Muscle tissue is one of the basic tissue types. Histologically, the muscles of the body can be classified into 3 types: skeletal, smooth, and cardiac. The 3 types of muscle tissue are based on the morphologic and functional properties of the cells. One of the defining characteristics of muscle tissue is its contractility, which generates forces that move the musculoskeletal system as well as cause movement in the vasculature and multiple organ systems. This contractility is due to specialized proteins Proteins Linear polypeptides that are synthesized on ribosomes and may be further modified, crosslinked, cleaved, or assembled into complex proteins with several subunits. The specific sequence of amino acids determines the shape the polypeptide will take, during protein folding, and the function of the protein. Energy Homeostasis known as myofilaments, which create organized structures that have the ability to lengthen and contract.
Last updated: Apr 14, 2025
Muscle tissue is made up of muscle cells known as myocytes, which is one of the primary tissue types.
There are 3 types of muscle tissue based on morphologic and functional differences:
The muscle is arranged in a hierarchical structure:
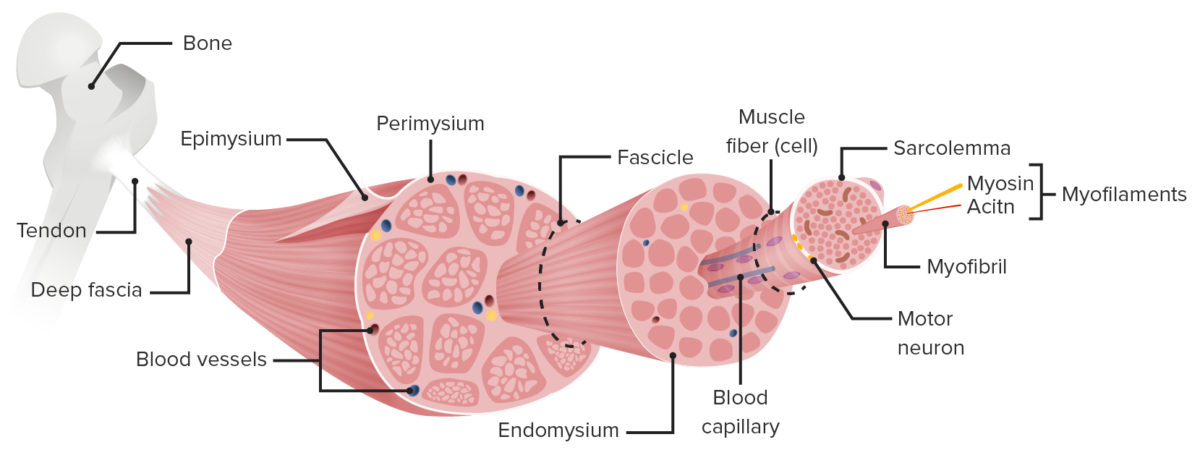
Structure of skeletal muscle
Image by Lecturio.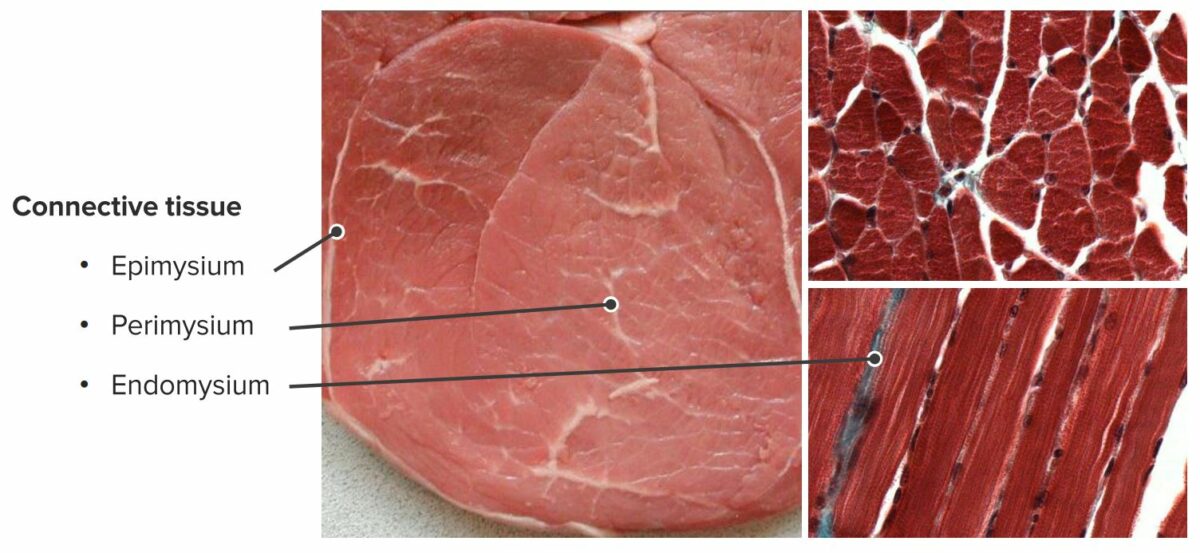
Connective tissue surrounding skeletal muscles
Image by Geoffrey Meyer, PhD.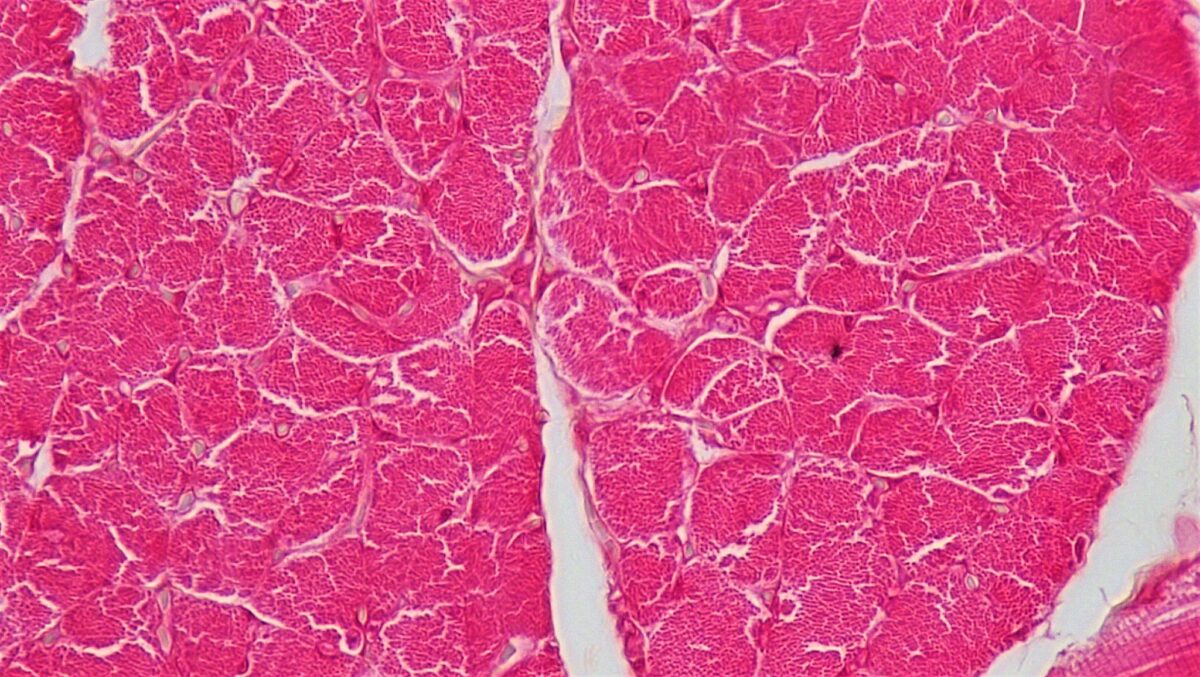
Cross section of skeletal muscle:
This image shows the muscle fibers enveloped in connective tissue. Note the bundles of muscle fascicles within the larger muscle and the individual muscle fibers visible within the fascicles.
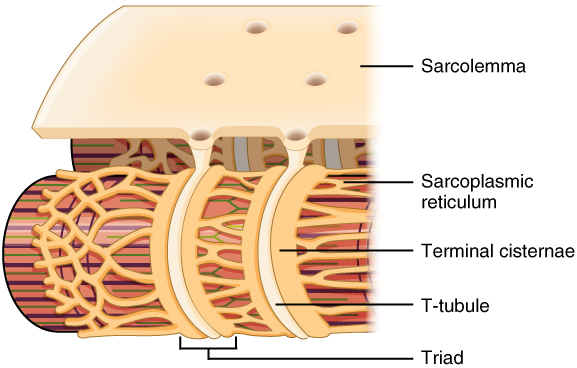
T tubules and their associations with the sarcoplasmic reticulum:
Note how the T tubules are channels through the sarcolemma that come in direct contact with the terminal cisternae of the sarcoplasmic reticulum.
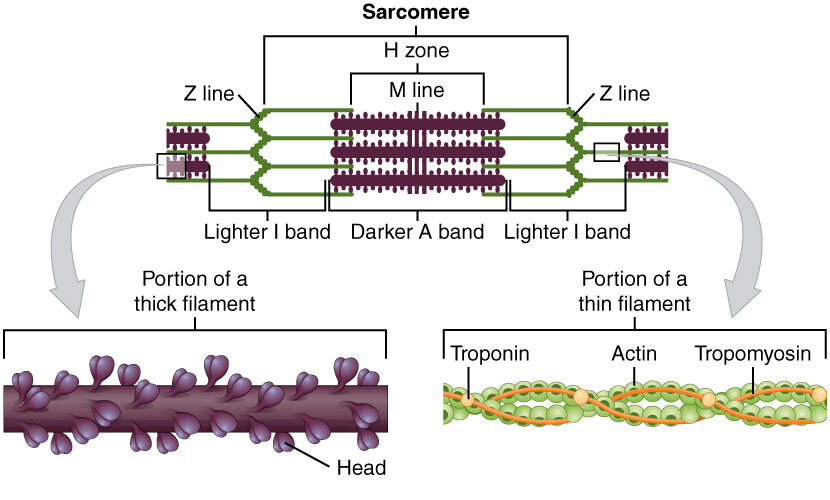
Diagram depicting the microscopic structure of sarcomeres, actin, and myosin
Image: “The sarcomere, the region from one Z-line to the next Z-line, is the functional unit of a skeletal muscle fiber” by OpenStax College. License: CC BY 4.0The myofibrils are organized in a pattern that creates different bands and zones when viewed under microscopy. These bands are created by overlapping actin Actin Filamentous proteins that are the main constituent of the thin filaments of muscle fibers. The filaments (known also as filamentous or f-actin) can be dissociated into their globular subunits; each subunit is composed of a single polypeptide 375 amino acids long. This is known as globular or g-actin. In conjunction with myosins, actin is responsible for the contraction and relaxation of muscle. Skeletal Muscle Contraction and myosin Myosin A diverse superfamily of proteins that function as translocating proteins. They share the common characteristics of being able to bind actins and hydrolyze mgATP. Myosins generally consist of heavy chains which are involved in locomotion, and light chains which are involved in regulation. Within the structure of myosin heavy chain are three domains: the head, the neck and the tail. The head region of the heavy chain contains the actin binding domain and mgATPase domain which provides energy for locomotion. The neck region is involved in binding the light-chains. The tail region provides the anchoring point that maintains the position of the heavy chain. The superfamily of myosins is organized into structural classes based upon the type and arrangement of the subunits they contain. Skeletal Muscle Contraction strands.
