The lower leg, or just “leg” in anatomical terms, is the part of the lower limb between the knee and the ankle joint Ankle joint The ankle is a hinged synovial joint formed between the articular surfaces of the distal tibia, distal fibula, and talus. The ankle primarily allows plantar flexion and dorsiflexion of the foot. . The bony structure is composed of the tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy and fibula bones, which articulate with each other at the proximal and distal tibiofibular Distal tibiofibular Ankle Joint: Anatomy joints. The muscles of the leg are grouped into the anterior, lateral, and posterior compartments by extensions of fascia Fascia Layers of connective tissue of variable thickness. The superficial fascia is found immediately below the skin; the deep fascia invests muscles, nerves, and other organs. Cellulitis and exert their action on the ankle, foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy, and toes.
Last updated: Nov 19, 2024
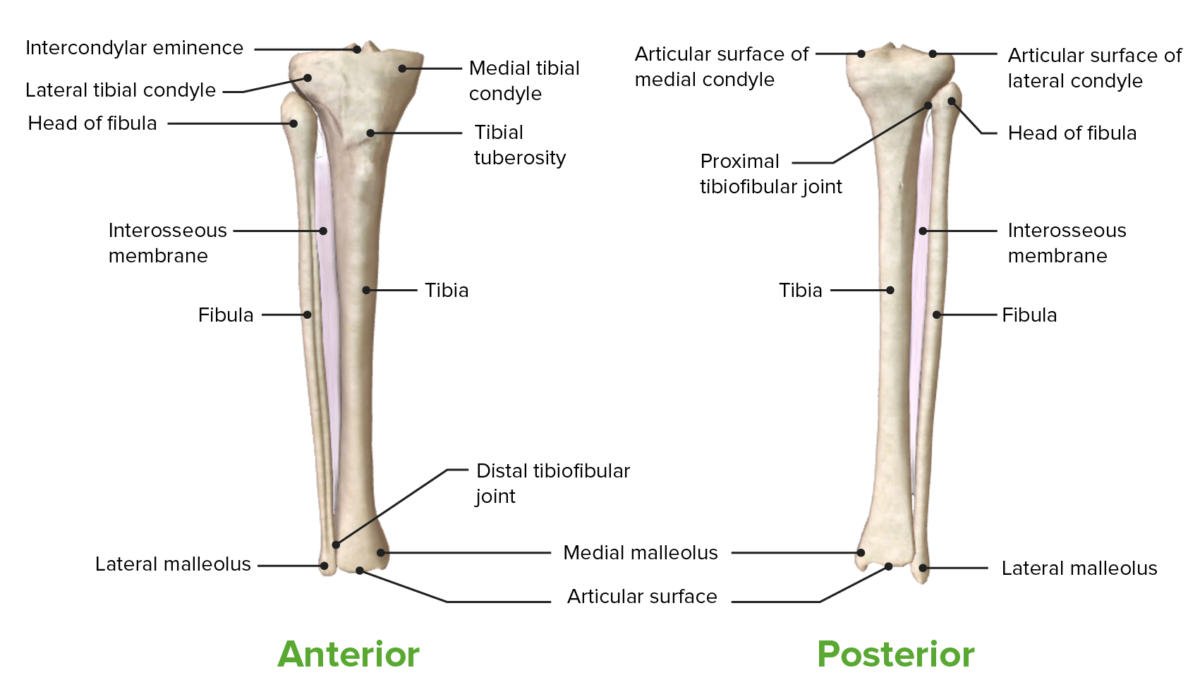
Anterior and posterior views of the tibia, fibula, and tibiofibular joints
Image by BioDigital, edited by Lecturio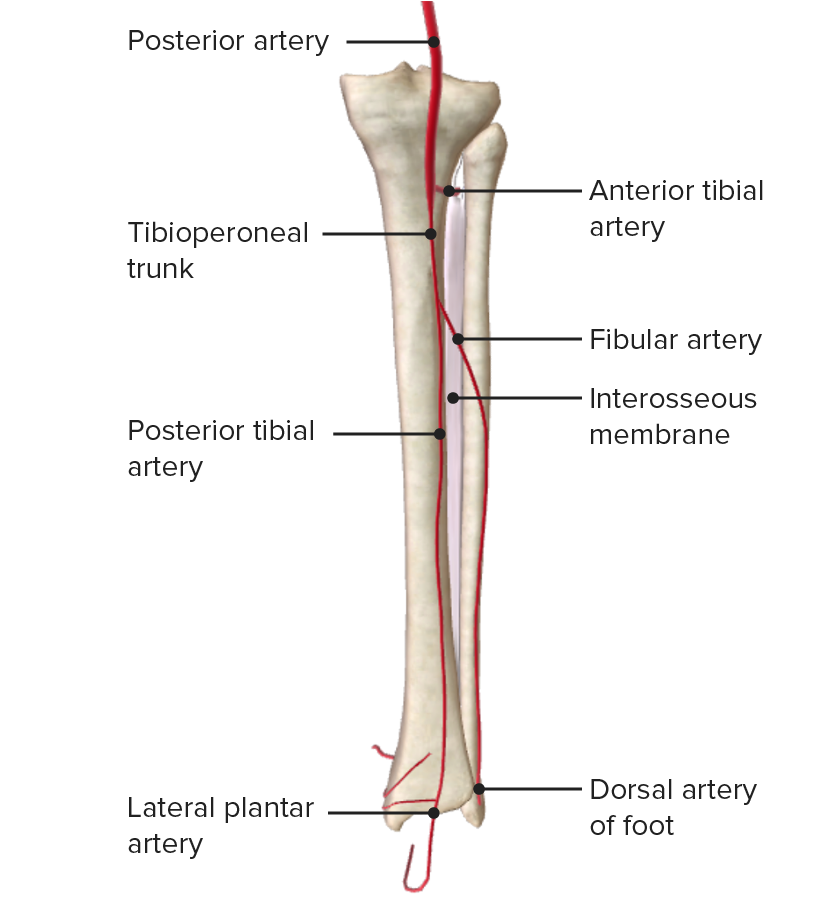
Posterior view of the leg, featuring the opening on the interosseous membrane and the passage of the anterior tibial artery
Image by BioDigital, edited by LecturioThe leg is divided into 4 fascial compartments by the interosseous membrane Interosseous Membrane A sheet of fibrous connective tissue rich in collagen often linking two parallel bony structures forming a syndesmosis type joint. It provides longitudinal stability, tensile strength, and weight distribution/transfer and may allow limited movement in syndesmoses. Forearm: Anatomy and the anterior, posterior, and transverse intermuscular septa as follows:
