Advertisement
Advertisement
Advertisement
Advertisement
Ankle and foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways accounts for up to 20% of cases of musculoskeletal complaints in outpatient clinics. The most common etiologies of foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy and ankle pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be categorized into arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, trauma, sprains, and systemic causes. The diagnosis is clinical with imaging and/or laboratory studies to confirm the suspected diagnosis. Management involves rest, ice packs, compression Compression Blunt Chest Trauma, elevation, and nonsteroidal anti-inflammatory drugs ( NSAIDs NSAIDS Primary vs Secondary Headaches). Surgical repair is rarely needed.
Last updated: Nov 21, 2022
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Epidemiology
Foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways is more common among people who wear uncomfortable shoes (usually women).
Classification
History
Physical examination
Ottawa ankle and foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy rules:
The etiology of ankle or foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways can be determined from the anatomical location of the maximum point of pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways or tenderness.
| Location | Condition | Features |
|---|---|---|
| Lateral aspect | Ankle sprain ( acute pain Acute pain Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, with well-defined location, character, and timing. Pain Management) |
|
| Medial aspect |
|
|
| Posterior aspect | Achilles tendinitis Tendinitis Ankylosing Spondylitis ( acute pain Acute pain Intensely discomforting, distressful, or agonizing sensation associated with trauma or disease, with well-defined location, character, and timing. Pain Management) |
|
| Variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables locations | Infectious and inflammatory conditions |
|
| Location | Condition | Features |
|---|---|---|
| Forefoot (toes + distal metatarsals) | Bunions (hallux valgus) |
|
| Ingrown toenails |
|
|
| Morton neuroma |
|
|
| Corns and calluses |
|
|
| Plantar warts Warts Benign epidermal proliferations or tumors; some are viral in origin. Female Genitourinary Examination |
|
|
| Metatarsal stress fractures Stress Fractures Fractures due to the strain caused by repetitive exercise. They are thought to arise from a combination of muscle fatigue and bone failure, and occur in situations where bone remodeling predominates over repair. The most common sites of stress fractures are the metatarsus, fibula, tibia, and femoral neck. Chronic Apophyseal Injury |
|
|
| Midfoot ( tarsal bones Tarsal Bones The seven bones which form the tarsus – namely, calcaneus; talus; cuboid, navicular, and the internal, middle, and external cuneiforms. Foot: Anatomy, arches, and ligaments) | Osteoarthritis Osteoarthritis Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis |
|
| High-arched feet ( pes PES Removal of plasma and replacement with various fluids, e.g., fresh frozen plasma, plasma protein fractions (ppf), albumin preparations, dextran solutions, saline. Used in treatment of autoimmune diseases, immune complex diseases, diseases of excess plasma factors, and other conditions. Thrombotic Thrombocytopenic Purpura cavus) and flat feet ( pes planus Pes Planus Ehlers-Danlos Syndrome) |
|
|
| Navicular Navicular Foot: Anatomy stress fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures |
|
|
| Hindfoot ( talus Talus The second largest of the tarsal bones. It articulates with the tibia and fibula to form the ankle joint. Ankle Joint: Anatomy + calcaneus Calcaneus The largest of the tarsal bones which is situated at the lower and back part of the foot, forming the heel. Foot: Anatomy) | Plantar fasciitis |
|
| Tarsal tunnel syndrome |
|
|
| Calcaneal and talar stress fractures Stress Fractures Fractures due to the strain caused by repetitive exercise. They are thought to arise from a combination of muscle fatigue and bone failure, and occur in situations where bone remodeling predominates over repair. The most common sites of stress fractures are the metatarsus, fibula, tibia, and femoral neck. Chronic Apophyseal Injury |
|
|
| Calcaneal apophysitis Apophysitis Osgood-Schlatter Disease (Sever’s disease) |
|
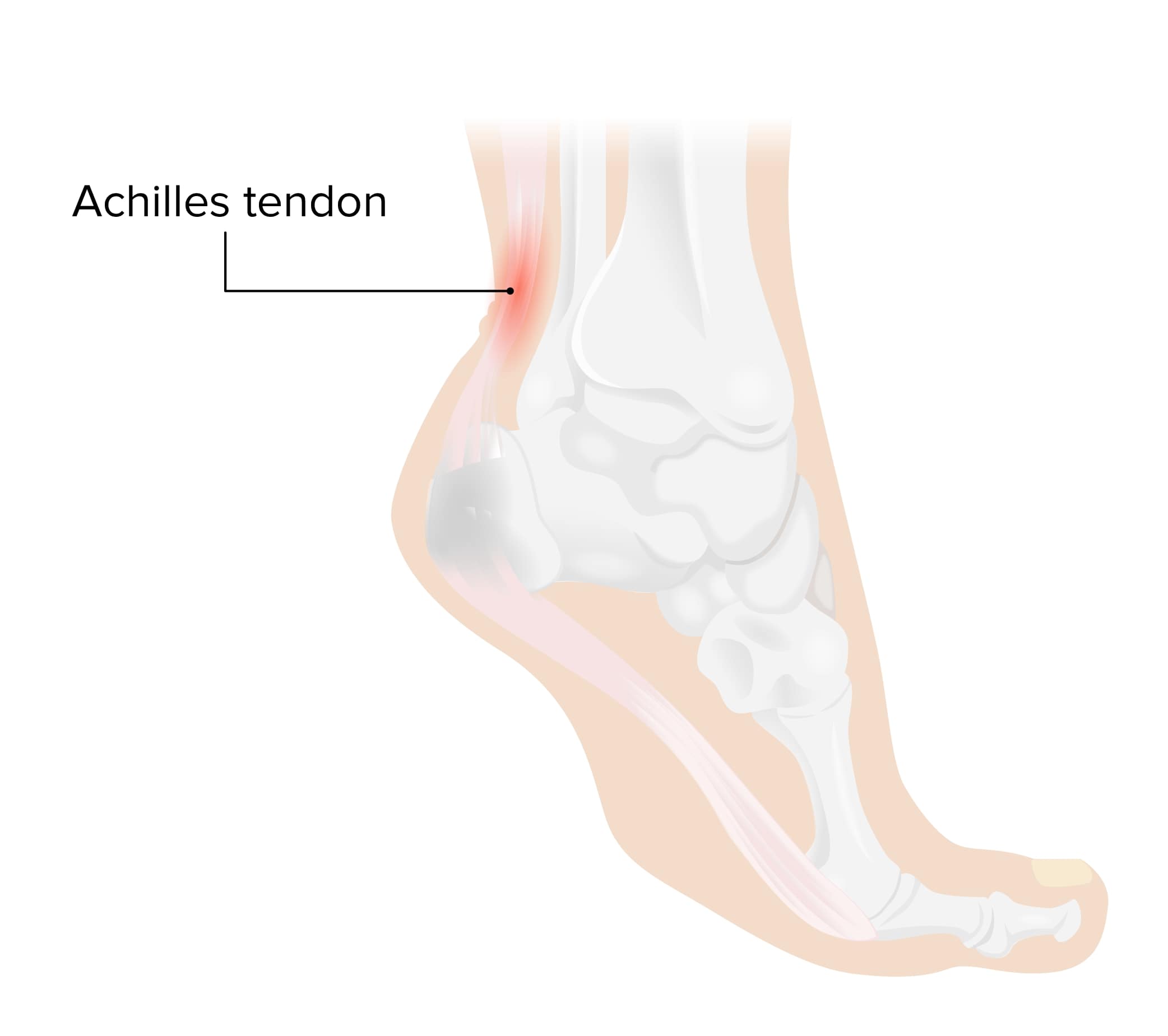
Achilles tendinitis:
The Achilles tendon is in the back of the ankle, connecting the calf muscles to the heel bone. This tendon is needed for walking, running, and jumping and withstands a great deal of stress during normal daily life. Achilles tendinitis occurs when the muscles and tendon are overused, causing irritation and swelling of the tendon.

Erythema and swelling of the 1st metatarsophalangeal joint consistent with acute gout
Image: “Podagra” by Gonzosft. License: CC BY 3.0 DE
Hallux valgus deformity:
The common and painful deformity occurs with lateral deviation of the hallux (the 1st digit) on the 1st metatarsal. Hallux valgus can also be associated with eversion of the toe.

Ingrown toenail of the 1st digit:
Ingrown toenails develop when part of the lateral nail plate pierces the lateral nail fold and skin, causing an inflammatory reaction.
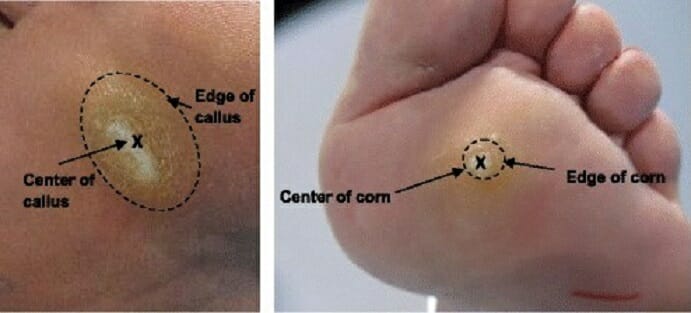
Landmarks of a callus (left) and a corn (right):
Calluses and corns are some of the most common skin lesions of the feet and potential sources of foot pain.

Plantar wart on the bottom of a big toe
Image: “Plantar wart on the bottom of the big toe (mine)” by Dewdude. License: CC BY 2.5
Pes planus (flatfoot)
Image: “Pes planus typically seen in Alström syndrome” by Marshall J.D. et al. License: CC BY 2.5, edited by Lecturio.Diagnostic workup:

Radiographs demonstrating a stress fracture of the 5th metatarsal (arrows):
a: anteroposterior (AP) view
b: oblique view

X-ray of a foot with pes cavus (high arch of the foot)
Image: “Pes cavus and os peroneum on lateral foot X-ray” by Mikael Häggström. License: CC0 1.0
X-ray of the foot of an 11-year-old boy, showing sclerosis and fragmentation of the calcaneal apophysis. However, X-rays have poor sensitivity and specificity for Sever’s disease so diagnosis is usually made clinically.
Image: “Sclerosis and fragmentation of the calcaneal apophysis” by Mikael Häggström. License: CC0 1.0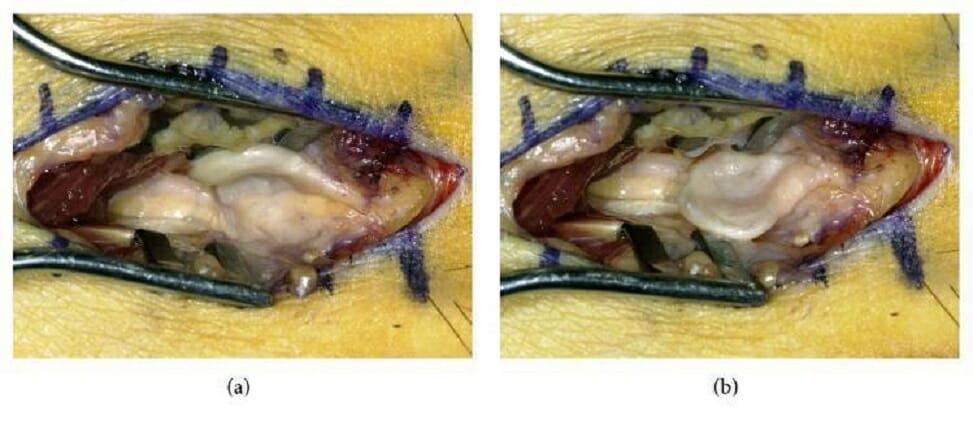
Intraoperative photographs showing a Morton neuroma (an interdigital neuroma of the foot):
(a): Dorsally deviated course of the interdigital nerve and neuroma
(b): Transversely reclined neuroma showing the impression in its center (assumedly made by the adjacent metatarsal heads)
The following are common conditions associated with ankle and foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways: