The pulmonary examination is a portion of the physical examination involving the assessment of the lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy and airways by a healthcare worker to evaluate for signs of disease or illness. The examination includes inspection Inspection Dermatologic Examination, auscultation, percussion, and palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination. A careful pulmonary exam provides important clues that, along with the history, can guide the physician to a presumptive diagnosis.
Last updated: Jun 4, 2024
Positioning:
Environment:
Initial steps:
The 1st part of the pulmonary exam begins with an inspection Inspection Dermatologic Examination of the patient noting pertinent positive and negative findings.
General appearance/distress level of patient:
Level of consciousness:
Respiratory rate ( RR RR Relative risk (RR) is the risk of a disease or condition occurring in a group or population with a particular exposure relative to a control (unexposed) group. Measures of Risk):
| Age group | Age | Normal respiratory rate range |
|---|---|---|
| Infant | 0–12 months | 30–60/min |
| Toddler | 1–3 years | 24–40/min |
| Preschooler | 4–5 years | 22–34/min |
| School age | 6–12 years | 18–30/min |
| Adolescent and adult | 13 years and older | 12–16/min |
Work of breathing:

Patients with respiratory distress often naturally take the tripod position:
Patients lean forward while sitting and rest the hands on the knees. The position allows maximal expansion of the lungs and airways to counter the feeling of asphyxia felt by the patient.
Inspection Inspection Dermatologic Examination of thorax:
Examine extremities for signs of respiratory illness:

Nail clubbing:
Clubbed nails are abnormal, rounded nail beds often seen in association with conditions causing chronic hypoxemia, such as cystic fibrosis or interstitial lung disease.
Examine neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess:
Certain breathing patterns help to narrow the differential diagnosis and direct patient care.
| Breathing pattern | Signs on exam | Associated diseases |
|---|---|---|
| Tachypnea | Breathing rate > 20/min in adults |
|
| Bradypnea | Breathing rate < 12/min |
|
| Apnea | No breathing |
|
| Prolonged expiratory phase | Expiration Expiration Ventilation: Mechanics of Breathing phase > ⅔ of breath length (normal inspiration Inspiration Ventilation: Mechanics of Breathing ⅓ of breath, expiration Expiration Ventilation: Mechanics of Breathing ⅔ of breath) |
|
| Cheyne-Stokes breathing |
|
|
| Kussmaul breathing | Rapid sighing respiration Respiration The act of breathing with the lungs, consisting of inhalation, or the taking into the lungs of the ambient air, and of exhalation, or the expelling of the modified air which contains more carbon dioxide than the air taken in. Nose Anatomy (External & Internal) | Metabolic acidosis Acidosis A pathologic condition of acid accumulation or depletion of base in the body. The two main types are respiratory acidosis and metabolic acidosis, due to metabolic acid build up. Respiratory Acidosis (e.g., DKA DKA Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS) are serious, acute complications of diabetes mellitus. Diabetic ketoacidosis is characterized by hyperglycemia and ketoacidosis due to an absolute insulin deficiency. Hyperglycemic Crises) |
| Agonal | Irregular breathing pattern | Imminent cardiorespiratory arrest |
Visualization of the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy can help determine the etiology of disease pathology.
| Chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy finding | Clinically important causes |
|---|---|
| Cachexia (extreme thinness or wasting) |
|
| Obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity |
|
| Surgical scars |
|
| Hyperexpanded barrel chest |
|
| Spinal abnormalities |
|
| Sternal abnormalities |
|
| Chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy masses |
|
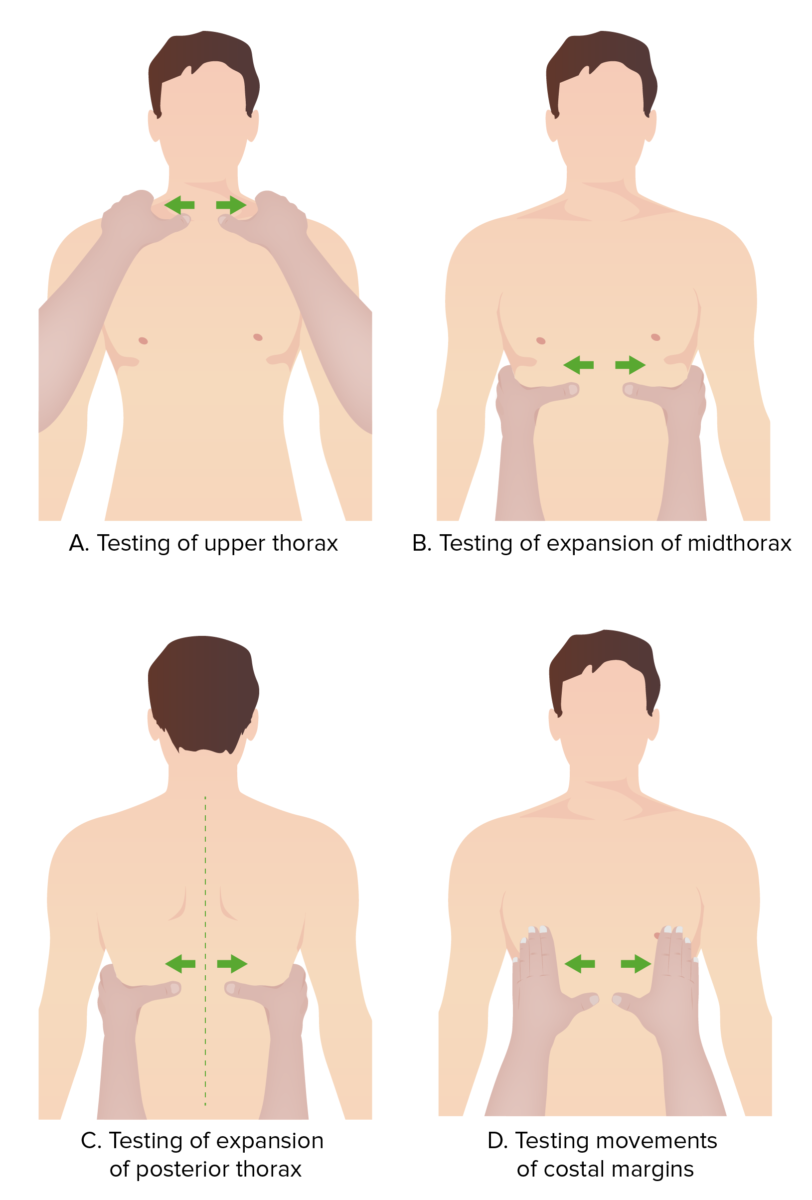
Evaluation of chest movement:
During the pulmonary exam, the physician can utilize their hands as a reference to evaluate different portions of the chest moving symmetrically during the respiratory cycle.

Tactile fremitus:
The clinician places the ulnar surface of their hands on both sides of the back to compare vibration transmission while the individual is speaking.
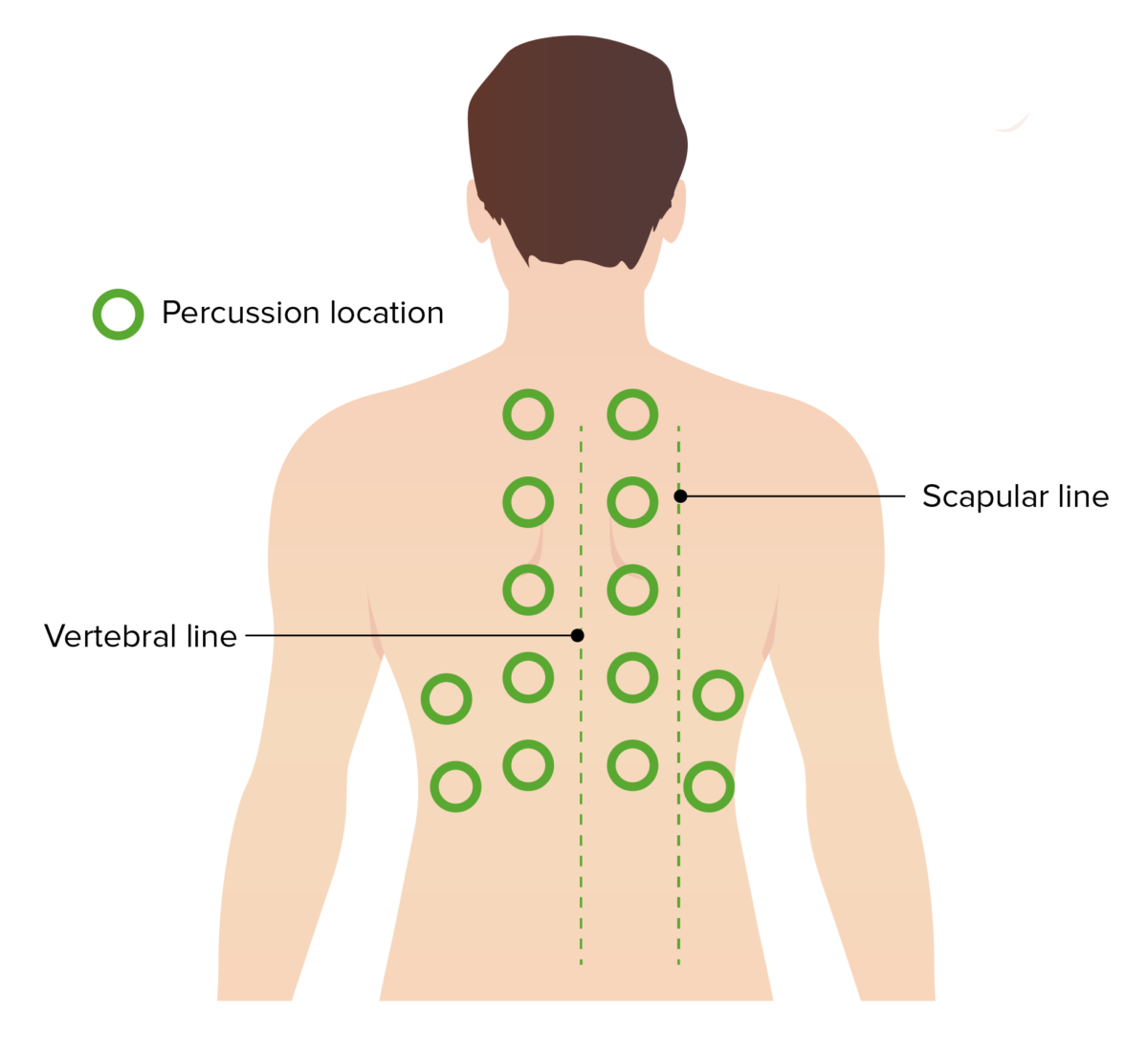
Percussion location:
Percussion is a key component of the lung exam. A systematic and symmetric percussion of a patient’s back can help identify areas of dullness consistent with infection, effusion or atelectasis.

Percussion technique:
The clinician’s middle finger is placed on the area of interest. The other hand strikes the middle finger at the distal interphalangeal joint.
Auscultation is done with stethoscope diaphragm Diaphragm The diaphragm is a large, dome-shaped muscle that separates the thoracic cavity from the abdominal cavity. The diaphragm consists of muscle fibers and a large central tendon, which is divided into right and left parts. As the primary muscle of inspiration, the diaphragm contributes 75% of the total inspiratory muscle force. Diaphragm: Anatomy on unclothed skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions.
| Sound | Description | Normal location |
|---|---|---|
| Tracheal breathing | Loud and high-pitched | Heard over neck Neck The part of a human or animal body connecting the head to the rest of the body. Peritonsillar Abscess |
| Bronchial breathing |
|
Heard over large airways (over sternum Sternum A long, narrow, and flat bone commonly known as breastbone occurring in the midsection of the anterior thoracic segment or chest region, which stabilizes the rib cage and serves as the point of origin for several muscles that move the arms, head, and neck. Chest Wall: Anatomy) |
| Bronchovesicular breathing |
|
Heard over 1st and 2nd intercostal spaces Intercostal spaces Chest Wall: Anatomy |
| Vesicular breathing |
|
Heard over both lung fields |
| Sound | Description | Associated conditions |
|---|---|---|
| Crackles ( rales Rales Respiratory Syncytial Virus or crepitations) |
|
|
| Wheezes or rhonchi Rhonchi Asthma |
|
|
| Inspiratory stridor Stridor Laryngomalacia and Tracheomalacia | High-pitched, musical breath sound from turbulent airflow during inspiration Inspiration Ventilation: Mechanics of Breathing | Obstruction above the
glottis
Glottis
The vocal apparatus of the larynx, situated in the middle section of the larynx. Glottis consists of the vocal folds and an opening (rima glottidis) between the folds.
Larynx: Anatomy:
|
| Expiratory stridor Stridor Laryngomalacia and Tracheomalacia | High-pitched, musical breath sound from turbulent airflow during expiration Expiration Ventilation: Mechanics of Breathing | Obstruction below the
glottis
Glottis
The vocal apparatus of the larynx, situated in the middle section of the larynx. Glottis consists of the vocal folds and an opening (rima glottidis) between the folds.
Larynx: Anatomy:
|
| Biphasic stridor Stridor Laryngomalacia and Tracheomalacia | High-pitched, musical breath sound from turbulent airflow during the entire respiratory cycle | Obstruction at the
glottis
Glottis
The vocal apparatus of the larynx, situated in the middle section of the larynx. Glottis consists of the vocal folds and an opening (rima glottidis) between the folds.
Larynx: Anatomy:
|
| Pleural friction rub |
|
Pleuritis Pleuritis Pleuritis, also known as pleurisy, is an inflammation of the visceral and parietal layers of the pleural membranes of the lungs. The condition can be primary or secondary and results in sudden, sharp, and intense chest pain on inhalation and exhalation. Pleuritis |
| Muffled or absent breath sounds |
|
|
| Disease | Inspection Inspection Dermatologic Examination | Palpation Palpation Application of fingers with light pressure to the surface of the body to determine consistency of parts beneath in physical diagnosis; includes palpation for determining the outlines of organs. Dermatologic Examination | Percussion | Auscultation |
|---|---|---|---|---|
| Status asthmaticus |
|
↓ Tactile fremitus |
|
Expiratory wheezes |
| Pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax |
|
|
Hyperresonant | Faint/no respiratory sound |
| Pleural effusion Pleural Effusion Pleural effusion refers to the accumulation of fluid between the layers of the parietal and visceral pleura. Common causes of this condition include infection, malignancy, autoimmune disorders, or volume overload. Clinical manifestations include chest pain, cough, and dyspnea. Pleural Effusion |
|
|
Dull | Faint respiratory sound |
| Atelectasis Atelectasis Atelectasis is the partial or complete collapse of a part of the lung. Atelectasis is almost always a secondary phenomenon from conditions causing bronchial obstruction, external compression, surfactant deficiency, or scarring. Atelectasis |
|
|
Dull | Faint respiratory sound |
| Consolidation Consolidation Pulmonary Function Tests ( pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia) |
|
↑ Tactile fremitus | Dull |
|
The following are common conditions found utilizing the 4-part pulmonary examination.