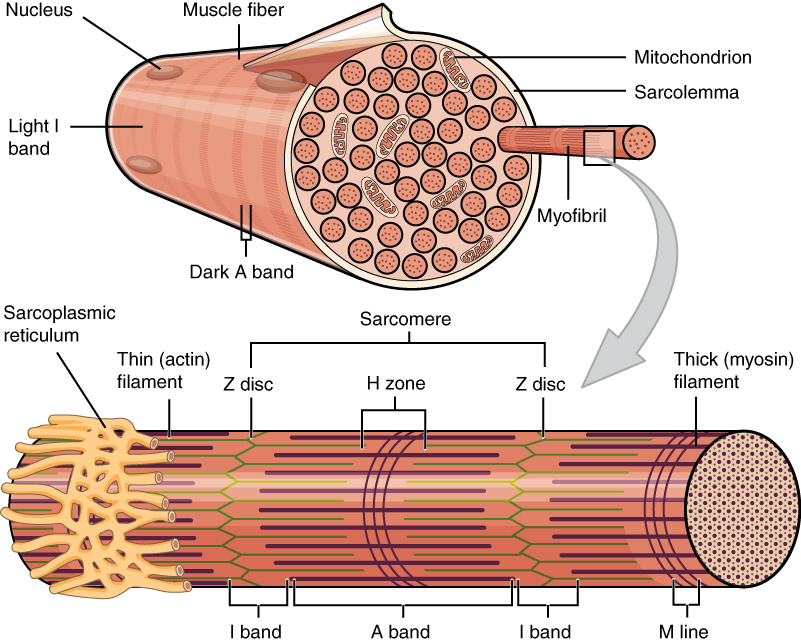
Structure of muscle fibers and myofibrils
Image: “A skeletal muscle fiber is surrounded by a plasma membrane called the sarcolemma” by OpenStax College. License: CC BY 4.0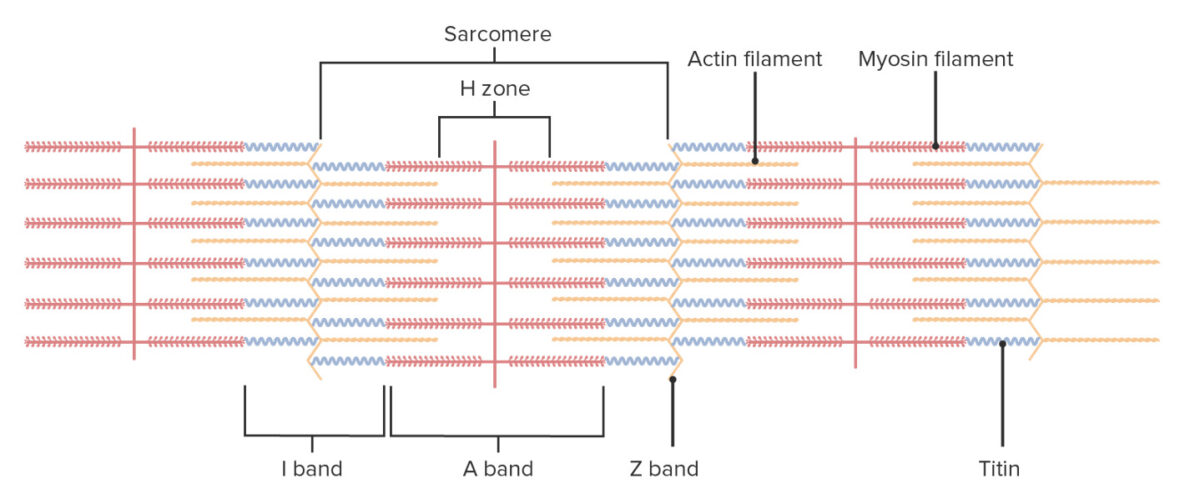
Organization of muscle fiber
Image by Lecturio.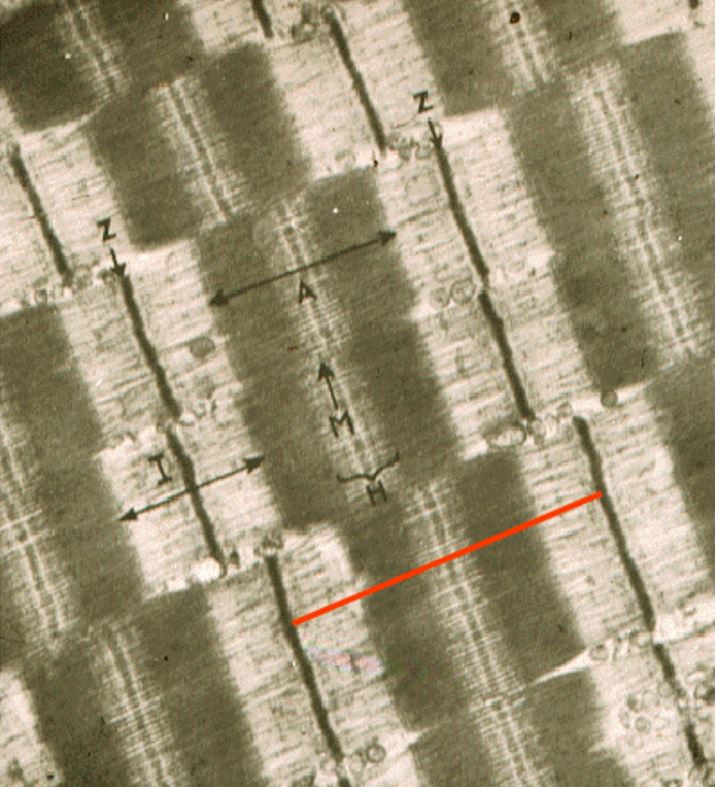
Electron micrograph of a sarcomere, the functional unit of the myofibril, which is the segment between Z lines:
Also note the labeled A, I, M, and H bands.
There are 3 primary types of skeletal muscle fibers, found in different muscles throughout the body based on their function.
Skeletal muscle cell contraction requires stimulation by an action potential Action Potential Abrupt changes in the membrane potential that sweep along the cell membrane of excitable cells in response to excitation stimuli. Membrane Potential from motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology neurons Neurons The basic cellular units of nervous tissue. Each neuron consists of a body, an axon, and dendrites. Their purpose is to receive, conduct, and transmit impulses in the nervous system. Nervous System: Histology.
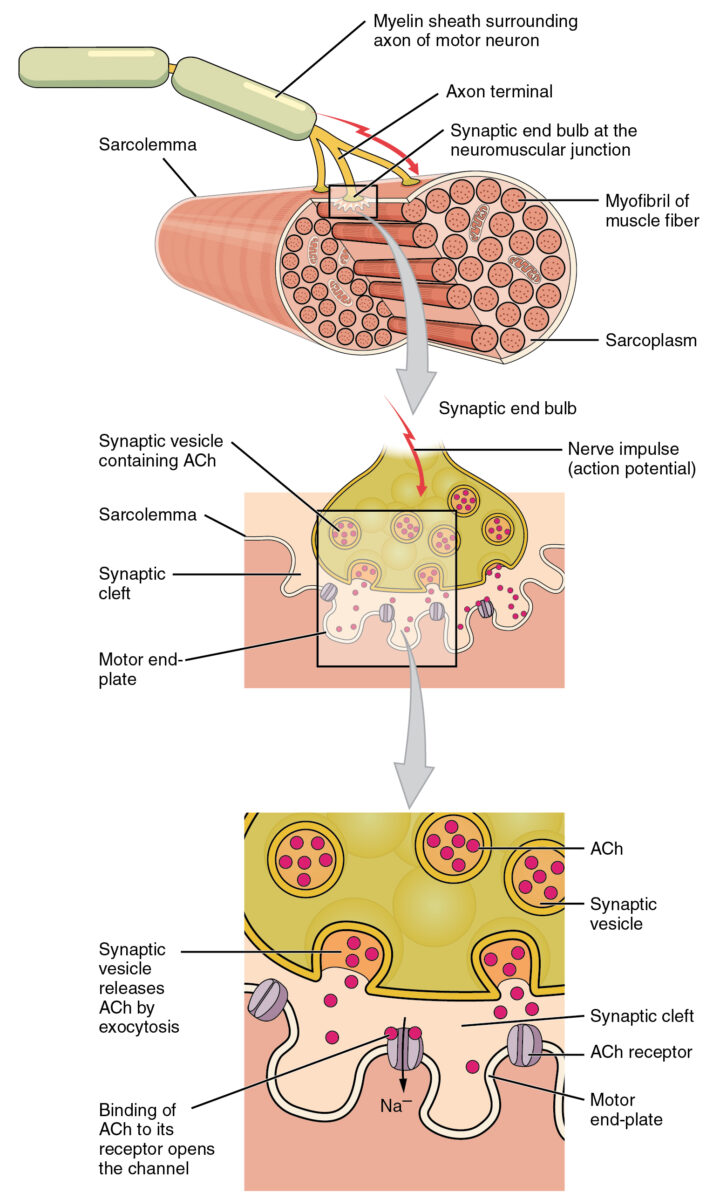
Motor end plate and innervation
ACh: acetylcholine
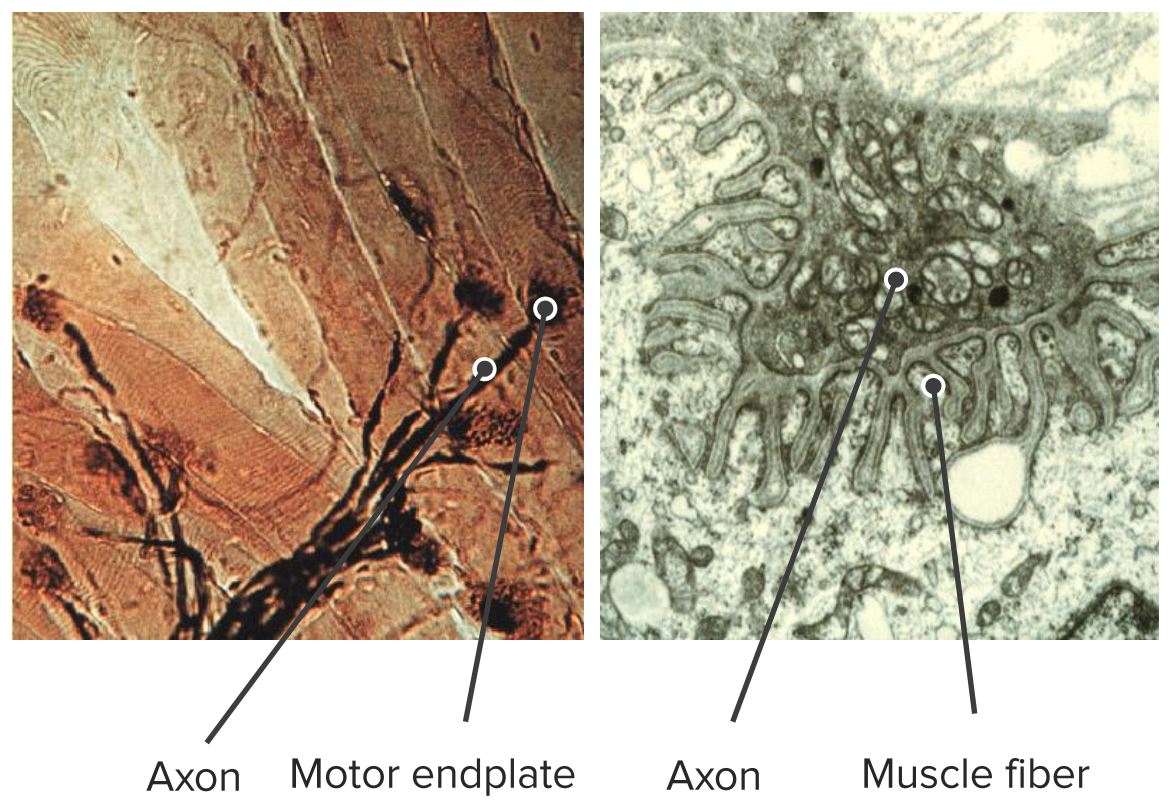
Electron micrograph showing the neuromuscular junction
Image by Geoffrey Meyer, PhD.There are several different types of organizational patterns based on the arrangement of bundles the muscle fascicles:
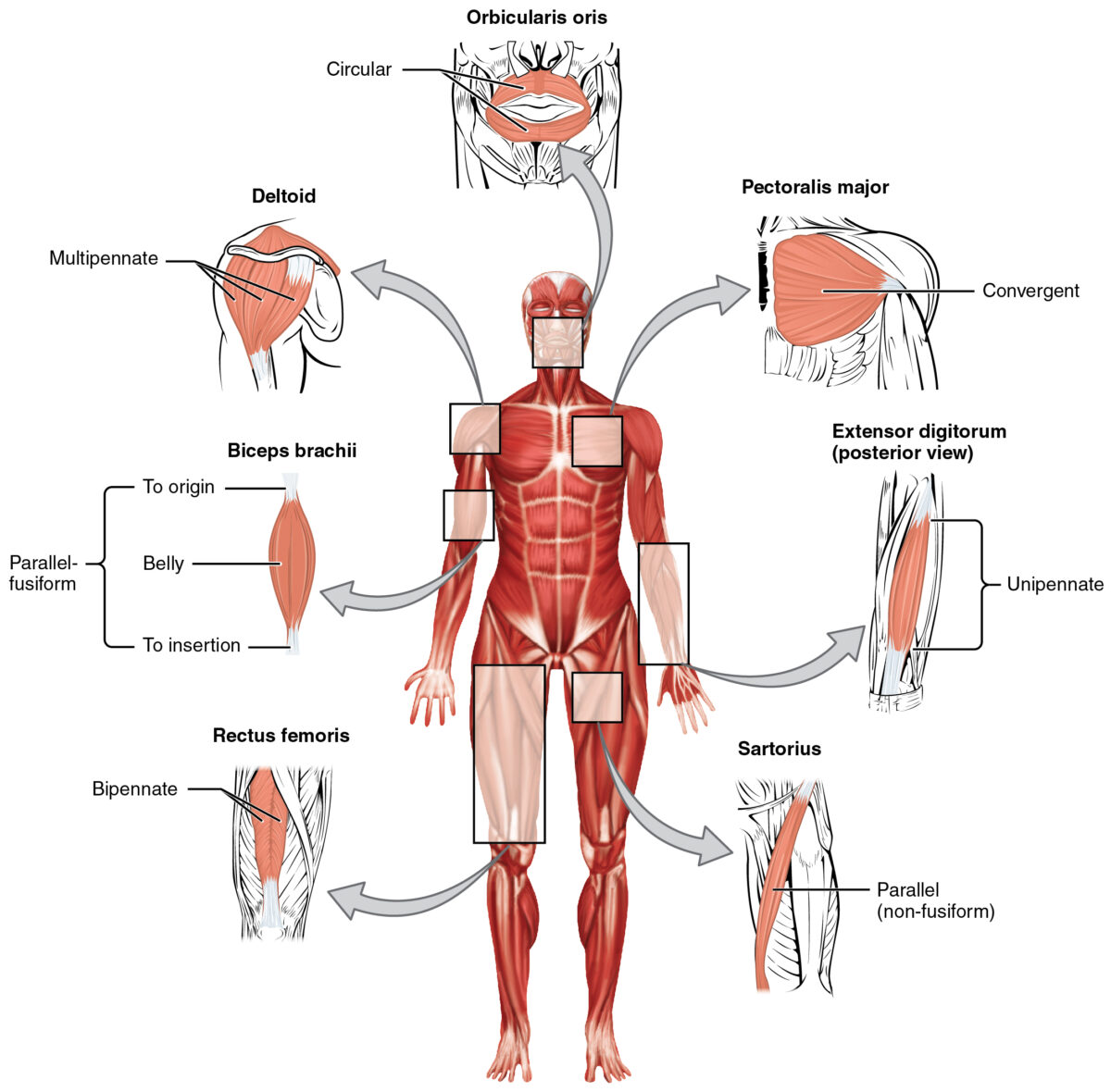
Types of organization within muscles
Image: “The skeletal muscles of the body typically come in seven different general shapes” by OpenStax College. License: CC BY 4.0Smooth muscle is primarily found in the walls of hollow structures, including:
