A burn is a type of injury to the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and deeper tissues caused by exposure to heat Heat Inflammation, electricity, chemicals, friction, or radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma. Burns are classified according to their depth as superficial (1st-degree), partial-thickness (2nd-degree), full-thickness (3rd-degree), and 4th-degree burns. Management is greatly dependent on the extent of surface area affected and the depth of the burns. Management involves fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome, adequate analgesia Analgesia Methods of pain relief that may be used with or in place of analgesics. Anesthesiology: History and Basic Concepts, and appropriate wound care with the goal of preventing opportunistic infection.
Last updated: Dec 22, 2022
Burns are acute traumatic injuries to the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions or underlying tissue caused by exposure to thermal energy, chemicals, electrical discharge, or radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma.
Burns are described using 2 identifiers—degree and severity:
| Degree of burn | Characteristics | Symptoms | Healing |
|---|---|---|---|
| Superficial burn (1st degree) |
|
Itching to pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways |
|
| Superficial partial burns (2nd degree) |
|
Severe pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways |
|
| Deep superficial burns (2nd degree) |
|
Severe pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | Partial recovery with scar Scar Dermatologic Examination formation |
| Full-thickness burns (3rd degree) |
|
Painless because nerve endings have been destroyed |
|
| Full-thickness/eschar burns (4th degree) |
|
Painless |
|
To determine the severity of the burn, calculate the percentage of TBSA injured:
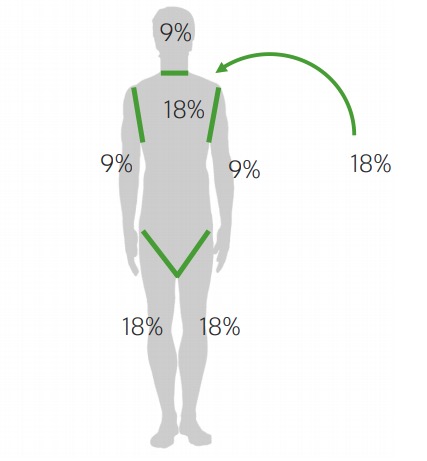
Rule of 9s in adolescents and adults used to determine the TBSA of burn
Image by Lecturio.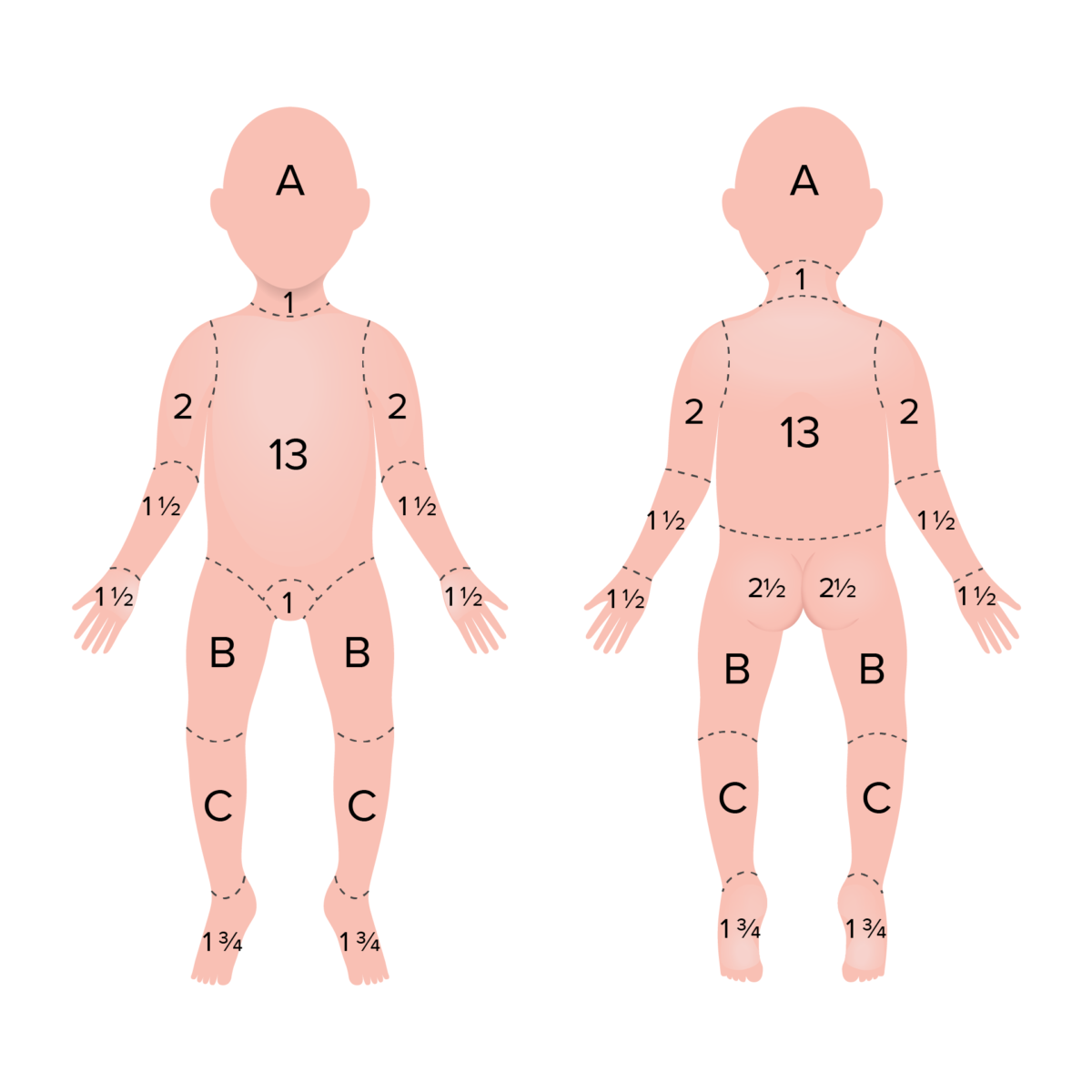
Rule of 9s in children used to determine the TBSA of burn
Infants’ and children’s heads and legs account for a larger and smaller proportion of TBSA, respectively, when compared with adults. As infants and children grow, the percent represented by these areas changes to more closely resemble adults.
Area A represents 8.5% TBSA in a 1-year-old, 6.5% in a 5-year-old, 5.5% in a 10-year-old, and 4.5% in a 15-year-old.
Area B represents 3.25% TBSA in a 1-year-old, 4.0% in a 5-year-old, 4.5% in a 10-year-old, and 4.5% in a 15-year-old.
Area C represents 2.5% TBSA in a 1-year-old, 2.75% in a 5-year-old, 3.0% in a 10-year-old, and 3.25% in a 15-year-old.
| Mild | Moderate | Severe | |
|---|---|---|---|
| Children | < 5% TBSA | 5%–10% TBSA | > 10% TBSA |
| Adult | < 10% TBSA | 10%–20% TBSA | > 20% TBSA |
| Elderly | < 5% TBSA | 5%–10% TBSA | > 10% TBSA |
| All | < 2% full thickness | 2%–5% full thickness, high voltage, inhalation, circumferential, comorbid disease | > 5% full thickness, high voltage, inhalation, circumferential, comorbid disease |
| Disposition | Outpatient | Admission | Burn unit Burn unit Specialized hospital facilities which provide intensive care for burn patients. Staphylococcal Scalded Skin Syndrome (SSSS) |

Superficial burn
Image: “Sunburn Skin Red Flushed Dermatology Burned” by Hans Braxmeier. License: Public domain.
Superficial partial-thickness facial burns caused by the rapid passage of a fireball following a petrol explosion in a confined space
Image: “Burn injury and explosions: an Australian perspective” by Greenwood JE. License: CC BY 2.0.
Deep partial-thickness burn
Image: “Major-2nd-degree-burn” by Westchaser. License: Public domain.
Full-thickness burns
Image: “Burn injury and explosions: an Australian perspective” by Greenwood JE. License: CC BY 2.0.Burns occur due to direct contact with:
Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions has low heat Heat Inflammation conductivity, so most thermal burns only involve the epidermis Epidermis The external, nonvascular layer of the skin. It is made up, from within outward, of five layers of epithelium: (1) basal layer (stratum basale epidermidis); (2) spinous layer (stratum spinosum epidermidis); (3) granular layer (stratum granulosum epidermidis); (4) clear layer (stratum lucidum epidermidis); and (5) horny layer (stratum corneum epidermidis). Skin: Structure and Functions.
Injured areas can be subdivided into 3 zones, like a bullseye:
Superficial burn management
Superficial burn management consists of non-steroidal anti-inflammatory drugs ( NSAIDs NSAIDS Primary vs Secondary Headaches) and cold packs for pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways.
Partial-thickness burn management:
Full-thickness burn management: