Shock is a life-threatening condition associated with impaired circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment that results in tissue hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage. The different types of shock are based on the underlying cause: distributive (↑ cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics (CO), ↓ systemic vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. The most common symptoms include tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, tachypnea Tachypnea Increased respiratory rate. Pulmonary Examination, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, altered mentation, and oliguria Oliguria Decreased urine output that is below the normal range. Oliguria can be defined as urine output of less than or equal to 0. 5 or 1 ml/kg/hr depending on the age. Renal Potassium Regulation. Treatment measures vary depending on the suspected cause of shock and may include mechanical ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing, IV fluids IV fluids Intravenous fluids are one of the most common interventions administered in medicine to approximate physiologic bodily fluids. Intravenous fluids are divided into 2 categories: crystalloid and colloid solutions. Intravenous fluids have a wide variety of indications, including intravascular volume expansion, electrolyte manipulation, and maintenance fluids. Intravenous Fluids for volume resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome, vasopressors Vasopressors Sepsis in Children, and transfusion of blood/blood products.
Last updated: Apr 18, 2023
Shock is a life-threatening condition of organ dysfunction resulting from tissue hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage due to decreased oxygen delivery, increased oxygen consumption, and/or defective oxygen utilization.
| Type of shock | Central venous pressure Central venous pressure The blood pressure in the central large veins of the body. It is distinguished from peripheral venous pressure which occurs in an extremity. Central Venous Catheter ( CVP CVP The blood pressure in the central large veins of the body. It is distinguished from peripheral venous pressure which occurs in an extremity. Central Venous Catheter) | Pulmonary capillary wedge pressure (PCWP) | Cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics | Systemic vascular resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing |
|---|---|---|---|---|
| Distributive | ↓ | ↓ | ↑ | ↓ |
| Cardiogenic | ↑ | ↑ | ↓ | ↑ |
| Obstructive | ↑ | ↓↑ | ↓ | ↑ |
| Hypovolemic | ↓ | ↓ | ↓ | ↑ |
Always maintain a high clinical suspicion for shock. Suggestive features include tachycardia Tachycardia Abnormally rapid heartbeat, usually with a heart rate above 100 beats per minute for adults. Tachycardia accompanied by disturbance in the cardiac depolarization (cardiac arrhythmia) is called tachyarrhythmia. Sepsis in Children, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, altered mentation, oliguria Oliguria Decreased urine output that is below the normal range. Oliguria can be defined as urine output of less than or equal to 0. 5 or 1 ml/kg/hr depending on the age. Renal Potassium Regulation, weak peripheral pulses, and cool and clammy skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions.
Shock is a medical emergency!
Initiate simultaneous treatment and evaluation for etiology, utilizing findings from history, physical examination, hemodynamic monitoring, and laboratory studies. This is best accomplished within a multidisciplinary team in a resource-equipped setting such as the intensive care unit (
ICU
ICU
Hospital units providing continuous surveillance and care to acutely ill patients.
West Nile Virus).
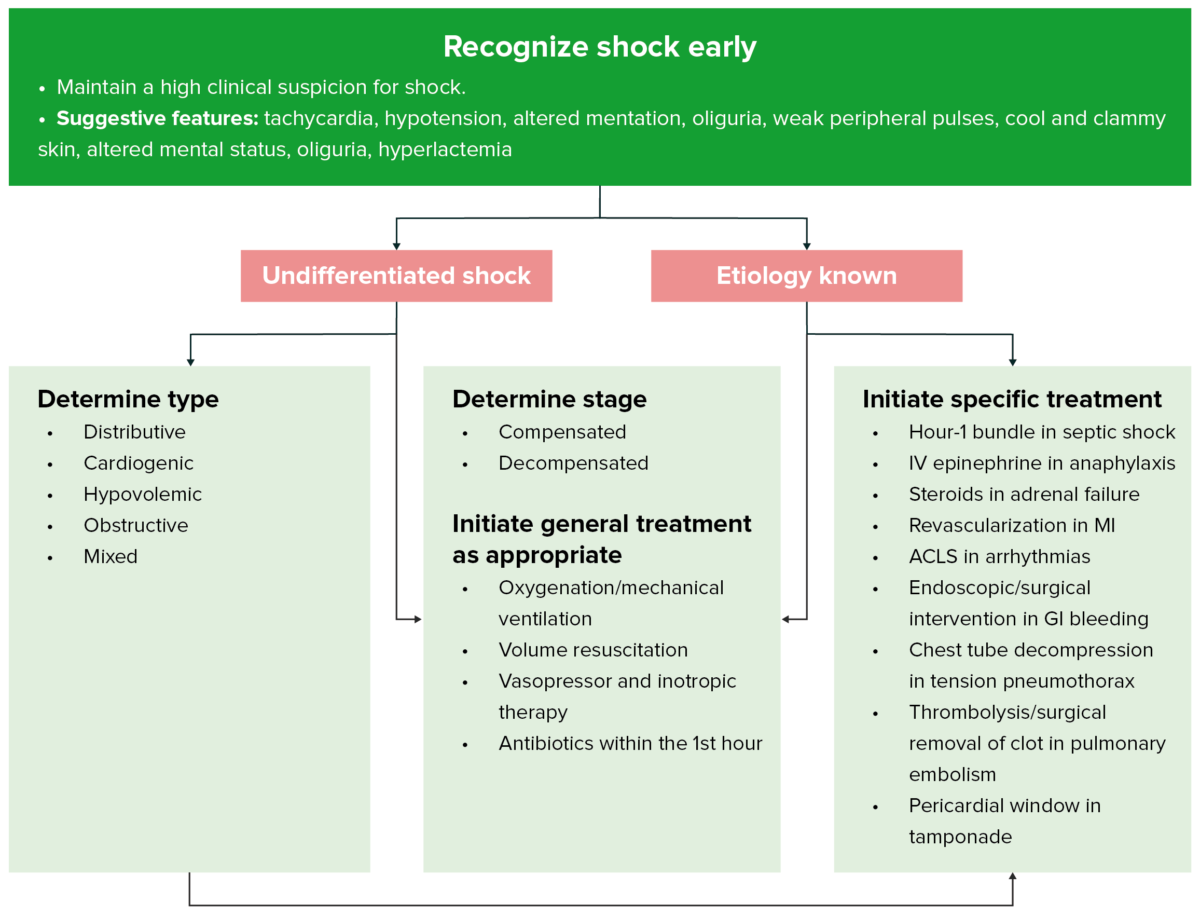
Approach to shock
Image by Lecturio.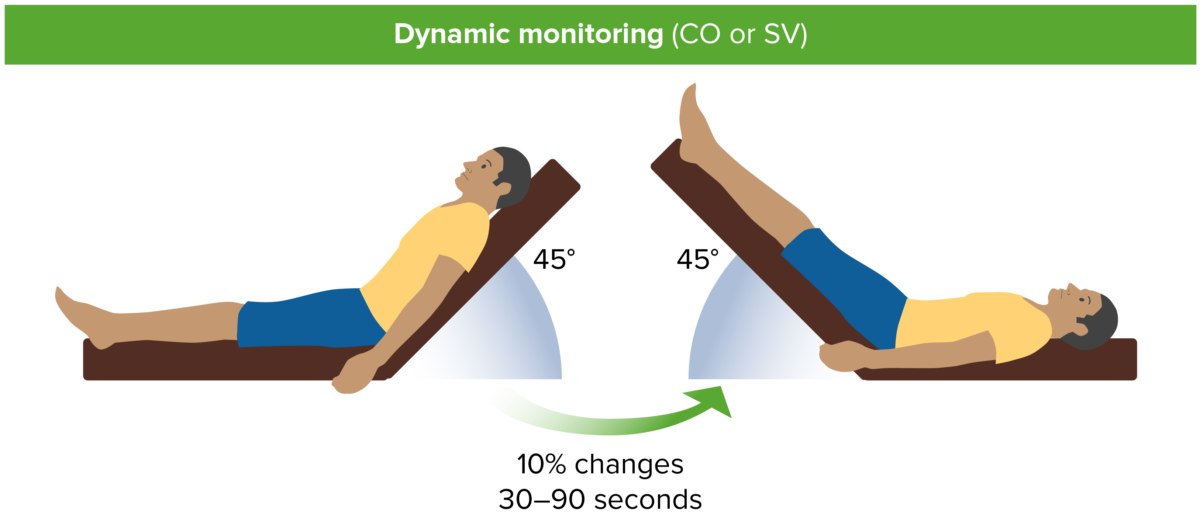
Passive leg raise. CO, cardiac output; SV, stroke volume.
Image by Lecturio.