Type I hypersensitivity reaction is an abnormal immune response triggered by exposure to specific antigens known as allergens. In this type of hypersensitivity reaction, the presentation of the antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination to the T-helper cells (Th cells) initiates a cascade of immunologic events leading to the production of antigen-specific IgE IgE An immunoglobulin associated with mast cells. Overexpression has been associated with allergic hypersensitivity. Immunoglobulins: Types and Functions antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions. Reexposure to the antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination promotes degranulation of the IgE-bound mast cells Mast cells Granulated cells that are found in almost all tissues, most abundantly in the skin and the gastrointestinal tract. Like the basophils, mast cells contain large amounts of histamine and heparin. Unlike basophils, mast cells normally remain in the tissues and do not circulate in the blood. Mast cells, derived from the bone marrow stem cells, are regulated by the stem cell factor. Innate Immunity: Phagocytes and Antigen Presentation and basophils Basophils Granular leukocytes characterized by a relatively pale-staining, lobate nucleus and cytoplasm containing coarse dark-staining granules of variable size and stainable by basic dyes. Innate Immunity: Phagocytes and Antigen Presentation, releasing chemical mediators that cause various allergy symptoms. Manifestations can be local, depending on the route of entry of the antigen Antigen Substances that are recognized by the immune system and induce an immune reaction. Vaccination. In severe cases, systemic reaction leads to anaphylactic shock Shock Shock is a life-threatening condition associated with impaired circulation that results in tissue hypoxia. The different types of shock are based on the underlying cause: distributive (↑ cardiac output (CO), ↓ systemic vascular resistance (SVR)), cardiogenic (↓ CO, ↑ SVR), hypovolemic (↓ CO, ↑ SVR), obstructive (↓ CO), and mixed. Types of Shock. To determine allergic etiology, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions testing as well as in vitro tests are available. Management includes avoidance of triggers to reduce exacerbation. Common treatment options are antihistamines Antihistamines Antihistamines are drugs that target histamine receptors, particularly H1 and H2 receptors. H1 antagonists are competitive and reversible inhibitors of H1 receptors. First-generation antihistamines cross the blood-brain barrier and can cause sedation. Antihistamines and glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids to control the inflammatory response. Anaphylaxis, however, is a medical emergency that requires immediate airway Airway ABCDE Assessment access with administration of epinephrine Epinephrine The active sympathomimetic hormone from the adrenal medulla. It stimulates both the alpha- and beta- adrenergic systems, causes systemic vasoconstriction and gastrointestinal relaxation, stimulates the heart, and dilates bronchi and cerebral vessels. Sympathomimetic Drugs and fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome.
Last updated: Apr 14, 2025
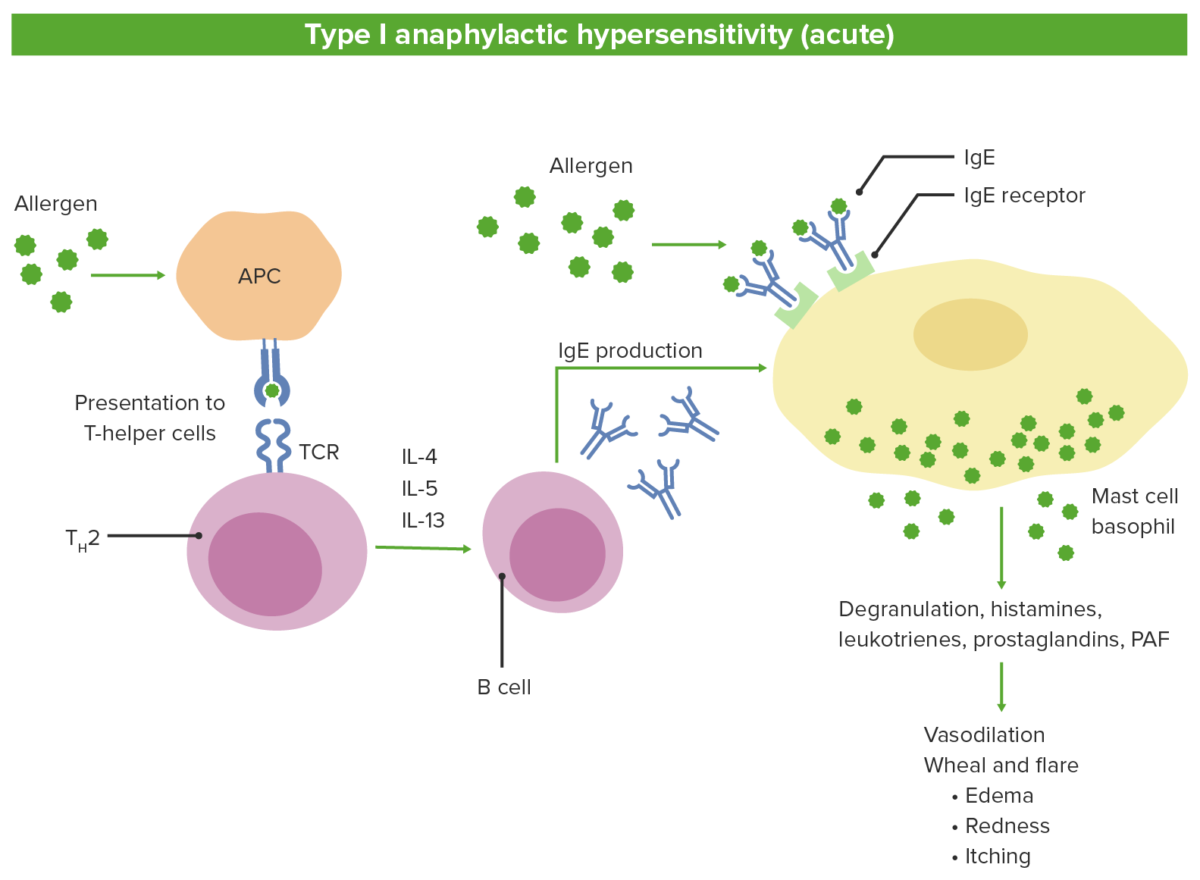
Pathophysiology of type 1 hypersensitivity:
1. Antigen-presenting cells (APC) recognize the allergen and presents to naive T cells
2. T cells differentiate into Th2 which release the interleukins.
3. Interleukins stimulate the B cells to produce IgE.
4. Antigen-specific IgE binds to mast cells and basophils.
5. Subsequent exposure to the same antigen leads to degranulation and release of mediators.
TCR: T cell receptor
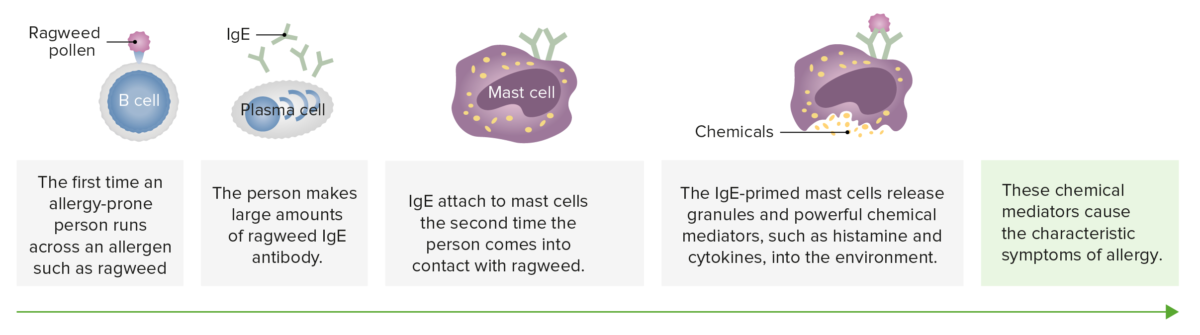
Mast cells are involved in allergy. Allergies such as pollen allergy are related to the antibody known as IgE. Like other antibodies, each IgE antibody is specific; one acts against oak pollen, another against ragweed.
Image by Lecturio.| Type I | Type II | Type III | Type IV |
|---|---|---|---|
| IgE-mediated hypersensitivity | IgG-mediated cytotoxic Cytotoxic Parvovirus B19 hypersensitivity | Immune complex-mediated hypersensitivity Immune complex-mediated hypersensitivity Type III hypersensitivity, also known as immune complex-mediated hypersensitivity, occurs when antibodies and antigens form immune complexes in circulation and deposit in susceptible tissues. The complement system triggers the immune response, leading to leukocyte recruitment and tissue injury. Type III Hypersensitivity Reaction | Cell-mediated hypersensitivity |
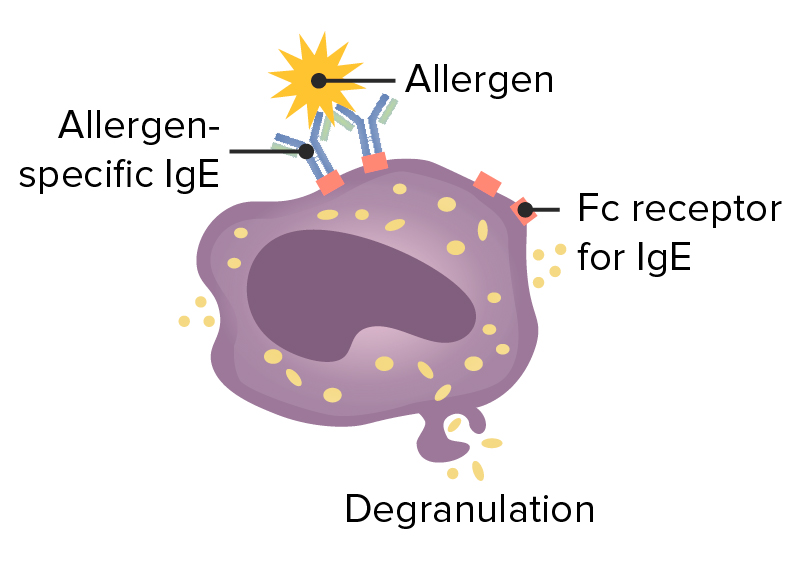
| IgE IgE An immunoglobulin associated with mast cells. Overexpression has been associated with allergic hypersensitivity. Immunoglobulins: Types and Functions is bound to mast cells Mast cells Granulated cells that are found in almost all tissues, most abundantly in the skin and the gastrointestinal tract. Like the basophils, mast cells contain large amounts of histamine and heparin. Unlike basophils, mast cells normally remain in the tissues and do not circulate in the blood. Mast cells, derived from the bone marrow stem cells, are regulated by the stem cell factor. Innate Immunity: Phagocytes and Antigen Presentation via its fragment crystallizable ( Fc Fc Crystallizable fragments composed of the carboxy-terminal halves of both immunoglobulin heavy chains linked to each other by disulfide bonds. Fc fragments contain the carboxy-terminal parts of the heavy chain constant regions that are responsible for the effector functions of an immunoglobulin (complement fixation, binding to the cell membrane via fc receptors, and placental transport). This fragment can be obtained by digestion of immunoglobulins with the proteolytic enzyme papain. Immunoglobulins: Types and Functions) portion. When an allergen binds to these antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, crosslinking of IgE IgE An immunoglobulin associated with mast cells. Overexpression has been associated with allergic hypersensitivity. Immunoglobulins: Types and Functions induces degranulation. | Cells are destroyed by bound antibody, either by activation of complement or by a NK cell with an Fc Fc Crystallizable fragments composed of the carboxy-terminal halves of both immunoglobulin heavy chains linked to each other by disulfide bonds. Fc fragments contain the carboxy-terminal parts of the heavy chain constant regions that are responsible for the effector functions of an immunoglobulin (complement fixation, binding to the cell membrane via fc receptors, and placental transport). This fragment can be obtained by digestion of immunoglobulins with the proteolytic enzyme papain. Immunoglobulins: Types and Functions receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors for the antibody (antibody-dependent cellular cytotoxicity). | Antigen-antibody complexes are deposited in tissues, causing activation of complement, which attracts neutrophils Neutrophils Granular leukocytes having a nucleus with three to five lobes connected by slender threads of chromatin, and cytoplasm containing fine inconspicuous granules and stainable by neutral dyes. Innate Immunity: Phagocytes and Antigen Presentation to the site. | Th1 Th1 A subset of helper-inducer T-lymphocytes which synthesize and secrete interleukin-2; interferon-gamma; and interleukin-12. Due to their ability to kill antigen-presenting cells and their lymphokine-mediated effector activity, th1 cells are associated with vigorous delayed-type hypersensitivity reactions. T cells: Types and Functions cells secrete cytokines Cytokines Non-antibody proteins secreted by inflammatory leukocytes and some non-leukocytic cells, that act as intercellular mediators. They differ from classical hormones in that they are produced by a number of tissue or cell types rather than by specialized glands. They generally act locally in a paracrine or autocrine rather than endocrine manner. Adaptive Immune Response, which activate macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation and cytotoxic Cytotoxic Parvovirus B19 T cells T cells Lymphocytes responsible for cell-mediated immunity. Two types have been identified – cytotoxic (t-lymphocytes, cytotoxic) and helper T-lymphocytes (t-lymphocytes, helper-inducer). They are formed when lymphocytes circulate through the thymus gland and differentiate to thymocytes. When exposed to an antigen, they divide rapidly and produce large numbers of new T cells sensitized to that antigen. T cells: Types and Functions and can cause macrophage accumulation at the site. |
| Causes localized and systemic anaphylaxis; seasonal allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency including hay fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever; food allergies Allergies A medical specialty concerned with the hypersensitivity of the individual to foreign substances and protection from the resultant infection or disorder. Selective IgA Deficiency, such as those to shellfish and peanuts; hives Hives Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives); and eczema Eczema Atopic dermatitis, also known as eczema, is a chronic, relapsing, pruritic, inflammatory skin disease that occurs more frequently in children, although adults can also be affected. The condition is often associated with elevated serum levels of IgE and a personal or family history of atopy. Skin dryness, erythema, oozing, crusting, and lichenification are present. Atopic Dermatitis (Eczema). | Red blood cells Red blood cells Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology are destroyed by complement and antibody during a transfusion of mismatched type or during erythroblastosis fetalis Erythroblastosis fetalis Hemolytic disease of the fetus and newborn (HDFN), also known as erythroblastosis fetalis, is caused by maternal IgG antibody destruction of the fetal RBCs. Rhesus (Rh) blood group incompatibility (frequently triggered by D antigen) and ABO incompatibility are common causes. Hemolytic Disease of the Fetus and Newborn. | The most common forms of immune complex disease Immune complex disease Group of diseases mediated by the deposition of large soluble complexes of antigen and antibody with resultant damage to tissue. Besides serum sickness and the arthus reaction, evidence supports a pathogenic role for immune complexes in many other immune system diseases including glomerulonephritis, systemic lupus erythematosus (lupus erythematosus, systemic) and polyarteritis nodosa. Membranoproliferative Glomerulonephritis include glomerulonephritis, rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, and systemic lupus erythematosus Systemic lupus erythematosus Systemic lupus erythematosus (SLE) is a chronic autoimmune, inflammatory condition that causes immune-complex deposition in organs, resulting in systemic manifestations. Women, particularly those of African American descent, are more commonly affected. Systemic Lupus Erythematosus. | The most common forms are contact dermatitis Contact dermatitis A type of acute or chronic skin reaction in which sensitivity is manifested by reactivity to materials or substances coming in contact with the skin. It may involve allergic or non-allergic mechanisms. Male Genitourinary Examination, tuberculin Tuberculin A protein extracted from boiled culture of tubercle bacilli (Mycobacterium tuberculosis). It is used in the tuberculin skin test (tuberculin test) for the diagnosis of tuberculosis infection in asymptomatic persons. Type IV Hypersensitivity Reaction reaction, diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus type I, multiple sclerosis Sclerosis A pathological process consisting of hardening or fibrosis of an anatomical structure, often a vessel or a nerve. Wilms Tumor, and rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis. |
Type 1 hypersensitivity
Image: “Figure 1” by Phil Schatz. License: CC BY 4.0, edited by Lecturio.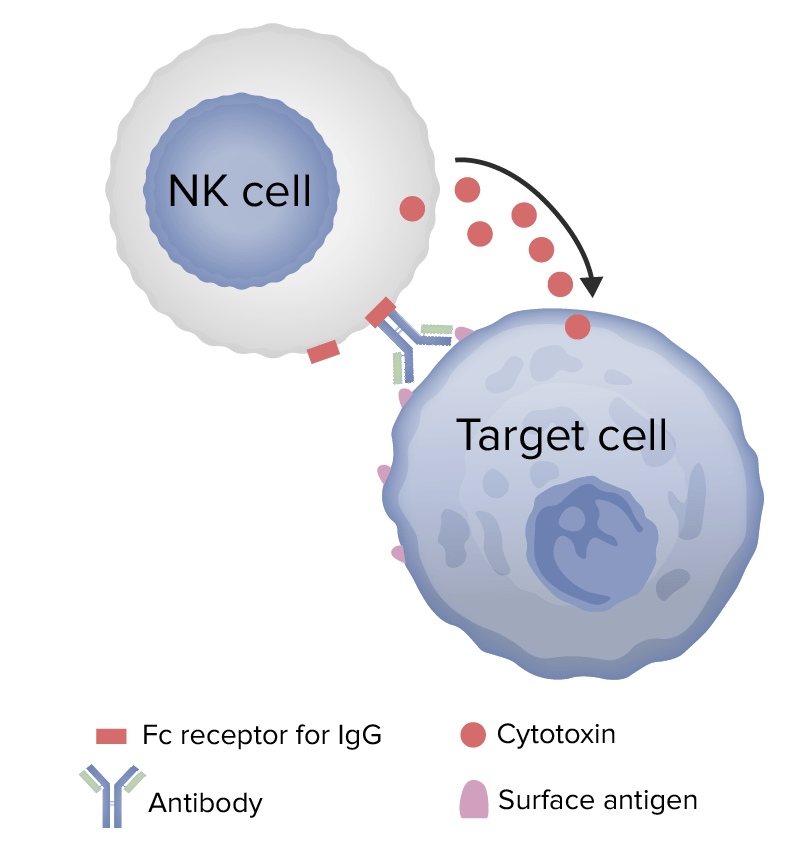
Mechanism of type 2 hypersensitivity
Image by Lecturio.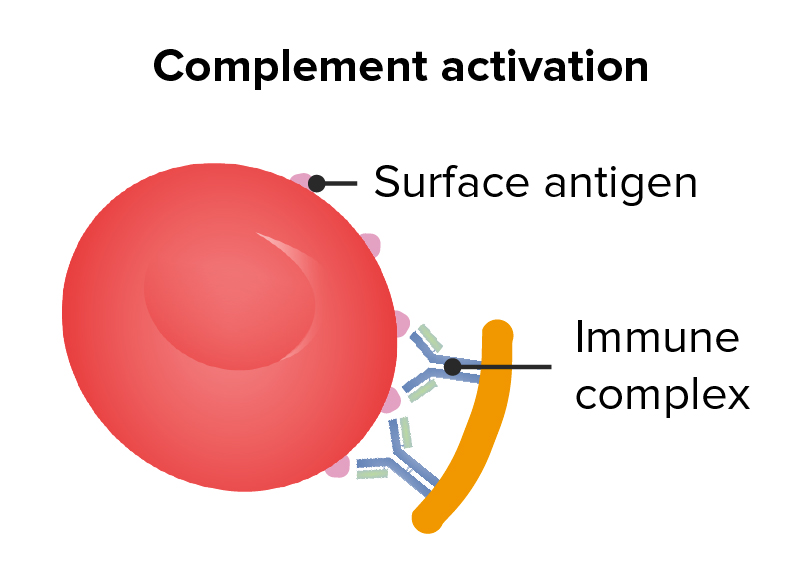
Type 2 hypersensitivity
Image: “Figure 1” by Phil Schatz. License: CC BY 4.0, edited by Lecturio.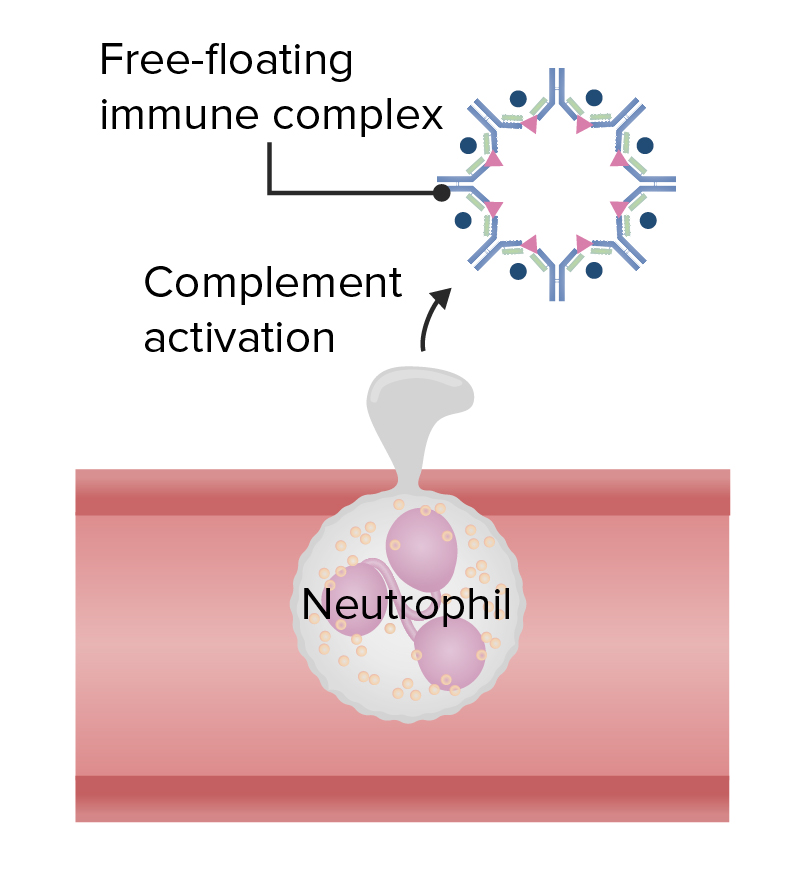
Type 3 hypersensitivity
Image: “Figure 1” by Phil Schatz. License: CC BY 4.0, edited by Lecturio.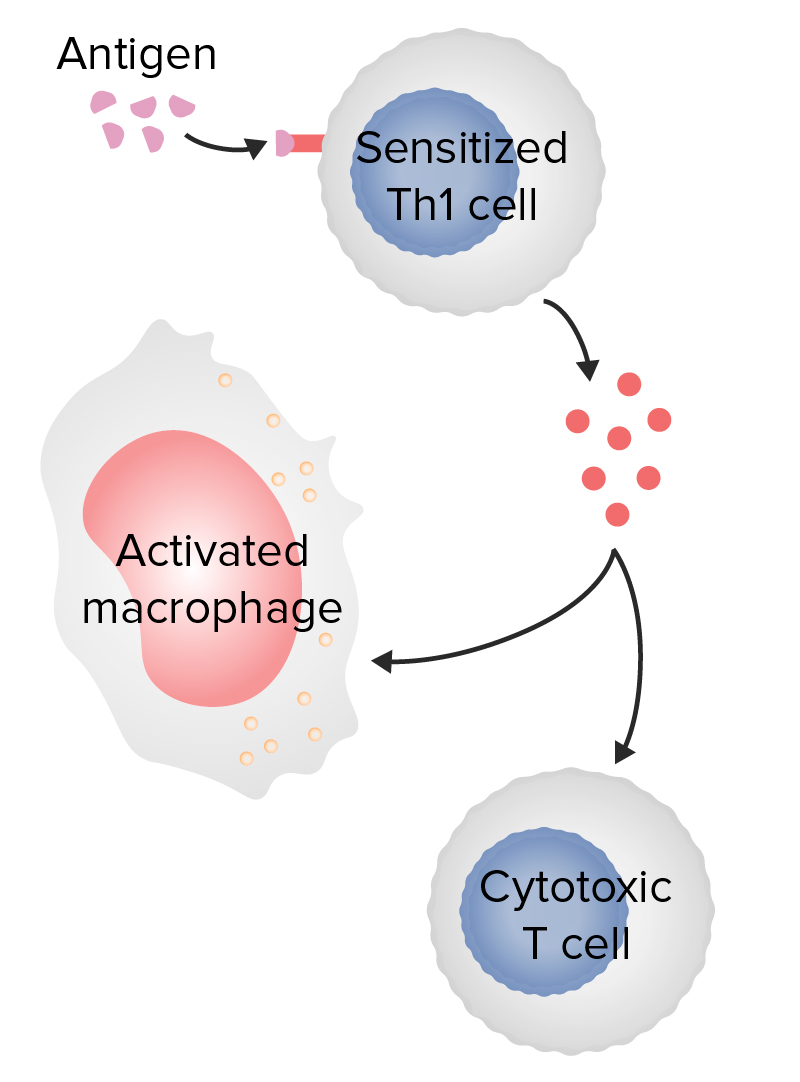
Type 4 hypersensitivity
Image: “Figure 1” by Phil Schatz. License: CC BY 4.0, edited by Lecturio.| Anaphylactic symptoms | Effects of histamine |
|---|---|
| Rhinitis Rhinitis Inflammation of the nasal mucosa, the mucous membrane lining the nasal cavities. Rhinitis, conjunctivitis Conjunctivitis Conjunctivitis is a common inflammation of the bulbar and/or palpebral conjunctiva. It can be classified into infectious (mostly viral) and noninfectious conjunctivitis, which includes allergic causes. Patients commonly present with red eyes, increased tearing, burning, foreign body sensation, and photophobia. Conjunctivitis | Peripheral vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs, increased vascular permeability, increased mucus secretion Secretion Coagulation Studies |
| Erythema Erythema Redness of the skin produced by congestion of the capillaries. This condition may result from a variety of disease processes. Chalazion | Accumulation of blood in the capillary bed from vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs |
| Pulmonary edema Pulmonary edema Pulmonary edema is a condition caused by excess fluid within the lung parenchyma and alveoli as a consequence of a disease process. Based on etiology, pulmonary edema is classified as cardiogenic or noncardiogenic. Patients may present with progressive dyspnea, orthopnea, cough, or respiratory failure. Pulmonary Edema, angioedema Angioedema Angioedema is a localized, self-limited (but potentially life-threatening), nonpitting, asymmetrical edema occurring in the deep layers of the skin and mucosal tissue. The common underlying pathophysiology involves inflammatory mediators triggering significant vasodilation and increased capillary permeability. Angioedema, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension | Fluid shift Fluid Shift Translocation of body fluids from one compartment to another, such as from the vascular to the interstitial compartments. Fluid shifts are associated with profound changes in vascular permeability and water-electrolyte imbalance. The shift can also be from the lower body to the upper body as in conditions of weightlessness. Volume Depletion and Dehydration into the stroma from increased vessel permeability, vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs |
| Pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema), urticaria Urticaria Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives), or hives Hives Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives) | Fluid extravasation into dermis Dermis A layer of vascularized connective tissue underneath the epidermis. The surface of the dermis contains innervated papillae. Embedded in or beneath the dermis are sweat glands; hair follicles; and sebaceous glands. Skin: Structure and Functions; increase trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation of skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology nerves (itch) |
| Bronchospasm Bronchospasm Asthma Drugs, bronchoconstriction | Bronchial smooth muscle contraction Smooth muscle contraction Smooth muscle is primarily found in the walls of hollow structures and some visceral organs, including the walls of the vasculature, GI, respiratory, and genitourinary tracts. Smooth muscle contracts more slowly and is regulated differently than skeletal muscle. Smooth muscle can be stimulated by nerve impulses, hormones, metabolic factors (like pH, CO2 or O2 levels), its own intrinsic pacemaker ability, or even mechanical stretch. Smooth Muscle Contraction, increased mucus secretion Secretion Coagulation Studies |