Bronchiolitis Bronchiolitis Inflammation of the bronchioles. Pediatric Chest Abnormalities obliterans is an obstructive lung disease triggered by a bronchiolar injury, which leads to inflammatory fibrosis and narrowing of the distal bronchioles Bronchioles The small airways branching off the tertiary bronchi. Terminal bronchioles lead into several orders of respiratory bronchioles which in turn lead into alveolar ducts and then into pulmonary alveoli. Bronchial Tree: Anatomy. The triggering bronchiolar injury is often due to inhalation of a noxious substance, infection, or drug toxicity Toxicity Dosage Calculation. Bronchiolitis Bronchiolitis Inflammation of the bronchioles. Pediatric Chest Abnormalities obliterans is also associated with rheumatic disease and is an important complication to recognize following a lung or hematopoietic stem-cell transplant. Following bronchiolar injury, there is an abnormal fibroproliferation within the bronchioles Bronchioles The small airways branching off the tertiary bronchi. Terminal bronchioles lead into several orders of respiratory bronchioles which in turn lead into alveolar ducts and then into pulmonary alveoli. Bronchial Tree: Anatomy, which results in small-airway obstruction. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with a persistent progressive cough and dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea. Diagnosis is usually made based on pulmonary function tests (showing a non-reversible obstructive pattern, air trapping, and decreased gas exchange Gas exchange Human cells are primarily reliant on aerobic metabolism. The respiratory system is involved in pulmonary ventilation and external respiration, while the circulatory system is responsible for transport and internal respiration. Pulmonary ventilation (breathing) represents movement of air into and out of the lungs. External respiration, or gas exchange, is represented by the O2 and CO2 exchange between the lungs and the blood. Gas Exchange) and high-resolution CT High-resolution CT Imaging of the Lungs and Pleura (showing air trapping and bronchial-wall thickening). Management involves supportive care, bronchodilators Bronchodilators Asthma Drugs, glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids, and/or macrolide antibiotics. Immunosuppressive therapy is usually increased in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who have undergone transplantation, and retransplantation may be required if the condition worsens.
Last updated: Apr 27, 2025
Small airway Airway ABCDE Assessment injuries that trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation bronchiolitis Bronchiolitis Inflammation of the bronchioles. Pediatric Chest Abnormalities obliterans can result from inhalation, infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, drug exposure, lung inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation due to a rheumatic process, or chronic transplant rejection.
Injury to the distal bronchioles Bronchioles The small airways branching off the tertiary bronchi. Terminal bronchioles lead into several orders of respiratory bronchioles which in turn lead into alveolar ducts and then into pulmonary alveoli. Bronchial Tree: Anatomy results in inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation. A dysregulated immune response then leads to fibroproliferation and narrowing of these small airways and decreases airflow.
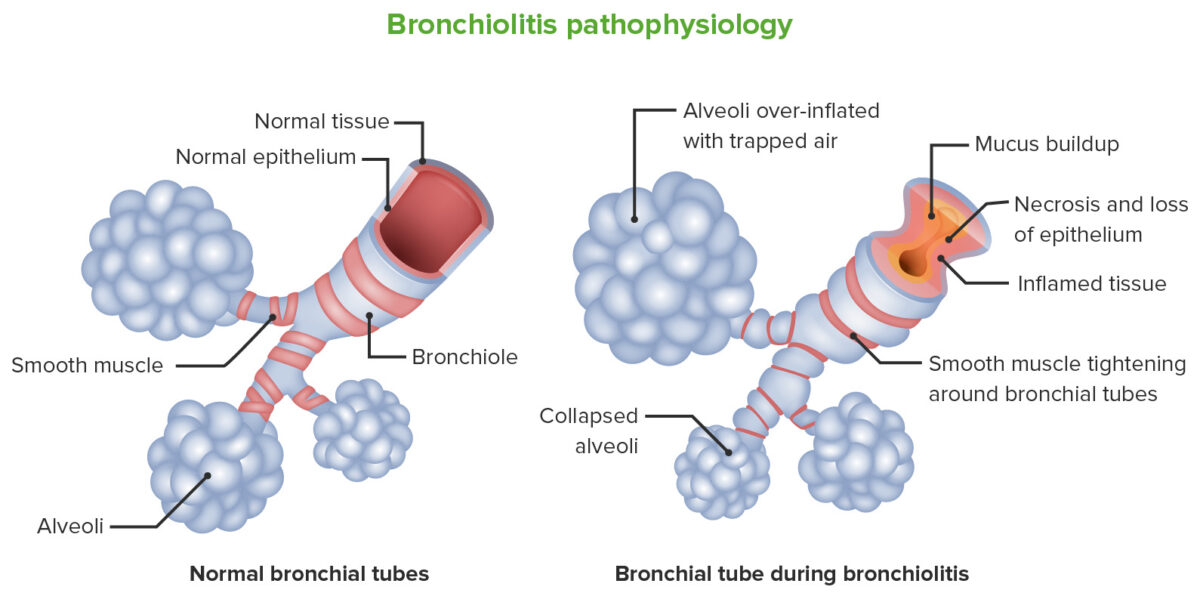
Bronchiolitis pathophysiology:
The image on the left represents the structure of a normal bronchiole. The image on the right represents changes occurring in bronchiolitis obliterans. Injury to the distal bronchioles results in inflammation of the bronchioles and adjacent alveoli. Fibrosis occurs (which is abnormal) instead of normal repair. There is mucus buildup, tightening and hypertrophy of the bronchial smooth muscles followed by narrowing of the small airways.
Bronchiolitis Bronchiolitis Inflammation of the bronchioles. Pediatric Chest Abnormalities obliterans should be suspected in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with slowly progressive dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea and cough, especially when the presentation is otherwise atypical for asthma Asthma Asthma is a chronic inflammatory respiratory condition characterized by bronchial hyperresponsiveness and airflow obstruction. The disease is believed to result from the complex interaction of host and environmental factors that increase disease predisposition, with inflammation causing symptoms and structural changes. Patients typically present with wheezing, cough, and dyspnea. Asthma or chronic obstructive pulmonary disease Pulmonary disease Diseases involving the respiratory system. Blastomyces/Blastomycosis ( COPD COPD Chronic obstructive pulmonary disease (COPD) is a lung disease characterized by progressive, largely irreversible airflow obstruction. The condition usually presents in middle-aged or elderly persons with a history of cigarette smoking. Signs and symptoms include prolonged expiration, wheezing, diminished breath sounds, progressive dyspnea, and chronic cough. Chronic Obstructive Pulmonary Disease (COPD)).
The diagnosis of bronchiolitis Bronchiolitis Inflammation of the bronchioles. Pediatric Chest Abnormalities obliterans is usually made based on history, pulmonary function test Pulmonary function test Pulmonary function tests are a group of diagnostic procedures yielding useful, quantifiable information about the rate of the flow of air through the individual’s airways, lung capacity, and the efficiency of gas exchange in relation to time. The most commonly utilized tests include spirometry (before and after bronchodilator use), lung volumes, and quantitation of diffusing capacity for carbon monoxide (CO). The tests can be influenced by the individual’s effort/fatigue, disease state, or anatomical malformation. Pulmonary Function Tests, imaging, and biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma findings.
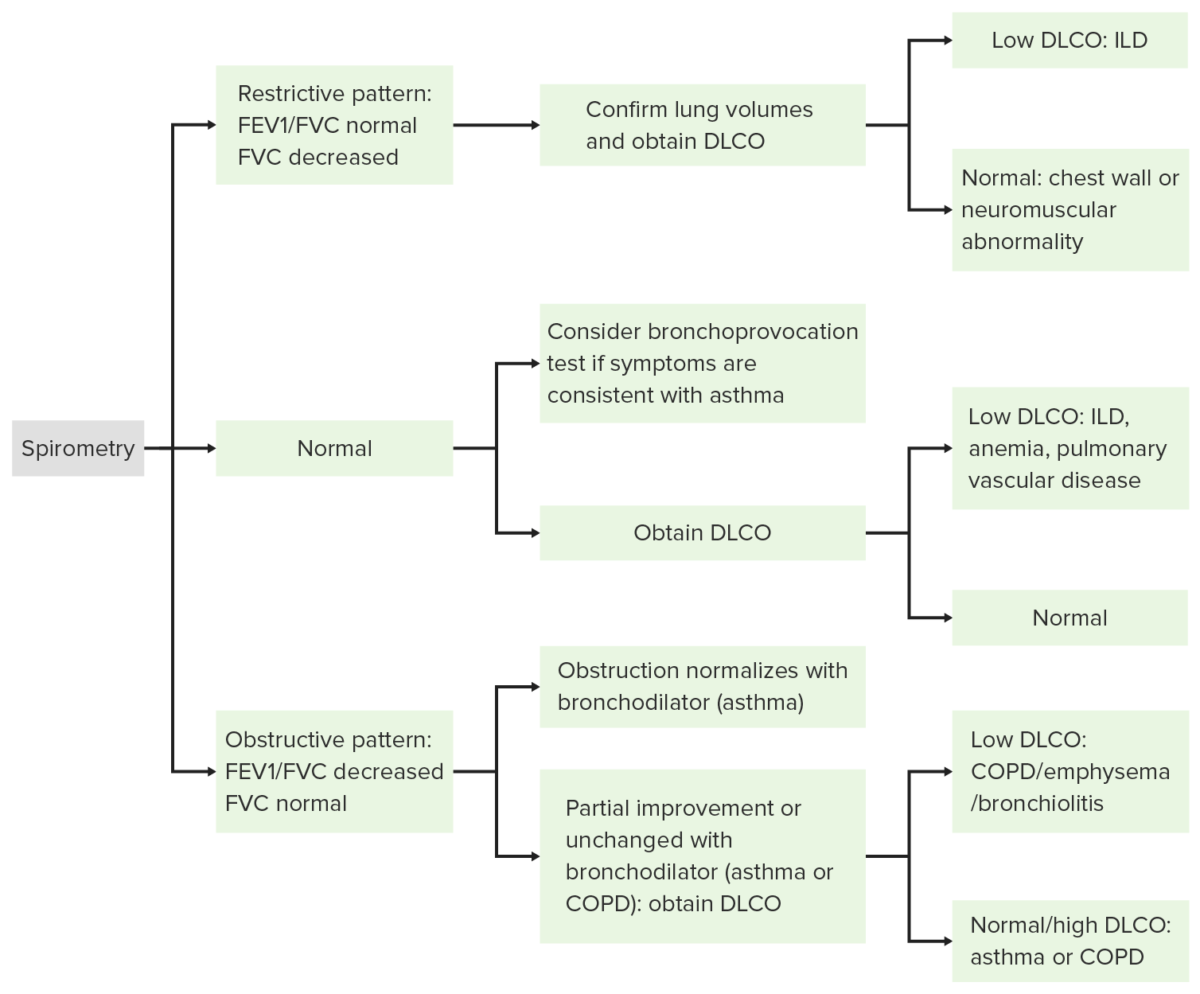
Algorithm for interpretation of pulmonary function tests:
FEV1: forced expiratory volume in the 1st second
FVC: forced vital capacity (total forced exhaled volume)
DLCO: diffusing capacity of the lungs for carbon monoxide (reflects the lung’s ability to transfer inhaled gas across the alveolar-capillary membrane)
COPD: chronic obstructive pulmonary disease
ILD: interstitial lung disease
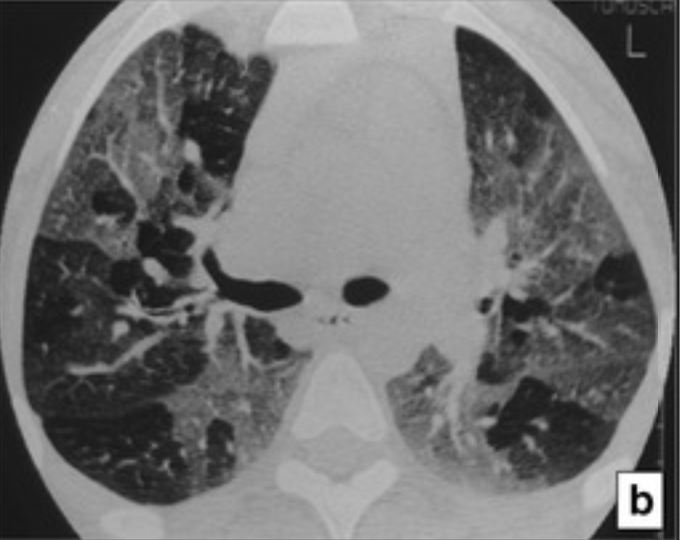
High-resolution CT (HRCT) in bronchiolitis obliterans:
The HRCT at expiration demonstrates a mosaic-attenuation pattern that results from air trapping.
Bronchiolitis Bronchiolitis Inflammation of the bronchioles. Pediatric Chest Abnormalities obliterans is often progressive and refractory to therapy; thus, management is often supportive, symptom driven, and based on the etiology.