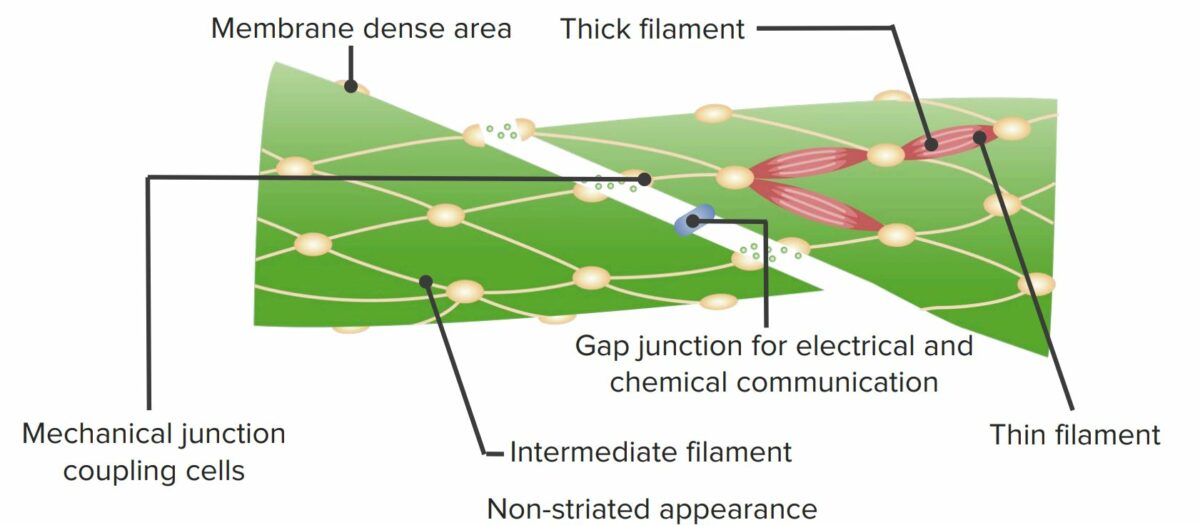
Structure of the smooth muscle cell
Image by Lecturio.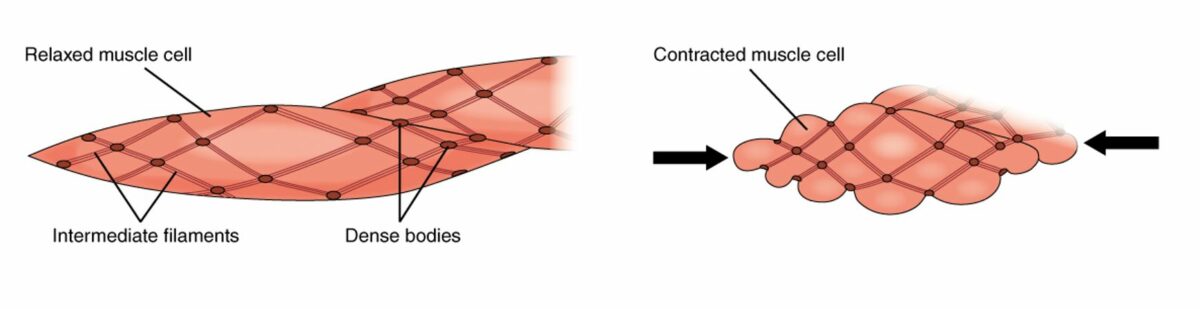
Smooth muscle cells in relaxed (left) and contracted (right) states
Image: “The dense bodies and intermediate filaments are networked through the sarcoplasm” by OpenStax College. License: CC BY 4.0
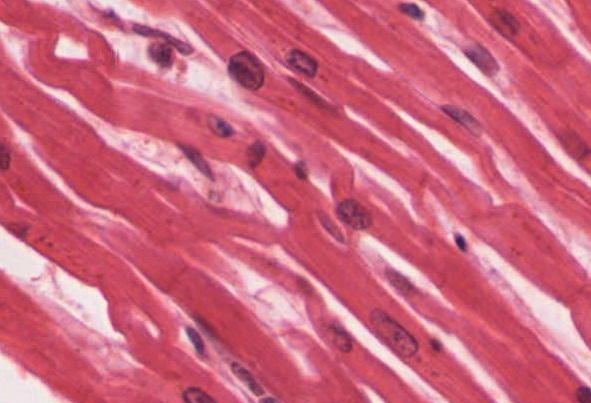
Histologic slide shows smooth muscle that contains a centrally located oval nucleus
Image: “Smooth muscle tissue is found around organs in the digestive, respiratory, reproductive tracts and the iris of the eye” by Regents of University of Michigan Medical School/OpenStax College. License: CC BY 4.0, cropped by Lecturio.There are 2 primary types of smooth muscle tissue:
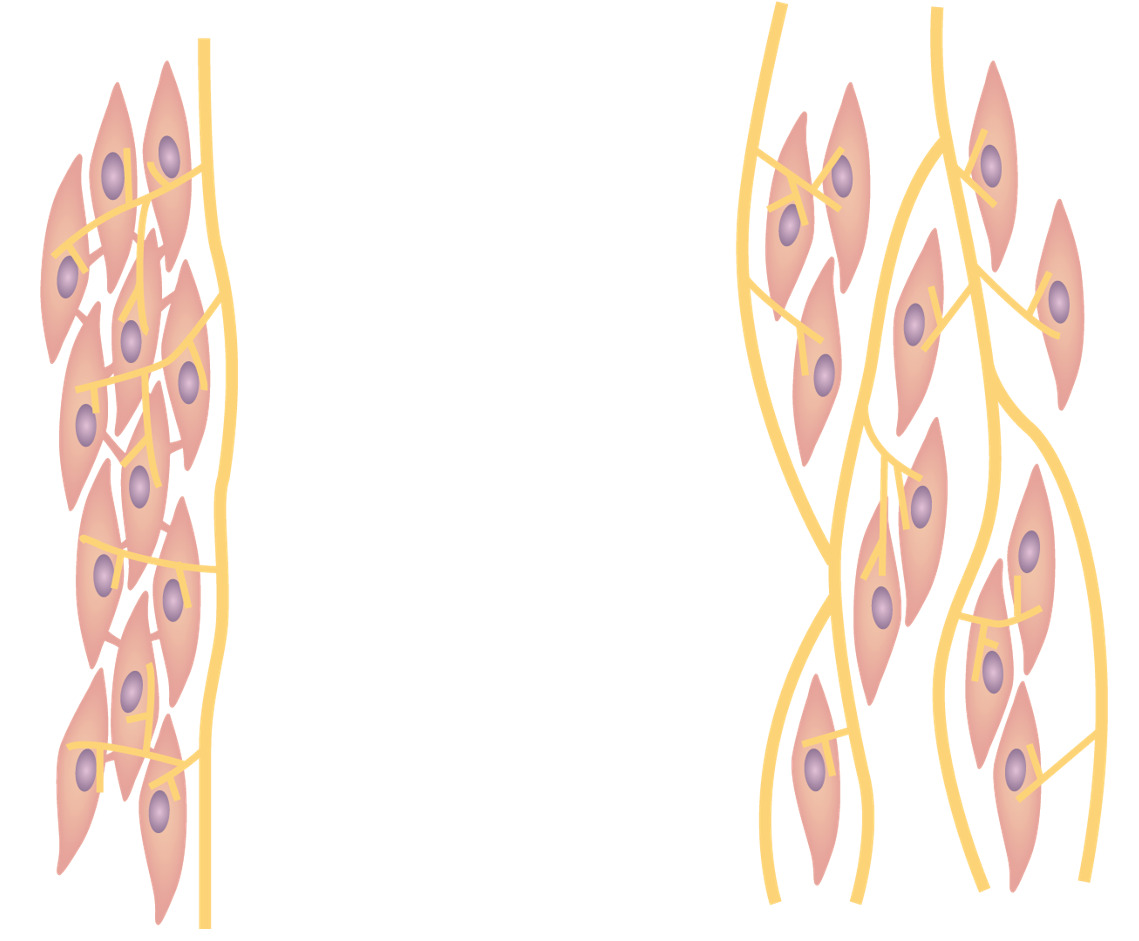
Smooth muscle:
Left: Single-unit type, with cells connected via gap junctions
Right: Multiple-unit type, with each cell separated by a basement membrane
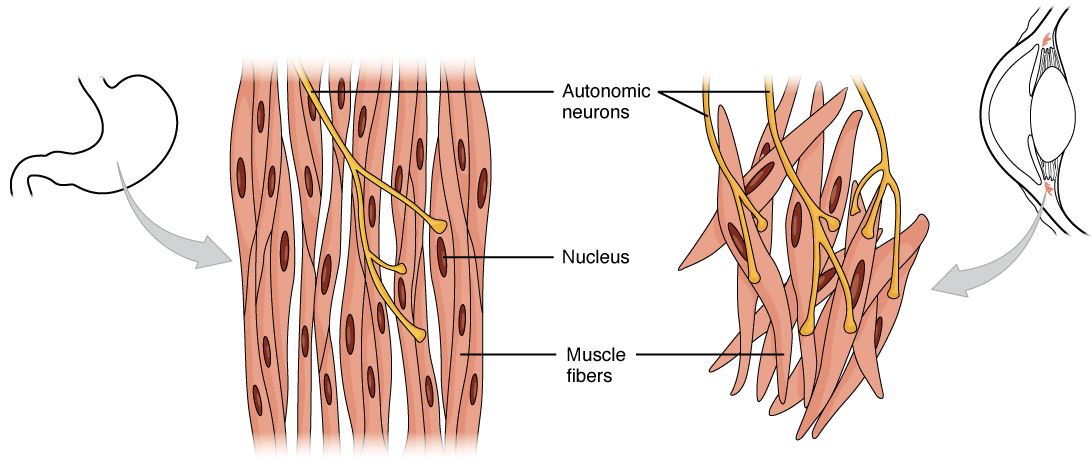
Single-unit types of smooth muscle contain more gap junctions, allowing a more continuous contraction pattern, such as in the muscles controlling the stomach.
Multiple-unit types of smooth muscle are single fibers with minimal gap junctions, resulting in cells that each contract individually.
Cardiac muscle tissue demonstrating interwoven, whorled appearance that causes a characteristic wave of contraction.
Image: “Cardiac muscle tissue is only found in the heart” by OpenStax College. License: CC BY 4.0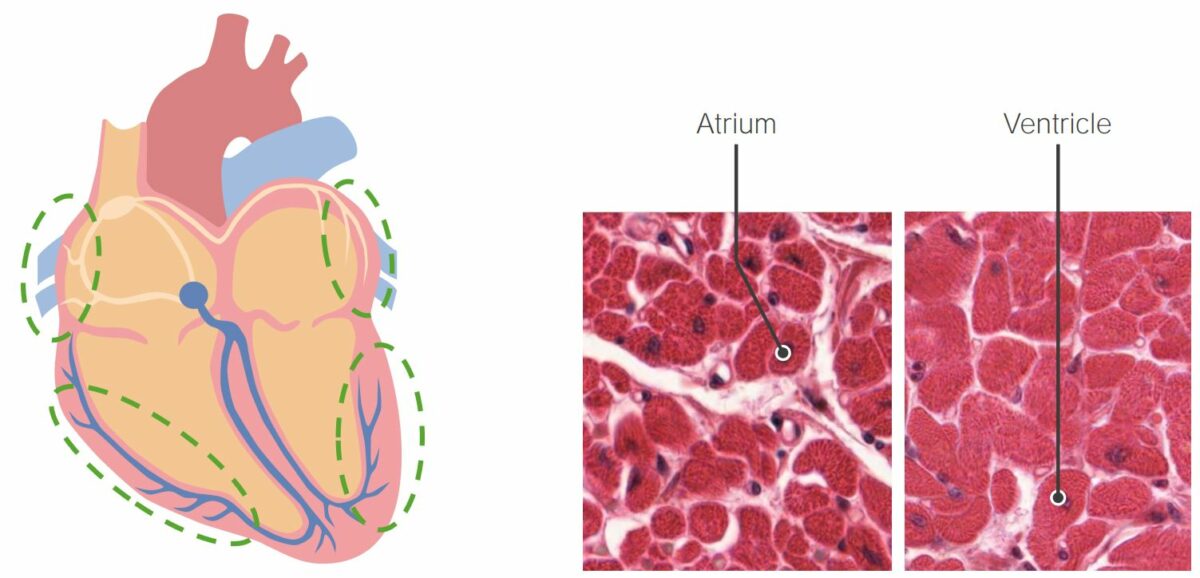
The thickness of the cardiac muscle fibers in the ventricles is greater than that of the fibers of the atrium. This is related to the ventricles’ role in pumping blood through the entire cardiovascular system.
Image by Lecturio/Geoffrey Meyer, PhD.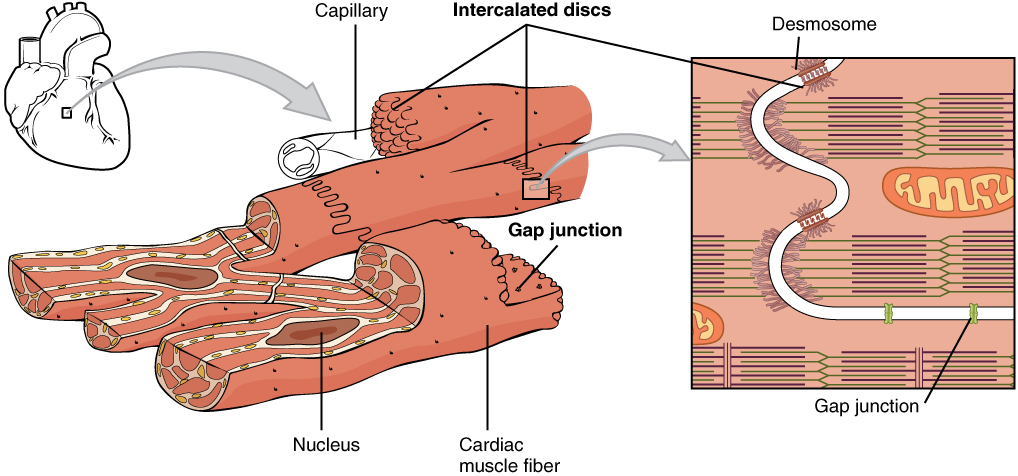
Structure of the intercalated discs within cardiac muscle
Image: “Intercalated discs are part of the cardiac muscle sarcolemma and they contain gap junctions and desmosomes” by OpenStax College. License: CC BY 4.0| Type | Location | Striated versus nonstriated | Motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology end plates | Characteristics of cells | Control |
|---|---|---|---|---|---|
| Skeletal | Skeletal muscles | Striated | Present |
|
Voluntary |
| Smooth |
|
Nonstriated | Absent |
|
Involuntary |
| Cardiac | Wall of heart | Striated | Absent (connected via intercalated discs) |
|
Involuntary |