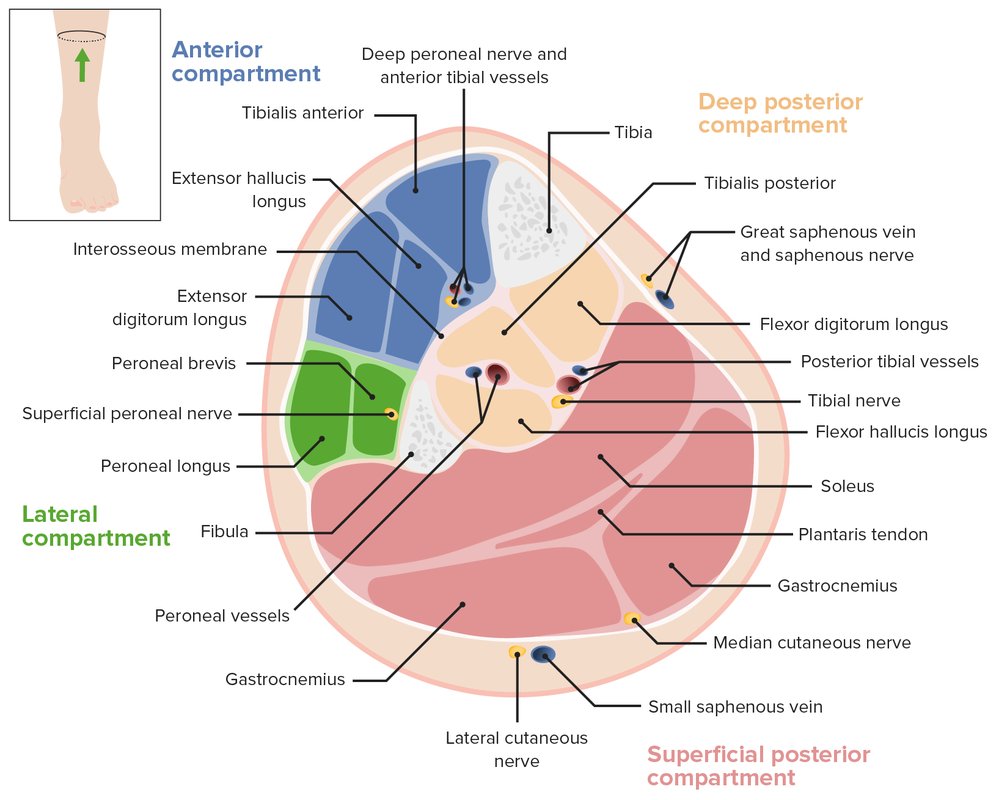
Cross section of the leg, featuring the fascial compartments and the location of the major vessels
Image by Lecturio.| Muscle | Origin | Insertion | Innervation | Function |
|---|---|---|---|---|
| Tibialis anterior | Lateral condyle, lateral surface of proximal tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy, and interosseous membrane Interosseous Membrane A sheet of fibrous connective tissue rich in collagen often linking two parallel bony structures forming a syndesmosis type joint. It provides longitudinal stability, tensile strength, and weight distribution/transfer and may allow limited movement in syndesmoses. Forearm: Anatomy (IO) | Medial cuneiform and base of 1st metatarsal | Deep fibular nerves (L4, L5, S1 S1 Heart Sounds) |
|
| Extensor digitorum Extensor digitorum Forearm: Anatomy longus | Lateral condyle of tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy, anterior surface of fibula, and IO | Middle and distal phalanges Phalanges Bones that make up the skeleton of the fingers, consisting of two for the thumb, and three for each of the other fingers. Hand: Anatomy of digits 2–5 |
|
|
| Extensor hallucis longus | Anterior surface of midfibula and IO | Distal phalanx of hallux (digit 1) |
|
|
| Fibularis tertius | Anterior surface of lower fibula and IO | Base of 5th metatarsal |
|
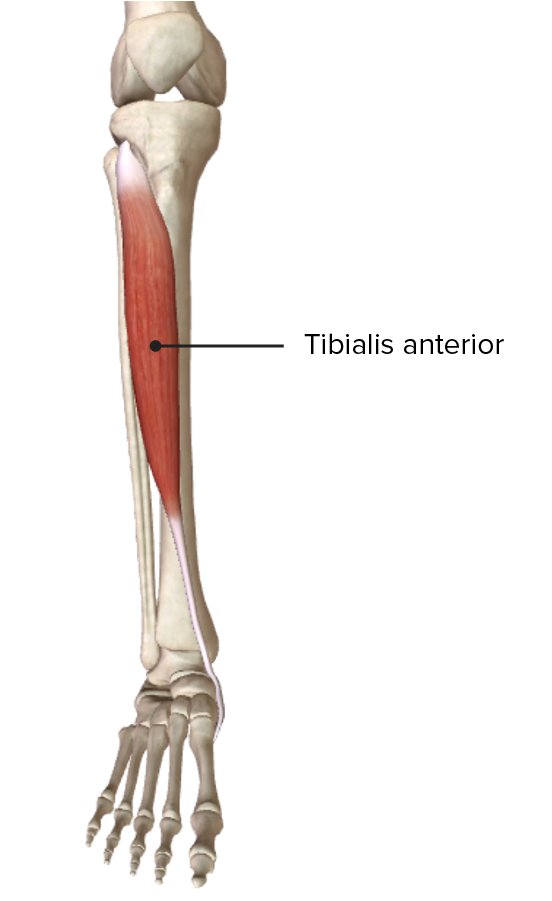
Origin and insertion of the tibialis anterior muscle in the anterior compartment of the leg
Image by BioDigital, edited by Lecturio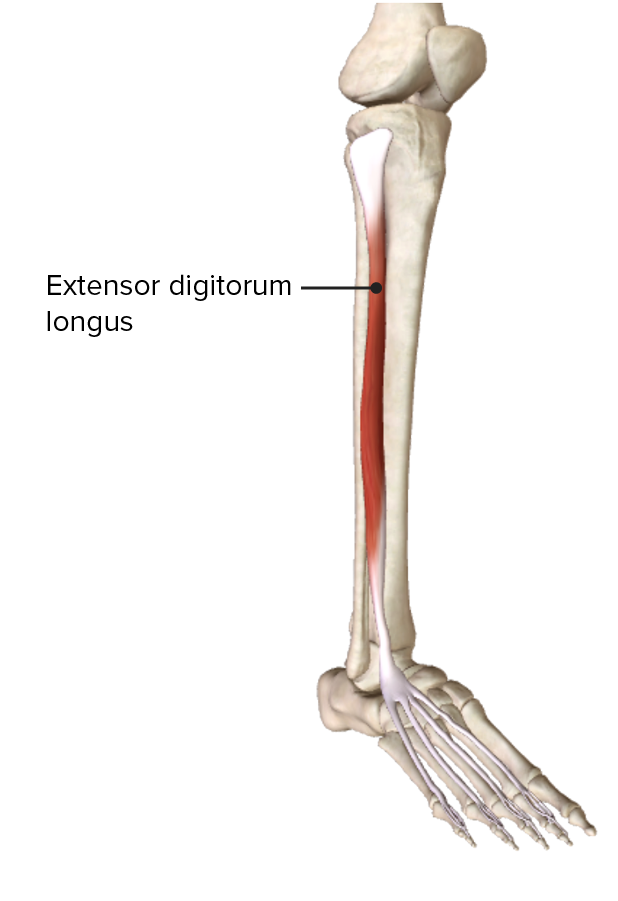
Origin and insertion of the extensor digitorum longus muscle in the anterior compartment of the leg
Image by BioDigital, edited by Lecturio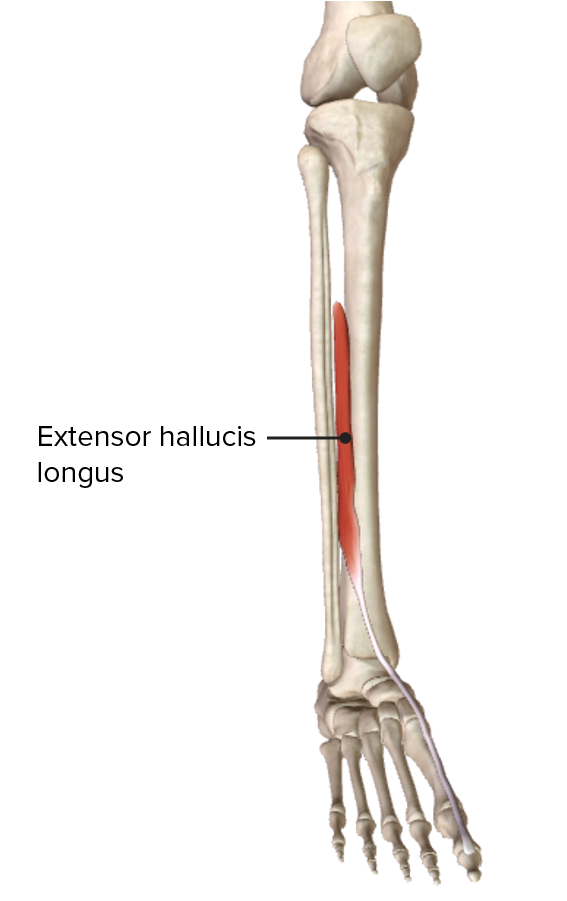
Origin and insertion of the extensor hallucis longus muscle in the anterior compartment of the leg
