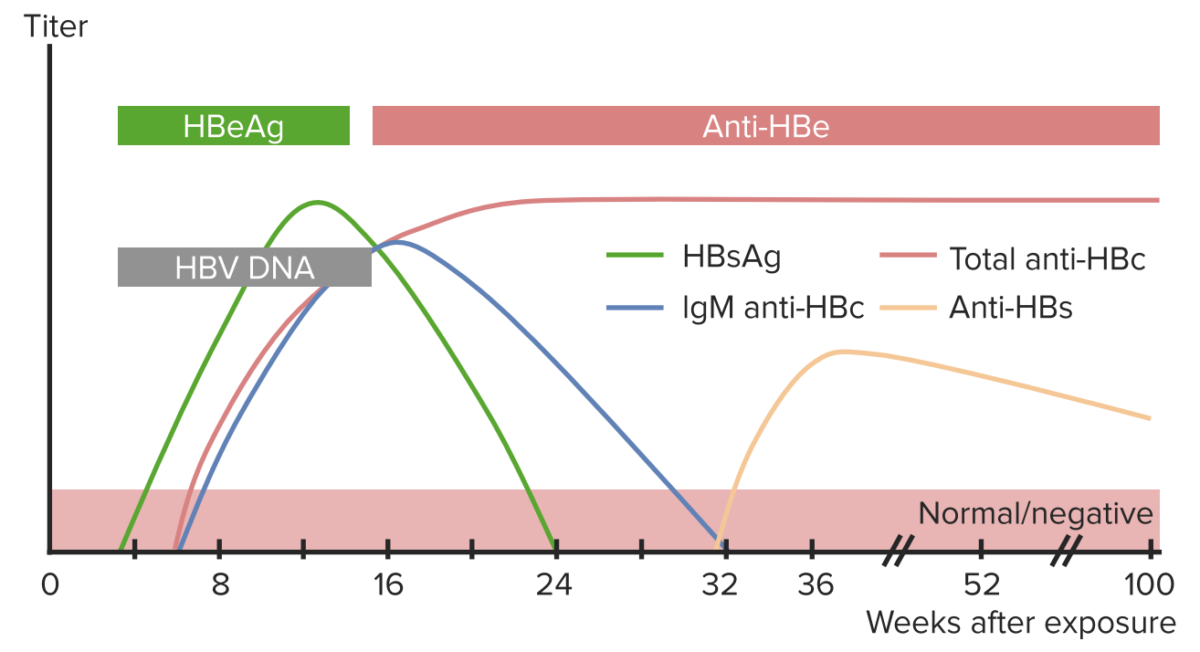
Laboratory parameters of hepatitis B virus (HBV) infection:
The chart shows the typical course of important markers in diagnosis of HBV infection after viral exposure.
Acute hepatitis Acute Hepatitis Autoimmune Hepatitis B:
Chronic hepatitis B Chronic Hepatitis B Inflammation of the liver in humans caused by hepatitis C virus, a single-stranded RNA virus. Its incubation period is 30-90 days. Hepatitis c is transmitted primarily by contaminated blood parenterally, and is often associated with transfusion and intravenous drug abuse. However, in a significant number of cases, the source of hepatitis C infection is unknown. Antivirals for Hepatitis B:
Screening Screening Preoperative Care:
Screening Screening Preoperative Care for HBV infection is recommended by the CDC for the following groups:
Vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination:
Postexposure prophylaxis Prophylaxis Cephalosporins ( PEP PEP A monocarboxylic acid anion derived from selective deprotonation of the carboxy group of phosphoenolpyruvic acid. It is a metabolic intermediate in glycolysis; gluconeogenesis; and other pathways. Glycolysis):
Anti-HBc: hepatitis B core antibody
Anti-HBs: hepatitis B surface antibody
HBcAg: hepatitis B core antigen
HBsAg: hepatitis B surface antigen
HBV: hepatitis B virus
HCC: hepatocellular carcinoma
HAV: hepatitis A virus
HCV: hepatitis C virus
HDV: hepatitis D virus