Antihistamines are drugs that target histamine receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors, particularly H1 and H2 receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors. H1 antagonists are competitive and reversible inhibitors of H1 receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors. First-generation antihistamines cross the blood-brain barrier Blood-brain barrier Specialized non-fenestrated tightly-joined endothelial cells with tight junctions that form a transport barrier for certain substances between the cerebral capillaries and the brain tissue. Systemic and Special Circulations and can cause sedation. Additionally, with the ability to block muscarinic receptors Muscarinic Receptors Asthma Drugs, anticholinergic Anticholinergic Anticholinergic drugs block the effect of the neurotransmitter acetylcholine at the muscarinic receptors in the central and peripheral nervous systems. Anticholinergic agents inhibit the parasympathetic nervous system, resulting in effects on the smooth muscle in the respiratory tract, vascular system, urinary tract, GI tract, and pupils of the eyes. Anticholinergic Drugs effects are also observed with this class of drugs. The 1st-generation H1 antagonists include chlorpheniramine, diphenhydramine, dimenhydrinate, and meclizine. Second-generation antihistamines generally do not cause drowsiness as these agents do not cross the blood-brain barrier Blood-brain barrier Specialized non-fenestrated tightly-joined endothelial cells with tight junctions that form a transport barrier for certain substances between the cerebral capillaries and the brain tissue. Systemic and Special Circulations. Examples of 2nd-generation antihistamines include loratadine, desloratadine, and cetirizine. Due to their antihistaminic activity, H1 antagonists are prescribed to treat allergy Allergy An abnormal adaptive immune response that may or may not involve antigen-specific IgE Type I Hypersensitivity Reaction symptoms. Moreover, 1st-generation antihistamines are also used to treat motion sickness, nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, and vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia. H2 antagonists (blockers) target the H2 receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors, reducing gastric acid Gastric acid Hydrochloric acid present in gastric juice. Gastroesophageal Reflux Disease (GERD) production and secretion Secretion Coagulation Studies. Thus, the general indications of H2 blockers include treatment of GERD GERD Gastroesophageal reflux disease (GERD) occurs when the stomach acid frequently flows back into the esophagus. This backwash (acid reflux) can irritate the lining of the esophagus, causing symptoms such as retrosternal burning pain (heartburn). Gastroesophageal Reflux Disease (GERD) and gastric and duodenal ulcers.
Last updated: Mar 28, 2025
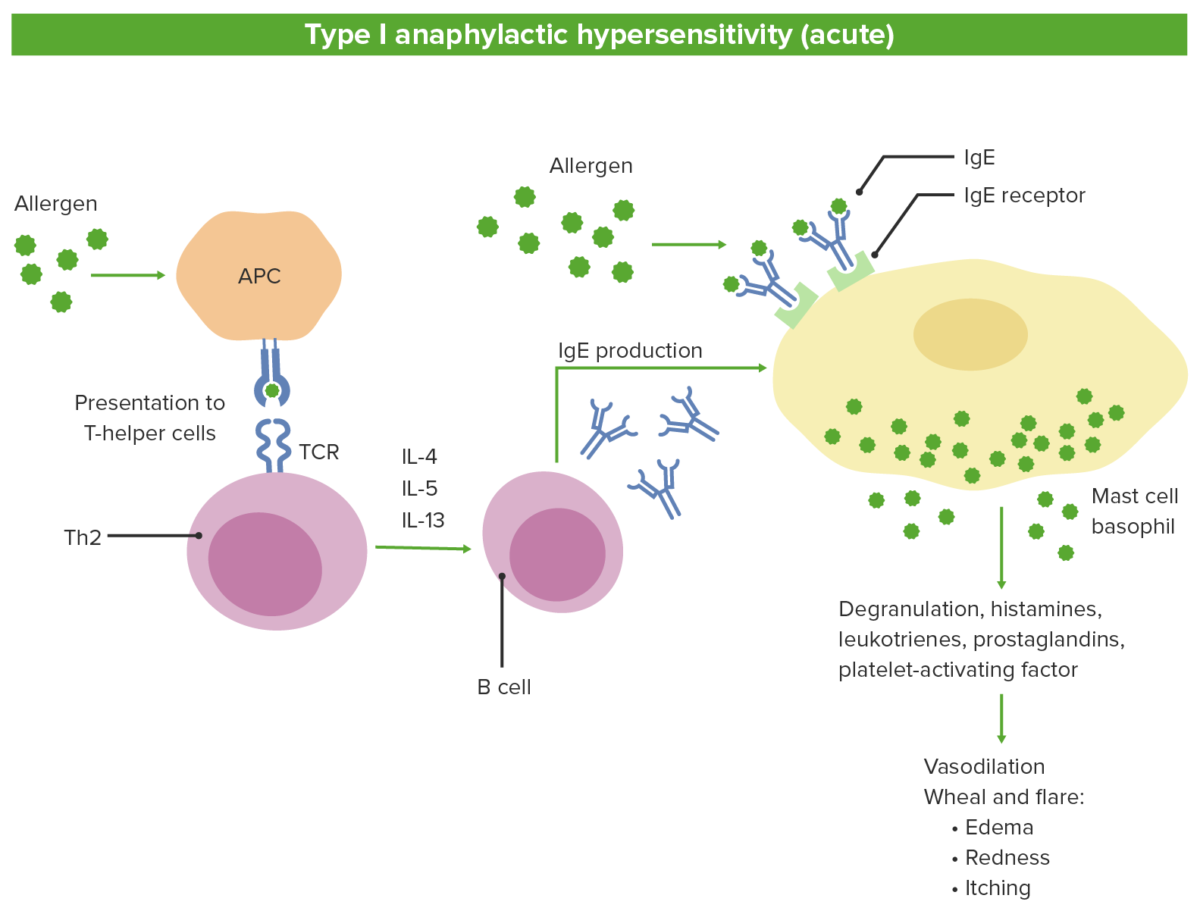
Pathophysiology of type 1 hypersensitivity:
1. Antigen-presenting cells (APCs) recognize the allergen and present to naive T cells
2. T cells differentiate into Th2, which release interleukins.
3. Interleukins stimulate B cells to produce IgE.
4. Antigen-specific IgE binds to mast cells and basophils.
5. Subsequent exposure to the same antigen leads to degranulation and release of mediators.
TCR: T cell receptor
| 1st generation | 2nd generation |
|---|---|
|
|
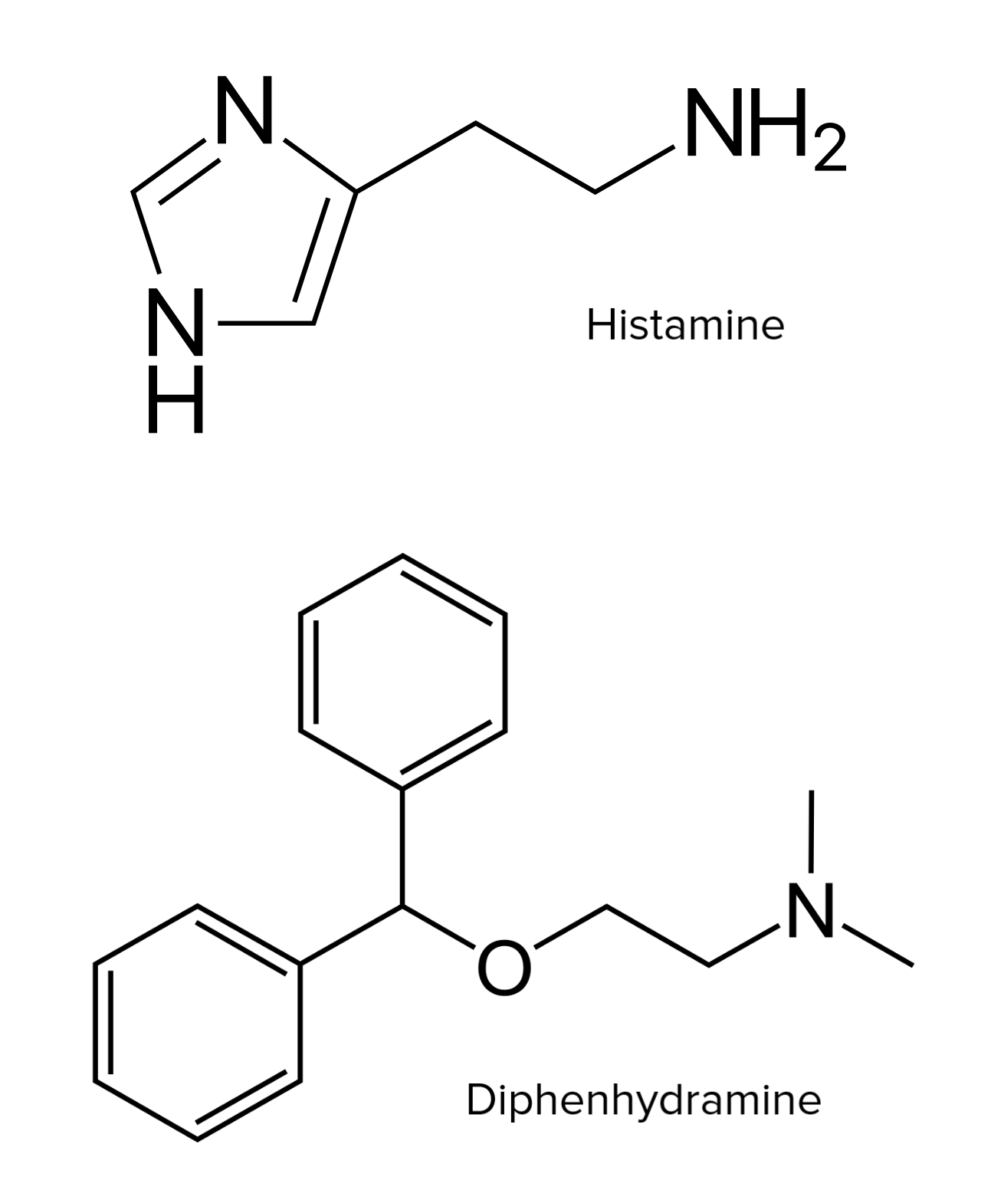
Chemical structures of histamine and diphenhydramine
Image: “Skeletal formula of histamine” by Vaccinationist. License: Public Domain| Type | Drug | Pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics |
|---|---|---|
| 1st generation | Chlorpheniramine |
|
| Diphenhydramine |
|
|
| Meclizine |
|
|
| Promethazine |
|
|
| 2nd generation | Cetirizine |
|
| Loratidine |
|
|
| Olopatadine |
|
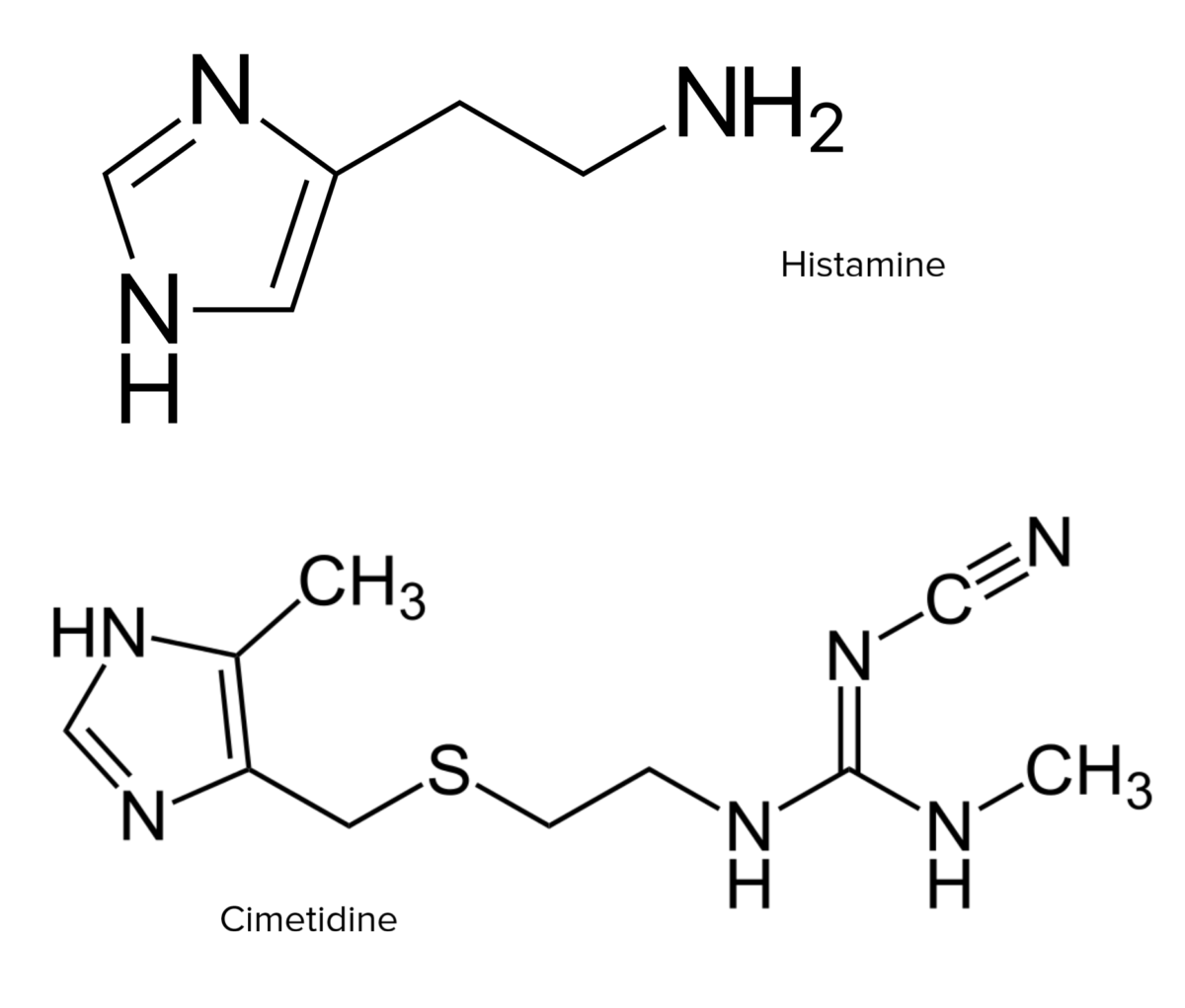
Chemical structures of histamine and cimetidine
Image: “Skeletal formula of histamine” by Vaccinationist. License: Public Domain| Drug | Pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics |
|---|---|
| Cimetidine |
|
| Famotidine |
|
| Nizatidine |
|
| Medication | Mechanism of action | Indication |
|---|---|---|
| 1st-generation H1 antagonists (sedating) |
|
|
| 2nd-generation H1 antagonists | ||
| H2 antagonists (blockers) | Antagonists of H2 receptors Receptors Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors located on gastric parietal cells Parietal cells Rounded or pyramidal cells of the gastric glands. They secrete hydrochloric acid and produce gastric intrinsic factor, a glycoprotein that binds vitamin B12. Stomach: Anatomy |
|