Image by BioDigital, edited by Lecturio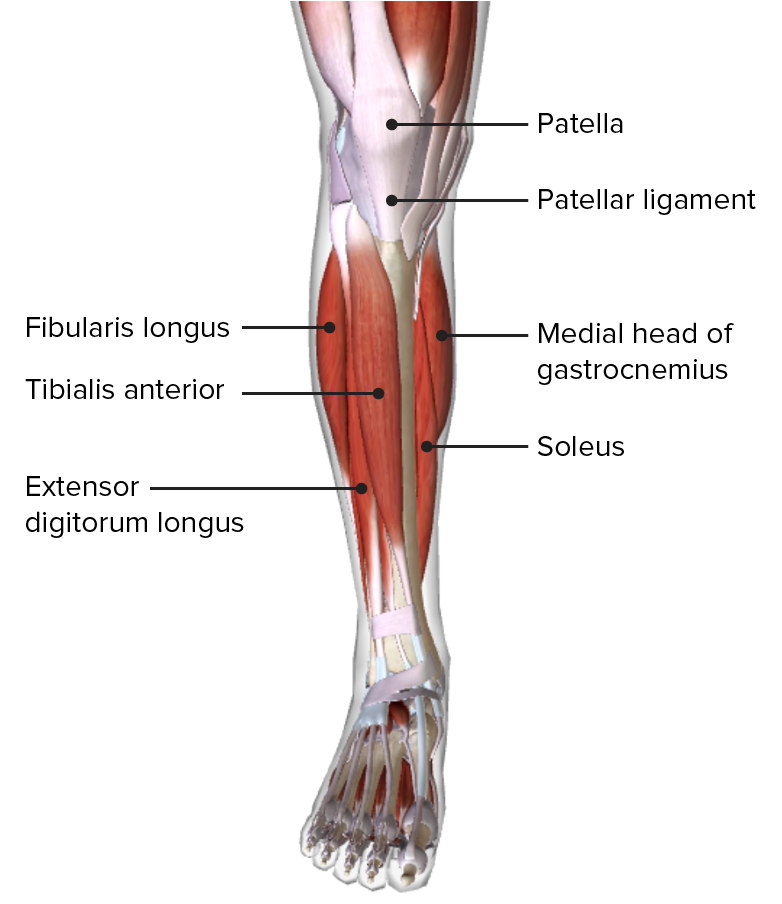
Anterior view of the leg, featuring the muscles of the anterior compartment and their relationships with other muscles and with each other
Image by BioDigital, edited by Lecturio| Muscle | Origin | Insertion | Innervation | Function |
|---|---|---|---|---|
| Fibularis longus | Head and proximal ⅔ of lateral fibula | 1st metatarsal and medial cuneiform | Superficial fibular nerves (L5, S1 S1 Heart Sounds) | |
| Fibularis brevis | Midportion of lateral fibula | Base of 5th metatarsal | Everts foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy; weak plantar flexion Flexion Examination of the Upper Limbs |
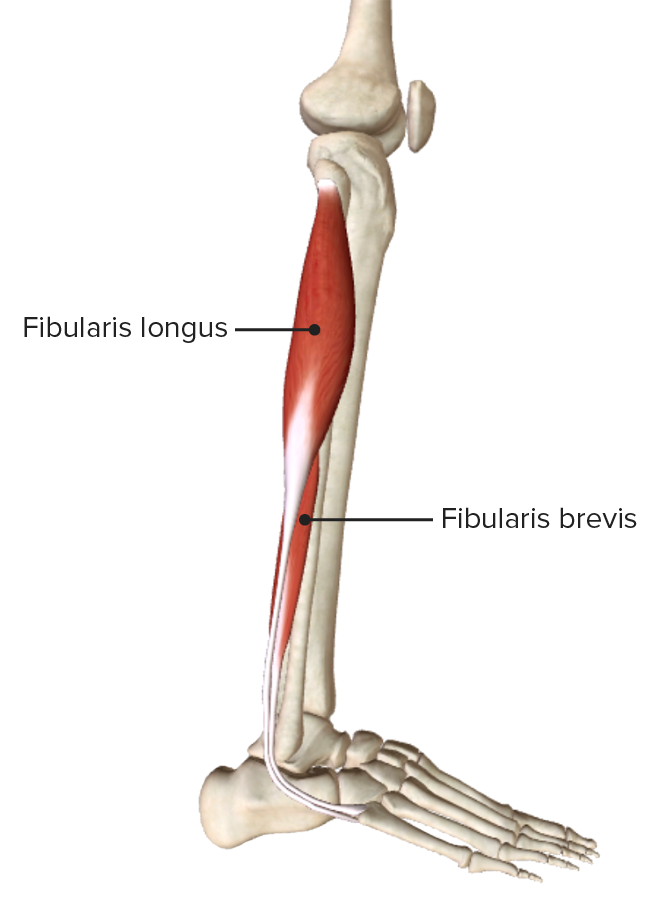
Lateral view of the leg, depicting the origin and insertion of the muscles comprising the lateral, or evertor, compartment of the leg
Image by BioDigital, edited by Lecturio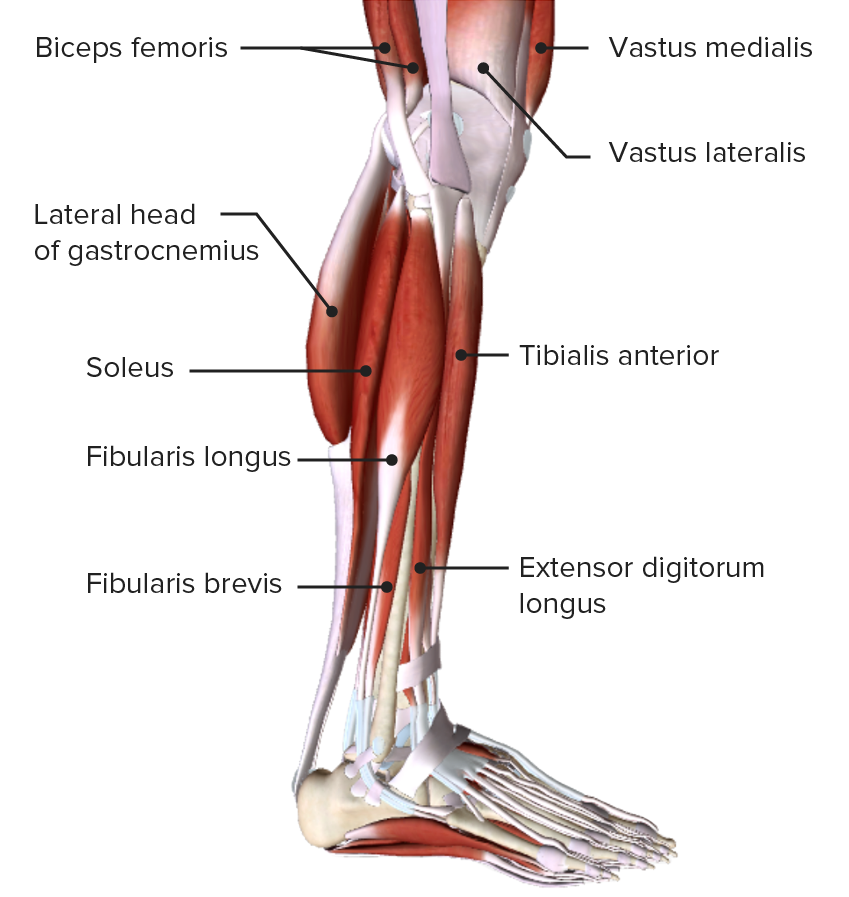
Lateral view of the leg, featuring the muscles of the lateral, or evertor, compartment and their relations with other muscles and with each other
Image by BioDigital, edited by Lecturio| Muscle | Origin | Insertion | Innervation | Function |
|---|---|---|---|---|
| Gastrocnemius |
|
Posterior aspect of calcaneus Calcaneus The largest of the tarsal bones which is situated at the lower and back part of the foot, forming the heel. Foot: Anatomy via calcaneal tendon | Tibial nerves ( S1 S1 Heart Sounds, S2 S2 Heart Sounds) |
|
| Soleus | Posterior surface of fibula and soleal line of tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy | Plantar flexes ankle | ||
| Plantaris | Inferior lateral supracondylar ridge of femur | Weak plantar flexion Flexion Examination of the Upper Limbs |
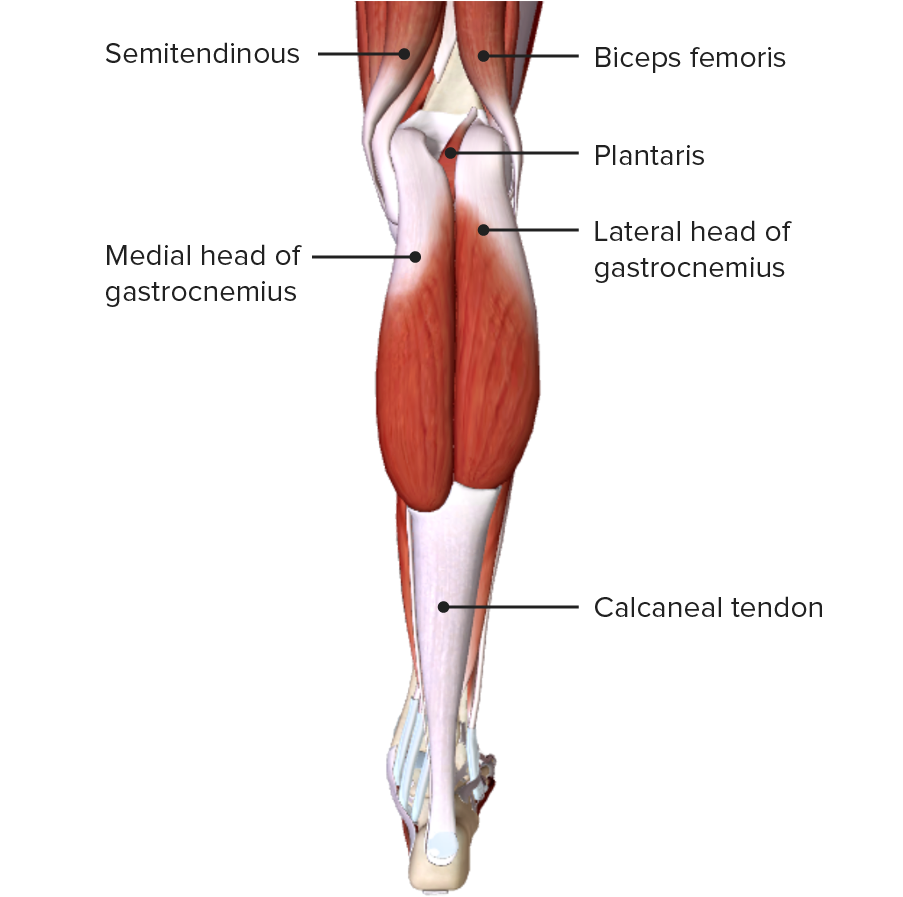
Posterior view of the leg, featuring the gastrocnemius muscles of the superficial layer of the posterior compartment
Image by BioDigital, edited by Lecturio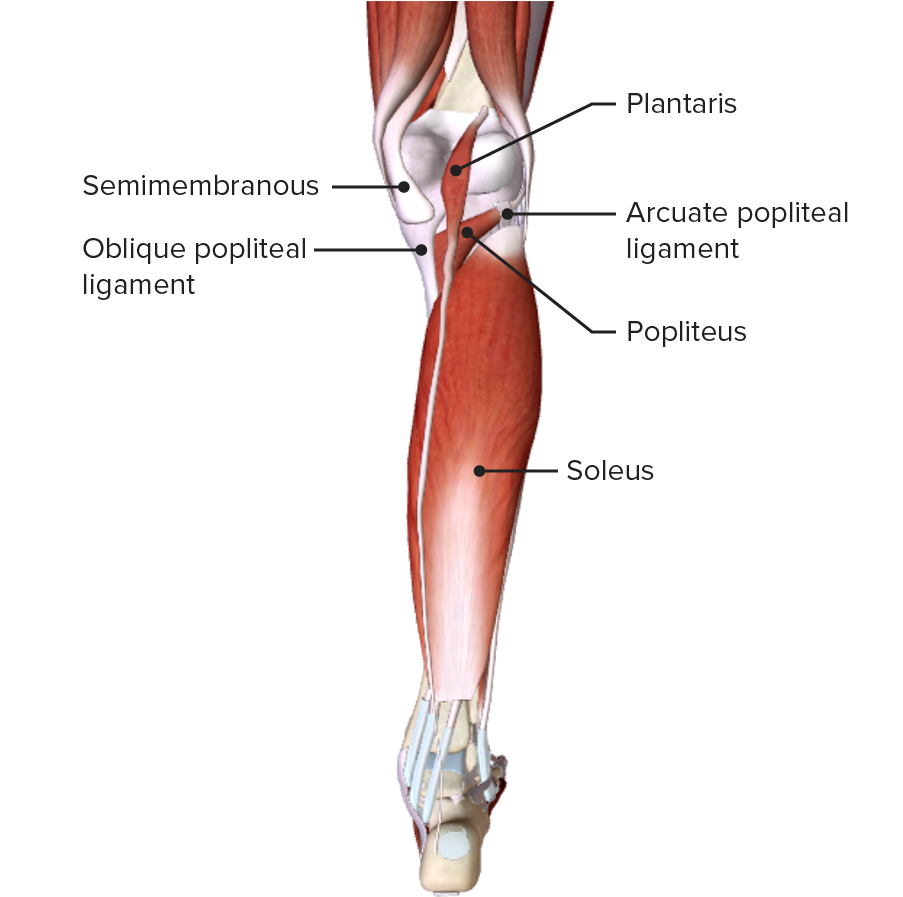
Posterior view of the leg, featuring the plantaris and soleus muscles of the superficial layer of the posterior compartment
Image by BioDigital, edited by Lecturio| Muscle | Origin | Insertion | Nerve supply | Function |
|---|---|---|---|---|
| Popliteus Popliteus Popliteal Fossa: Anatomy | Lateral aspect of lateral condyle of femur and lateral meniscus | Posterior tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy above soleal line | Tibial nerves (L4, L5, S1 S1 Heart Sounds, S2 S2 Heart Sounds, S3 S3 Heart Sounds) |
|
| Flexor digitorum longus | Posterior surface of tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy below soleal line | Distal phalanges Phalanges Bones that make up the skeleton of the fingers, consisting of two for the thumb, and three for each of the other fingers. Hand: Anatomy of digits 2–5 |
|
|
| Flexor hallucis longus | Lower ⅔ of posterior fibula and interosseous membrane Interosseous Membrane A sheet of fibrous connective tissue rich in collagen often linking two parallel bony structures forming a syndesmosis type joint. It provides longitudinal stability, tensile strength, and weight distribution/transfer and may allow limited movement in syndesmoses. Forearm: Anatomy | Distal phalanx of hallux |
|
|
| Tibialis posterior | Interosseous membrane Interosseous Membrane A sheet of fibrous connective tissue rich in collagen often linking two parallel bony structures forming a syndesmosis type joint. It provides longitudinal stability, tensile strength, and weight distribution/transfer and may allow limited movement in syndesmoses. Forearm: Anatomy and posterior borders of tibia Tibia The second longest bone of the skeleton. It is located on the medial side of the lower leg, articulating with the fibula laterally, the talus distally, and the femur proximally. Knee Joint: Anatomy and fibula | Tuberosity of the navicular Navicular Foot: Anatomy bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, 1st–3rd cuneiform bones, and 2nd–4th metatarsal bones Metatarsal Bones The five long bones of the metatarsus, articulating with the tarsal bones proximally and the phalanges of toes distally. Foot: Anatomy |
|
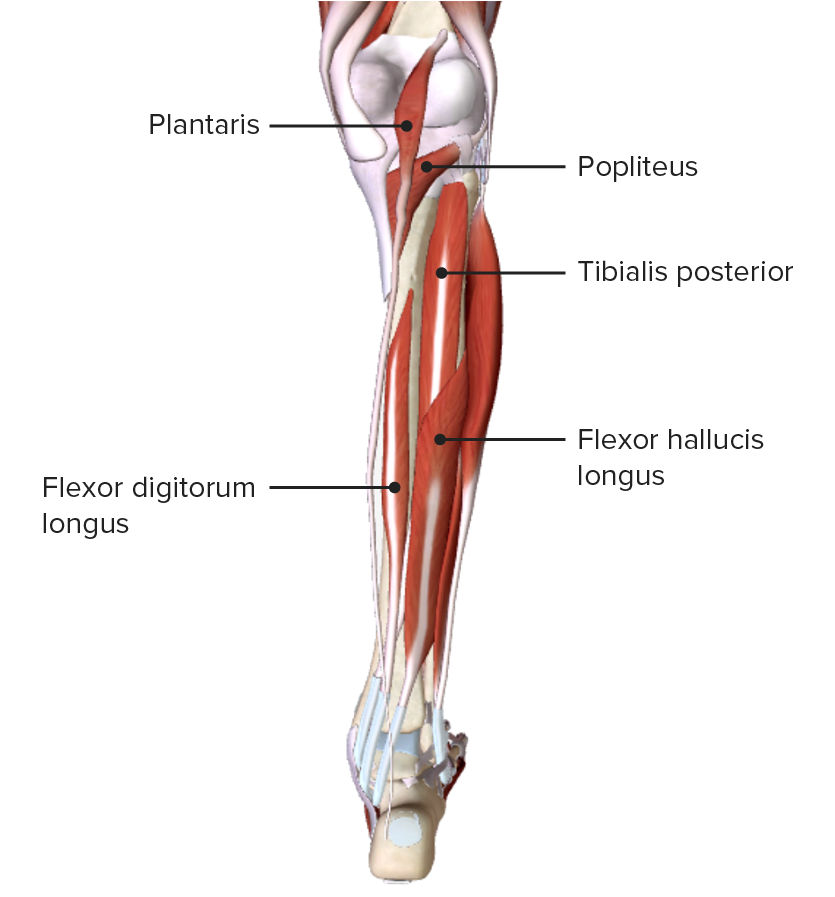
Posterior view of the leg, featuring the muscles of the deep layer of the posterior compartment and their spatial relationships with other muscles and with each other
Image by BioDigital, edited by Lecturio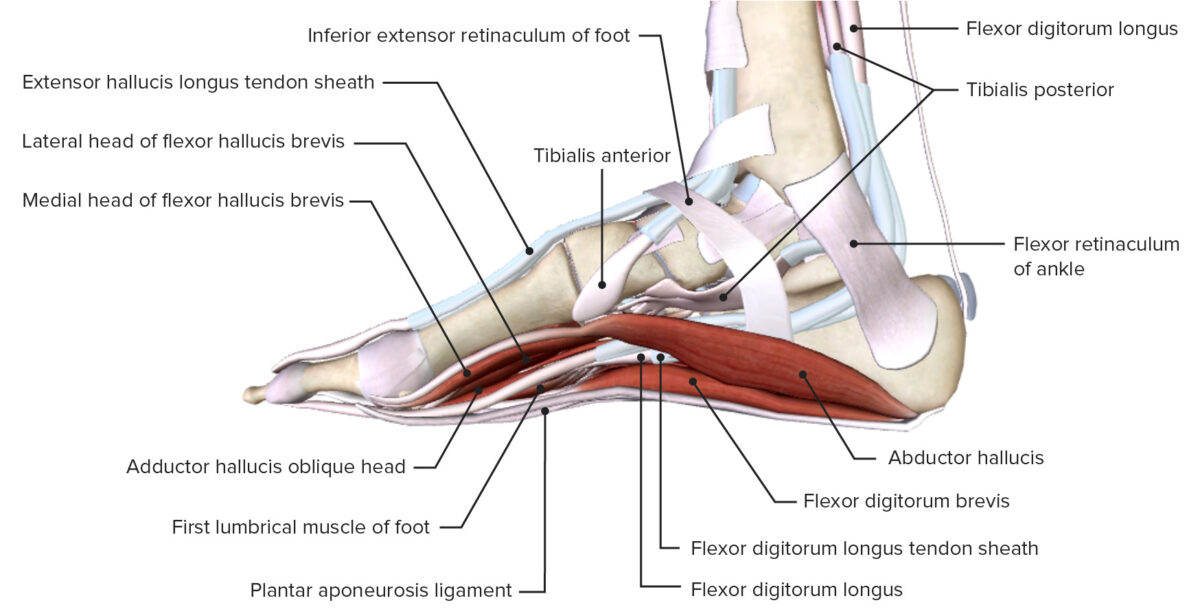
Medial view of ankle joint, featuring the retinacula of the ankle and the insertions of the muscles of the leg
Image by BioDigital, edited by LecturioA continuation of the popliteal artery Popliteal Artery The continuation of the femoral artery coursing through the popliteal fossa; it divides into the anterior and posterior tibial arteries. Popliteal Fossa: Anatomy supplies blood to the lower leg. The artery bifurcates at the lower margin of the popliteal fossa Popliteal fossa The popliteal fossa or the “knee pit” is a diamond-shaped, fat-filled, shallow depression on the posterior aspect of the knee joint. The popliteal fossa is located at the dorsal aspect of the knee and contains an increased number of lymph nodes as well as structures of the neurovascular system that travel from the thigh to the lower leg. Popliteal Fossa: Anatomy and sends branches to the anterior compartment, the anterior tibial artery, and the posterior and lateral compartments, forming the tibioperoneal trunk.
| Origin | Trajectory | Branches | Supply | |
|---|---|---|---|---|
| Anterior tibial artery (accompanied by the deep peroneal nerve Deep peroneal nerve Foot: Anatomy) | Division of popliteal artery Popliteal Artery The continuation of the femoral artery coursing through the popliteal fossa; it divides into the anterior and posterior tibial arteries. Popliteal Fossa: Anatomy into anterior tibial artery and tibiofibular trunk |
|
|
Anterior compartment of leg |
| Posterior tibial artery (accompanied by tibial nerve Tibial Nerve The medial terminal branch of the sciatic nerve. The tibial nerve fibers originate in lumbar and sacral spinal segments (L4 to S2). They supply motor and sensory innervation to parts of the calf and foot. Popliteal Fossa: Anatomy) | Terminal branch of tibioperoneal trunk |
|
|
|
| Peroneal artery Peroneal Artery Ankle Joint: Anatomy | Terminal branch of tibioperoneal trunk |
|
Muscular branches | Lateral compartment and deep layer of posterior compartment of leg |
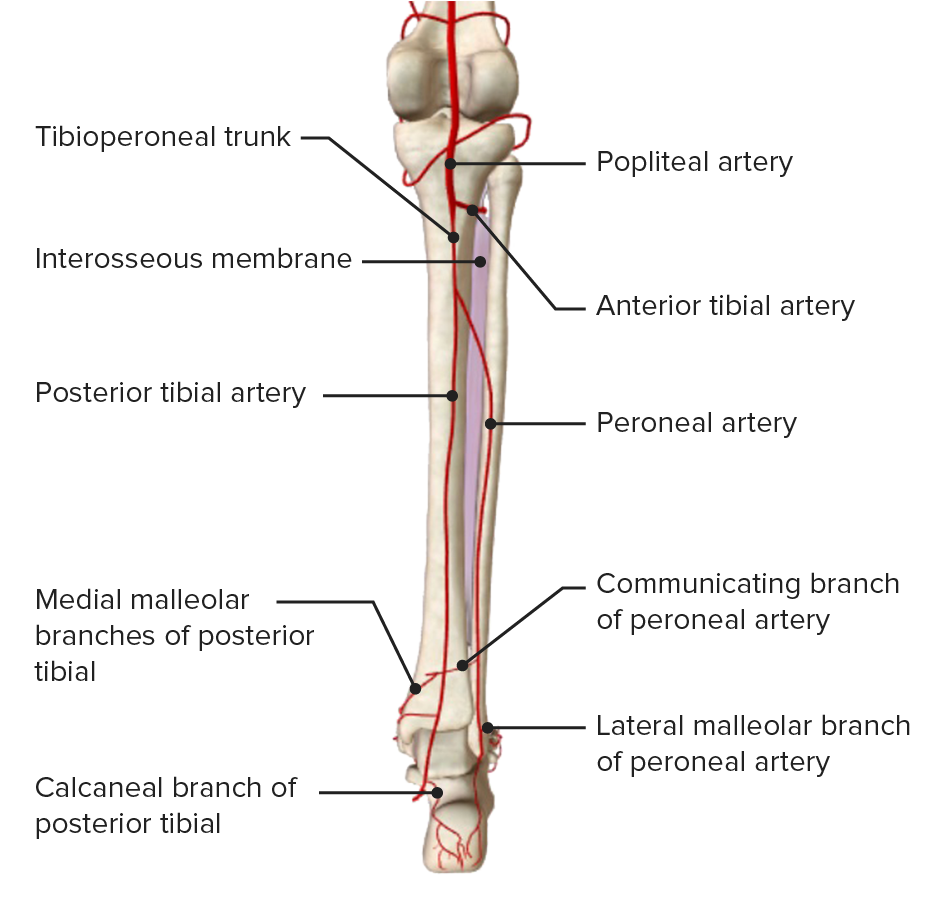
Posterior view of the leg, featuring the arterial blood supply derived from the popliteal artery and its branches
Image by BioDigital, edited by Lecturio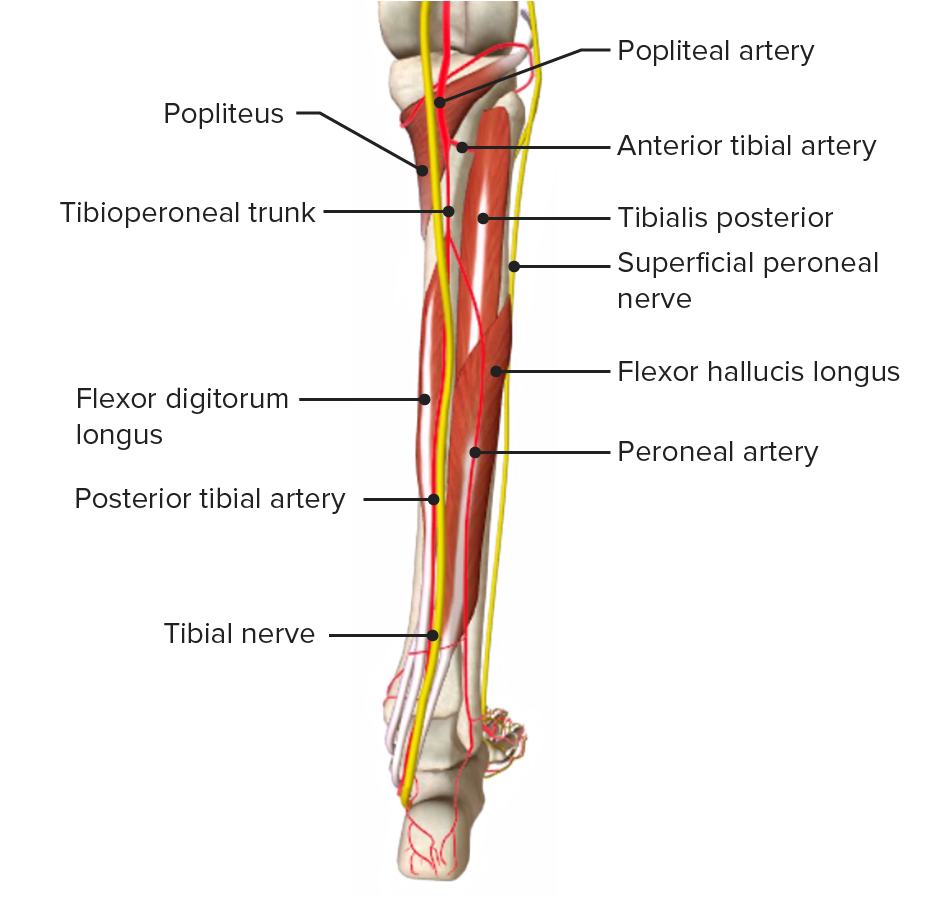
Posterior view of the leg, featuring the arterial blood supply and accompanying nerves
Image by BioDigital, edited by Lecturio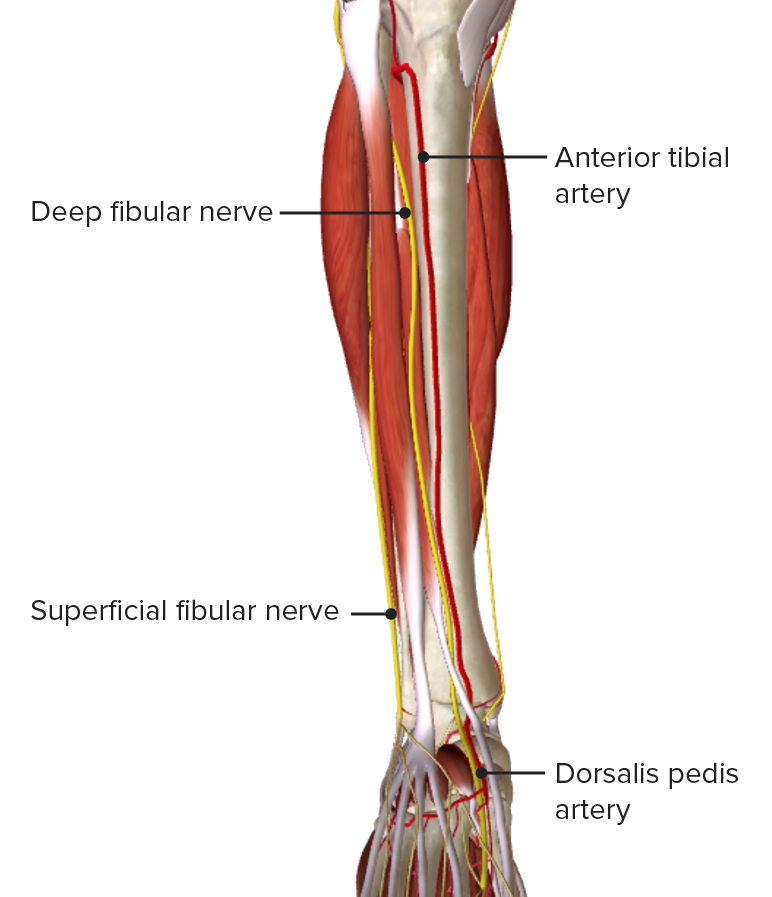
Anterior view of the leg, featuring the blood supply of the anterior compartment
Image by BioDigital, edited by LecturioThere are 2 venous drainage networks in the leg:
| Origin | Trajectory | Tributaries | Drainage | |
|---|---|---|---|---|
| Great saphenous vein (accompanied by saphenous nerve Saphenous nerve Foot: Anatomy) | Continuation of medial end of dorsal venous arch Dorsal venous arch Foot: Anatomy of the foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy |
|
|
Anteromedial aspect of leg and plantar aspect of foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy |
| Small saphenous vein (accompanied by sural nerve) | Continuation of lateral end of dorsal venous arch Dorsal venous arch Foot: Anatomy of foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy |
|
Posterior aspect of leg |
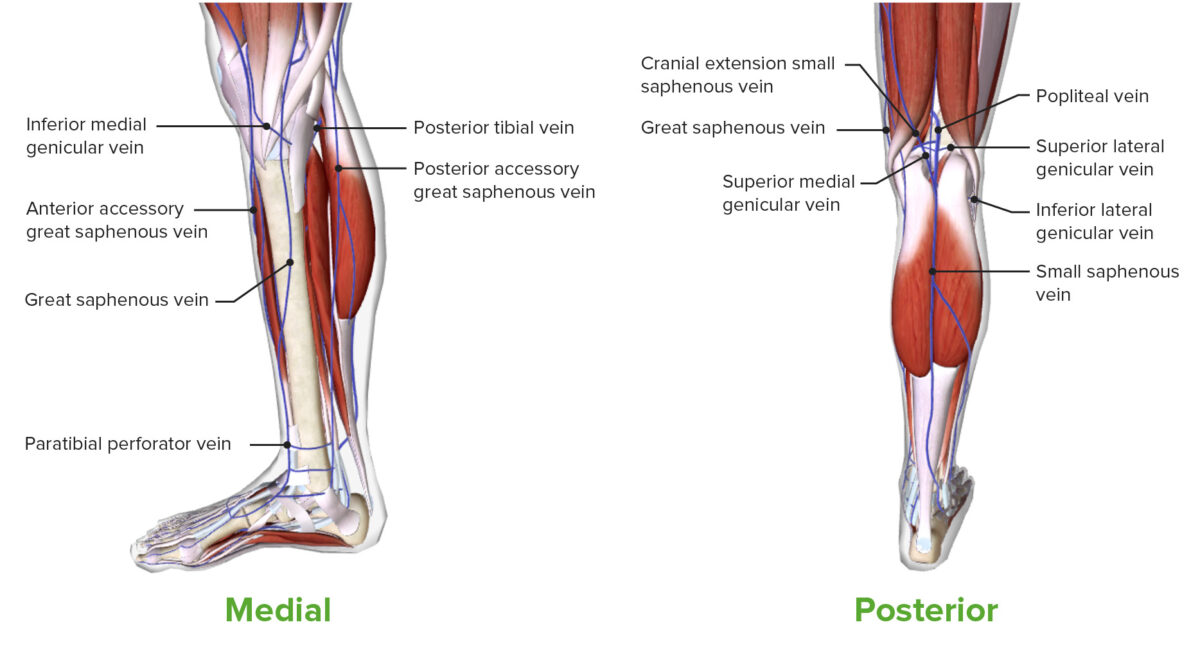
Medial and posterior views of the leg, featuring the superficial venous drainage
Image by BioDigital, edited by LecturioDeep veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology of the leg:
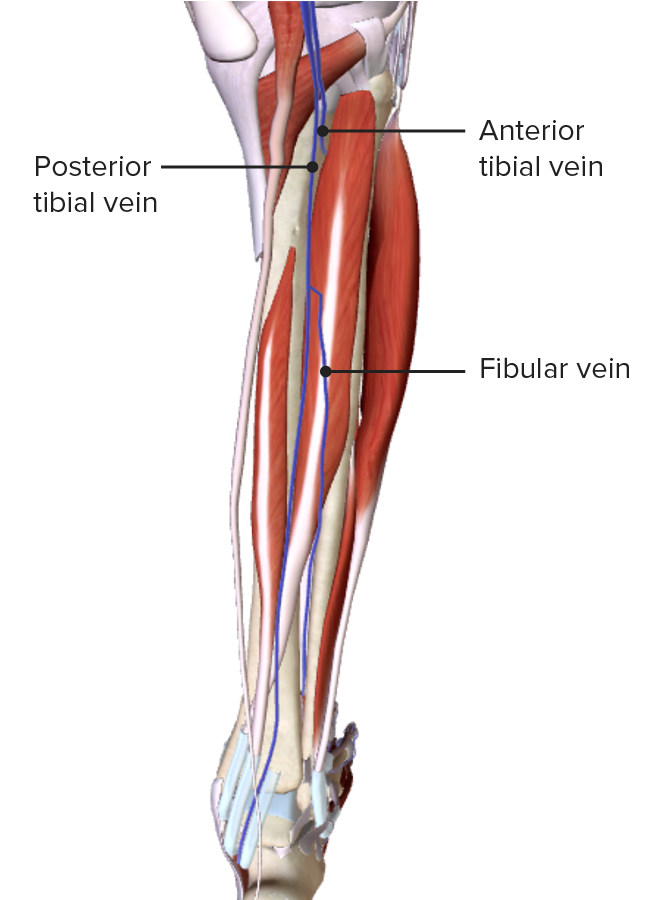
Posterior view of the leg, featuring the deep venous drainage
Image by BioDigital, edited by LecturioThe sensory Sensory Neurons which conduct nerve impulses to the central nervous system. Nervous System: Histology and motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology innervation to the lower limb is supplied by the lumbosacral plexus (L1– S4 S4 Heart Sounds).
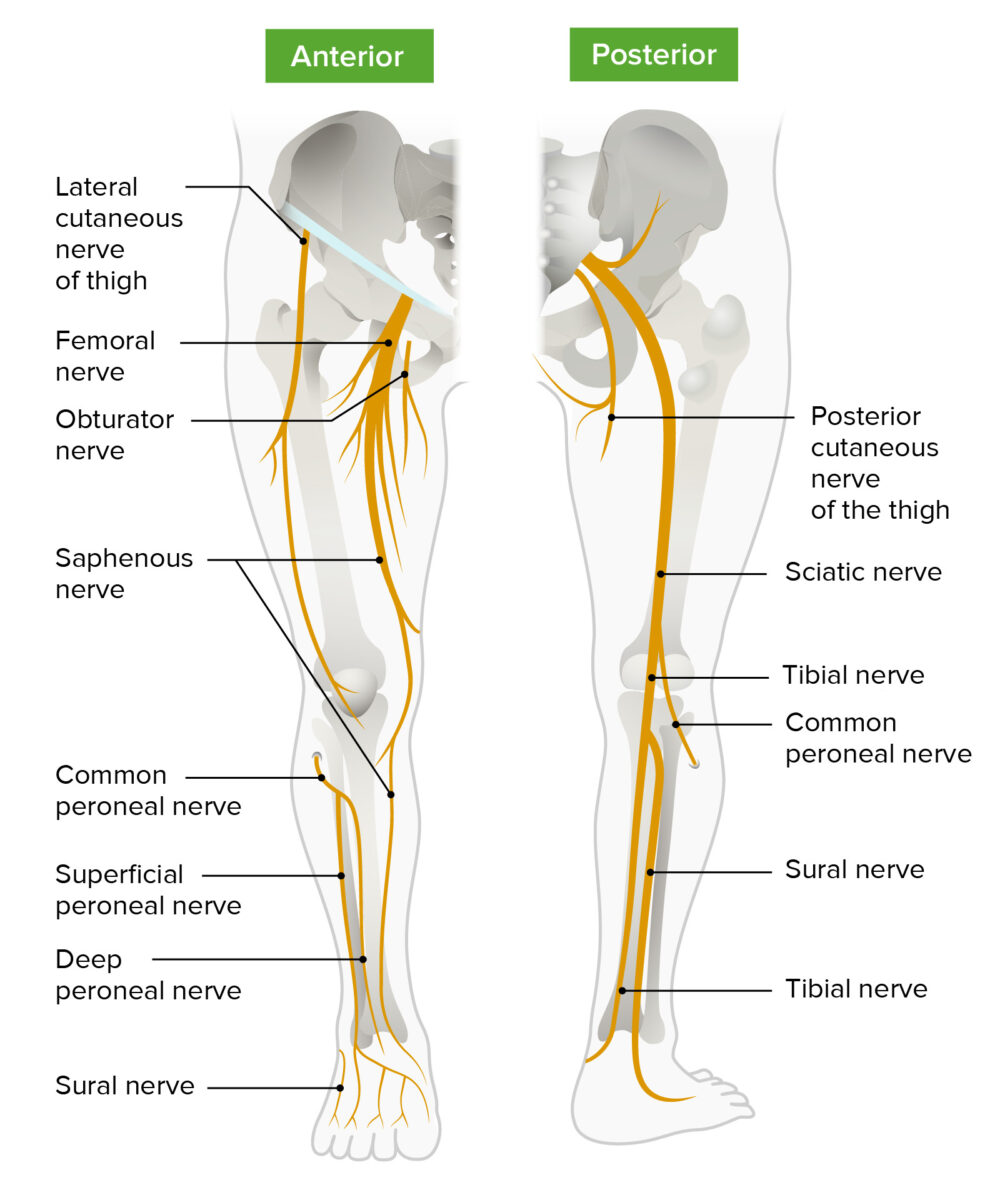
Schematic diagram of the course and main branches of the lumbosacral plexus that innervate the lower limbs
Image by Lecturio.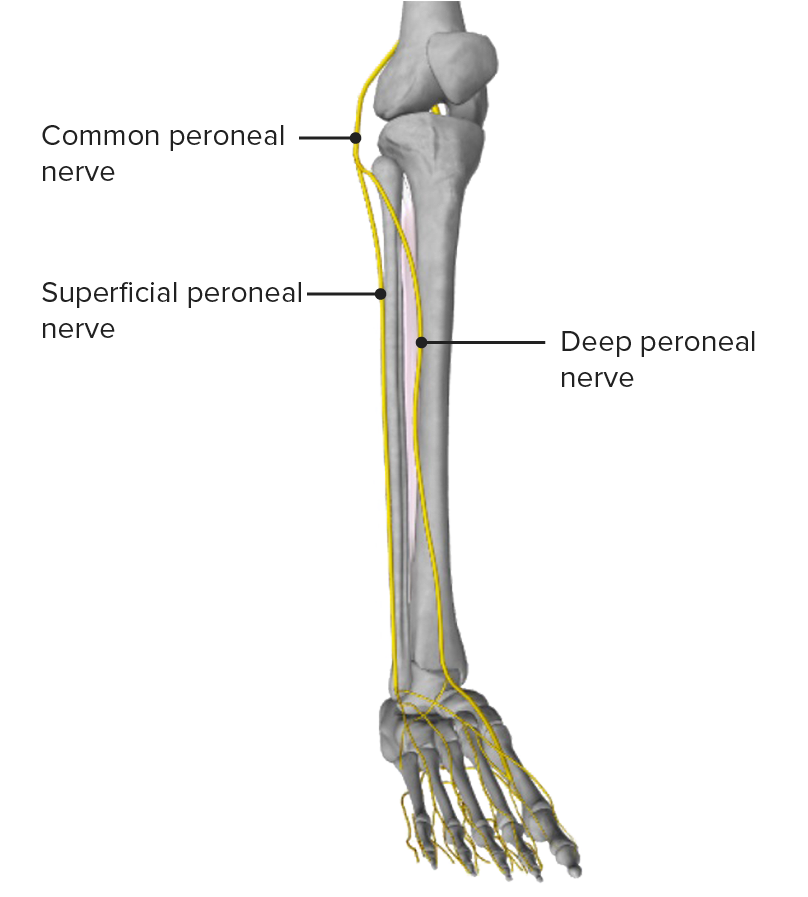
Anterior view of the leg, featuring the common peroneal nerve and its main branches
Image by BioDigital, edited by Lecturio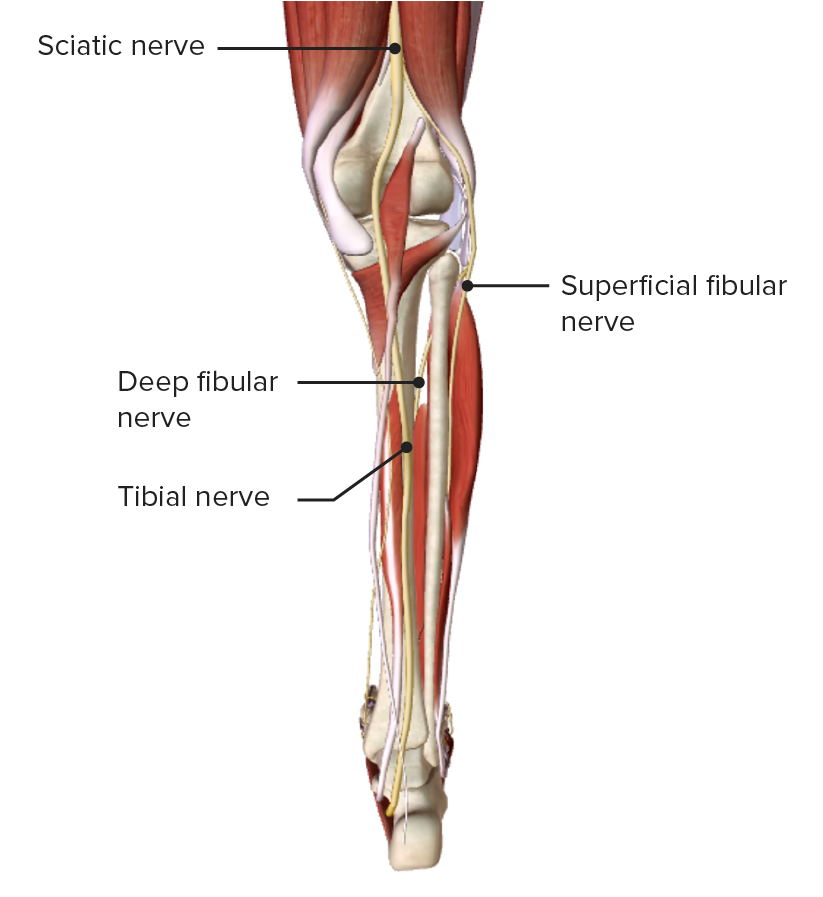
Posterior view of the leg, featuring the tibial nerve as it passes through the medial aspect of the popliteal fossa
Image by BioDigital, edited by Lecturio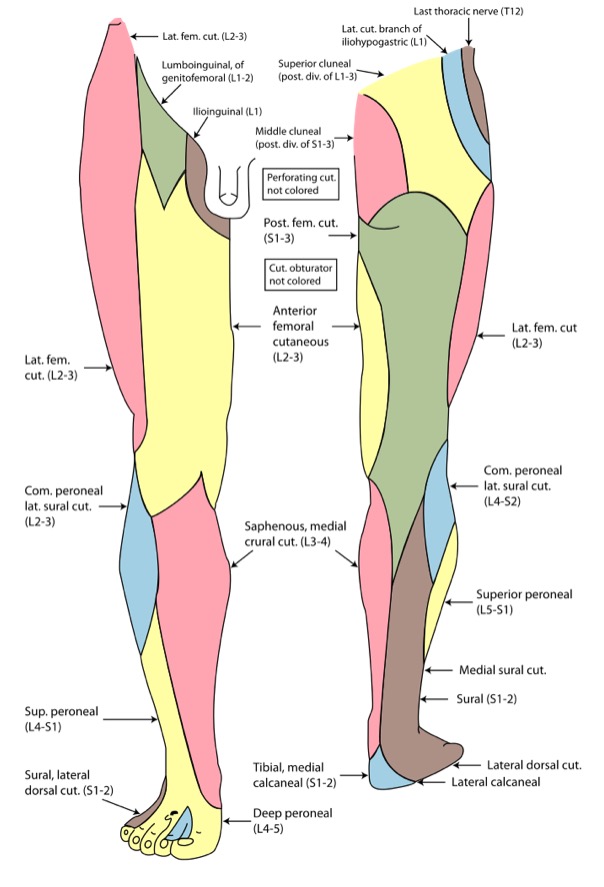
Cutaneous innervation of the lower limb
Image: “Gray826and831” by Henry Vandyke Carter. License: Public DomainThe following are common conditions associated with the lower leg: