Surgical site infection Surgical site infection Infection occurring at the site of a surgical incision. Surgical Complications (SSI) is a type of surgical infection Surgical infection An infection is the proliferation of microorganisms within tissues, body cavities, or spaces, which induces an immune response and overwhelms the body's natural defenses. In surgical patients, these infections are frequently caused by the translocation of commensal organisms into deeper tissues, combined with the impairment of host defenses due to surgical injury or stress. Surgical Infections that occurs at or near a surgical incision within 30 days of the procedure or within 90 days if prosthetic material is implanted. Surgical site infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are classified according to the depth of involvement as superficial, deep, or organ/space. Diagnosis relies on clinical findings and may require diagnostic imaging. Management involves antibiotics as well as surgical drainage/ debridement Debridement The removal of foreign material and devitalized or contaminated tissue from or adjacent to a traumatic or infected lesion until surrounding healthy tissue is exposed. Stevens-Johnson Syndrome as necessary.
Last updated: Feb 21, 2023
Surgical site infection Surgical site infection Infection occurring at the site of a surgical incision. Surgical Complications (SSI) is an infection that occurs at or near a surgical incision or deep to it within 30 days of the procedure or within 90 days if prosthetic material is implanted.
Surgical wounds are classified from clean to dirty on the basis of the increasing risk of infection.
| Class | Description |
|---|---|
| Clean |
|
| Clean-contaminated |
|
| Contaminated |
|
| Dirty |
|
Contamination of surgical wounds occurs to some degree in all surgical procedures. However, in most cases, the infecting agents do not overcome host defenses. For SSI to occur, the bacterial colonization Colonization Bacteriology must trigger Trigger The type of signal that initiates the inspiratory phase by the ventilator Invasive Mechanical Ventilation an immune response.
Procedural factors:
Patient factors:
When the virulence factors Virulence factors Those components of an organism that determine its capacity to cause disease but are not required for its viability per se. Two classes have been characterized: toxins, biological and surface adhesion molecules that affect the ability of the microorganism to invade and colonize a host. Haemophilus of a microorganism are sufficient to overcome the innate and adaptive immune responses, a clinically important infection occurs in the following manner:
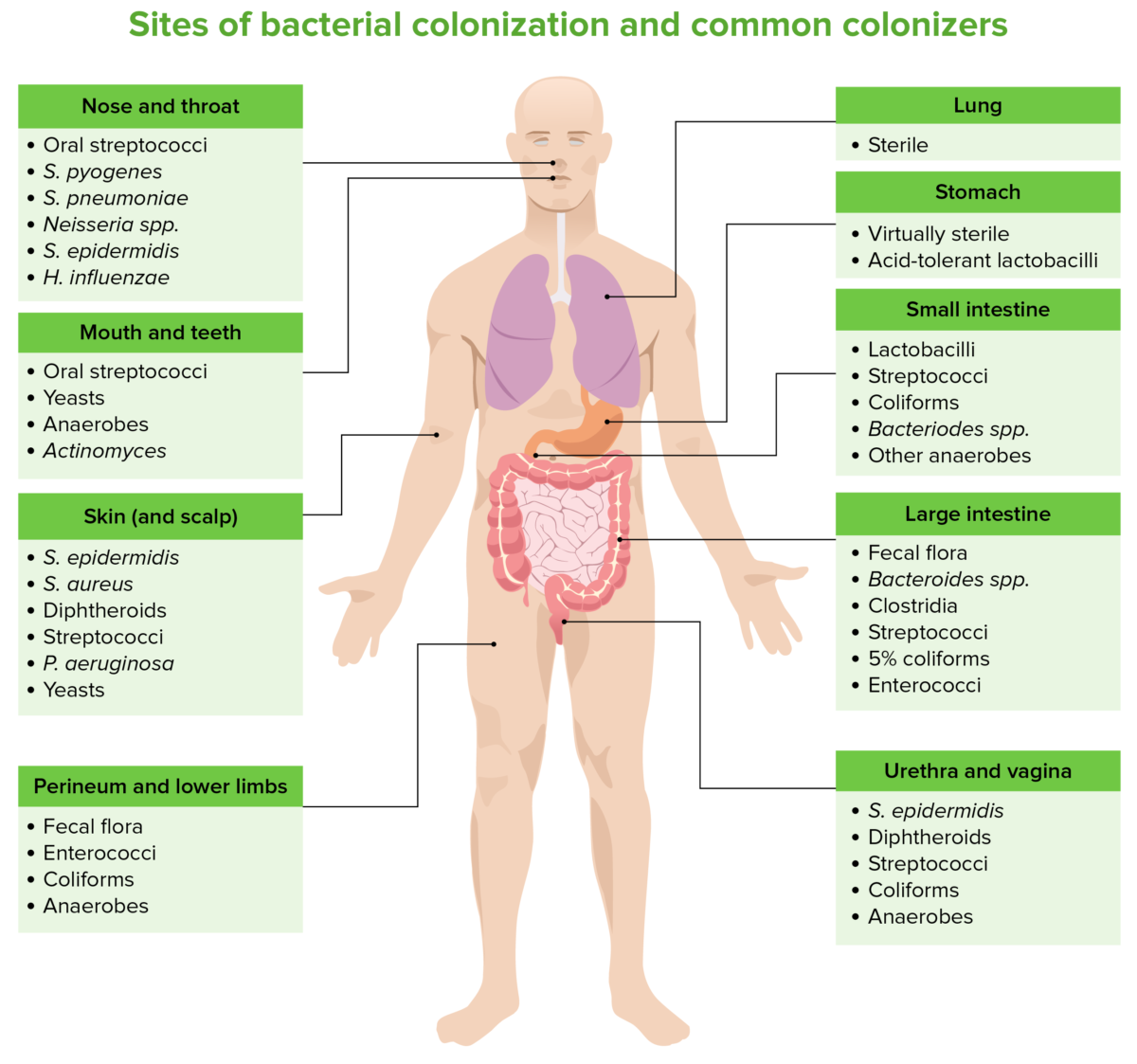
Sites of bacterial colonization and common colonizers
Image by Lecturio. License: CC BY-NC-SA 4.0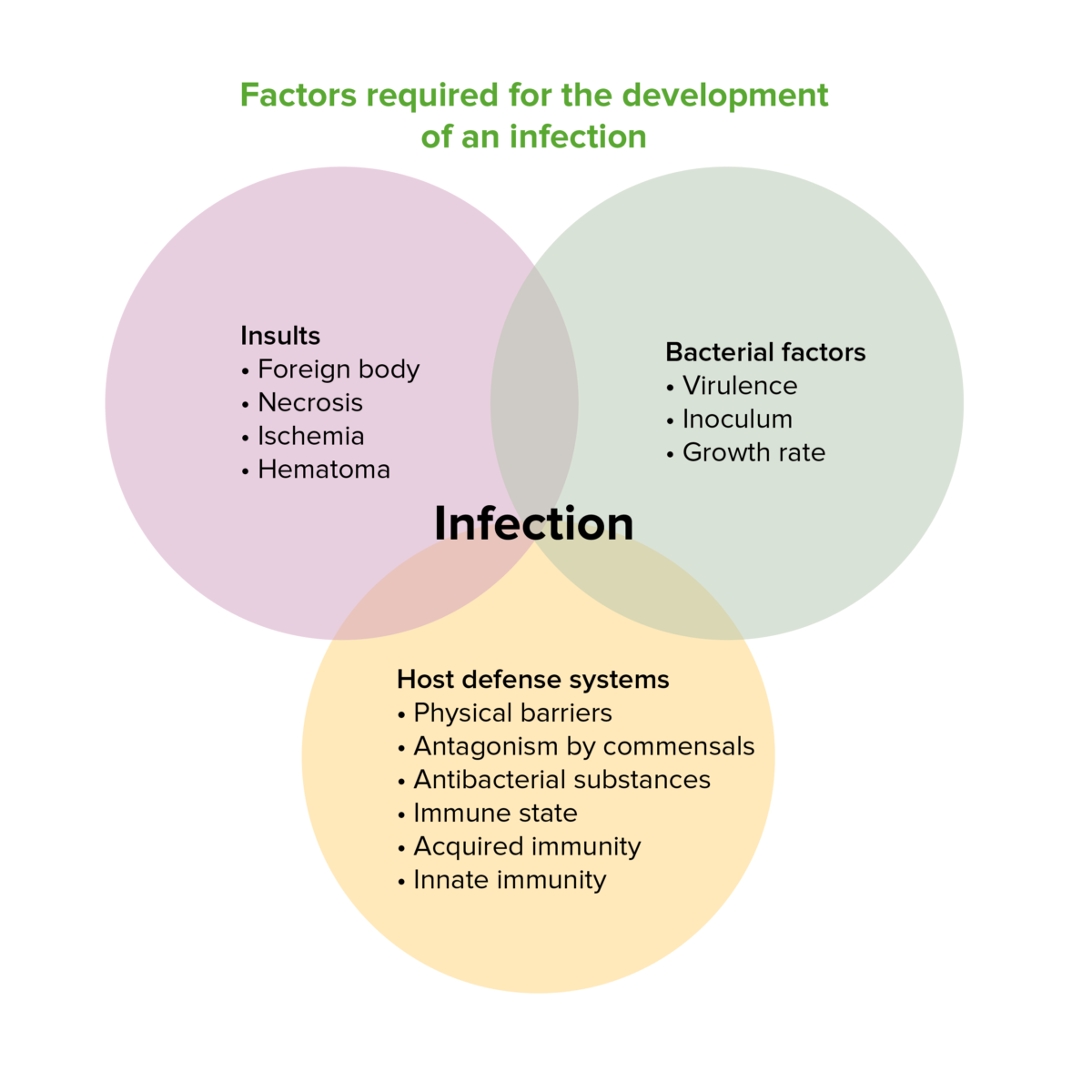
Factors required for the development of an infection
Image by Lecturio. License: CC BY-NC-SA 4.0
Superficial surgical wound infection:
Opening and dehiscence of the wound edges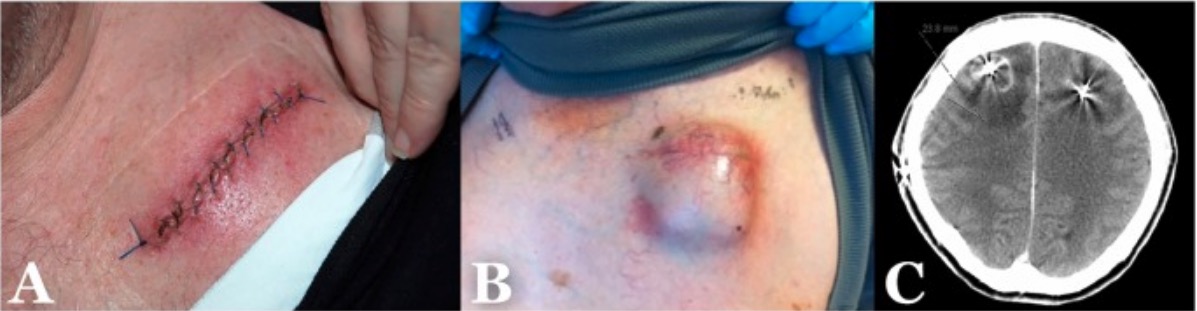
Examples of the different types of surgical site infections (SSIs):
A: Superficial incisional SSI
B: Deep incisional SSI
C: Organ/space SSI
Systemic inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation:
Local inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation:
Septic shock Septic shock Sepsis associated with hypotension or hypoperfusion despite adequate fluid resuscitation. Perfusion abnormalities may include, but are not limited to lactic acidosis; oliguria; or acute alteration in mental status. Sepsis and Septic Shock:
The diagnosis of SSI relies primarily on clinical findings. Diagnostic imaging and laboratory studies are helpful for identifying deep tissue and organ/space infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease.
Clinical findings (local):
Sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock findings (systemic):
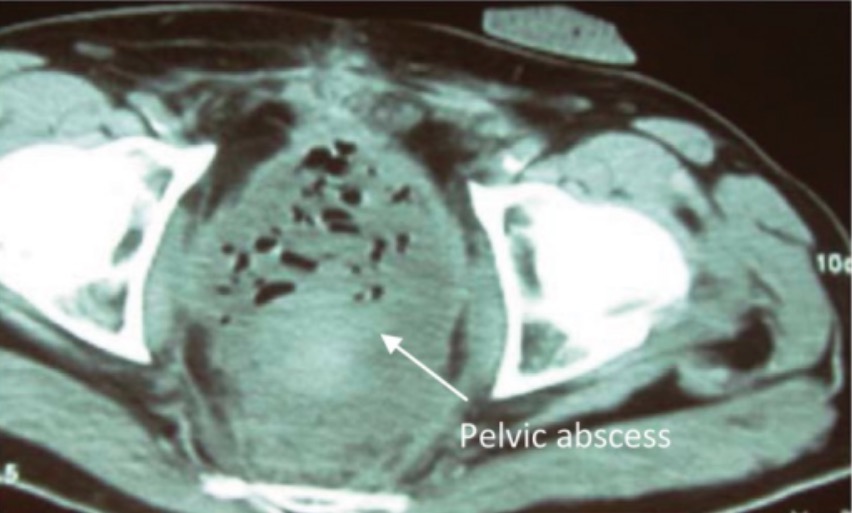
Postsurgical pelvic abscess
Image: “Axial computed tomography of the pelvis showing pelvic abscess” by Plastic and Reconstructive Surgery Department, Cork University Hospital, Wilton, Cork, Ireland. License: CC BY 3.0The management of SSIs may include antibiotics, abscess Abscess Accumulation of purulent material in tissues, organs, or circumscribed spaces, usually associated with signs of infection. Chronic Granulomatous Disease drainage (open or percutaneous), and removal of infected prosthetic material.
| Organism | 1st choice | Alternative |
|---|---|---|
| Methicillin-sensitive Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess | Cefazolin Cefazolin A semisynthetic cephalosporin analog with broad-spectrum antibiotic action due to inhibition of bacterial cell wall synthesis. It attains high serum levels and is excreted quickly via the urine. Cephalosporins | Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides |
| Methicillin-resistant Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides | Linezolid Linezolid An oxazolidinone and acetamide derived anti-bacterial agent and protein synthesis inhibitor that is used in the treatment of gram-positive bacterial infections of the skin and respiratory tract. Oxazolidinones or daptomycin Daptomycin A cyclic lipopeptide antibiotic that inhibits gram-positive bacteria. Lipopeptides and Lipoglycopeptides |
| Coagulase-negative staphylococci Coagulase-negative staphylococci Staphylococcus | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides | Linezolid Linezolid An oxazolidinone and acetamide derived anti-bacterial agent and protein synthesis inhibitor that is used in the treatment of gram-positive bacterial infections of the skin and respiratory tract. Oxazolidinones or daptomycin Daptomycin A cyclic lipopeptide antibiotic that inhibits gram-positive bacteria. Lipopeptides and Lipoglycopeptides |
| Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pneumoniae | Benzylpenicillin | Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides |
| Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pyogenes (group A β-hemolytic streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus) | Benzylpenicillin, clindamycin Clindamycin An antibacterial agent that is a semisynthetic analog of lincomycin. Lincosamides | Clarithromycin Clarithromycin A semisynthetic macrolide antibiotic derived from erythromycin that is active against a variety of microorganisms. It can inhibit protein synthesis in bacteria by reversibly binding to the 50s ribosomal subunits. This inhibits the translocation of aminoacyl transfer-RNA and prevents peptide chain elongation. Macrolides and Ketolides |
| Enterococci | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides |
| Bacteroides Bacteroides Bacteroides is a genus of opportunistic, anaerobic, gram-negative bacilli. Bacteroides fragilis is the most common species involved in human disease and is part of the normal flora of the large intestine. Bacteroides spp. | Metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins–clavulanate |
| Escherichia coli Escherichia coli The gram-negative bacterium Escherichia coli is a key component of the human gut microbiota. Most strains of E. coli are avirulent, but occasionally they escape the GI tract, infecting the urinary tract and other sites. Less common strains of E. coli are able to cause disease within the GI tract, most commonly presenting as abdominal pain and diarrhea. Escherichia coli | Piperacillin Piperacillin Semisynthetic, broad-spectrum, ampicillin derived ureidopenicillin antibiotic proposed for pseudomonas infections. It is also used in combination with other antibiotics. Penicillins– tazobactam Tazobactam A penicillanic acid and sulfone derivative and potent beta-lactamase inhibitor that enhances the activity of other anti-bacterial agents against beta-lactamase producing bacteria. Cephalosporins | Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Haemophilus influenzae Haemophilus Influenzae A species of Haemophilus found on the mucous membranes of humans and a variety of animals. The species is further divided into biotypes I through viii. Haemophilus | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins–clavulanate |
| Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella spp. | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins–clavulanate | Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Proteus Proteus Proteus spp. are gram-negative, facultatively anaerobic bacilli. Different types of infection result from Proteus, but the urinary tract is the most common site. The majority of cases are caused by Proteus mirabilis (P. mirabilis). The bacteria are part of the normal intestinal flora and are also found in the environment. Proteus spp. | Amoxicillin Amoxicillin A broad-spectrum semisynthetic antibiotic similar to ampicillin except that its resistance to gastric acid permits higher serum levels with oral administration. Penicillins–clavulanate | Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Pseudomonas aeruginosa Pseudomonas aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas | Piperacillin Piperacillin Semisynthetic, broad-spectrum, ampicillin derived ureidopenicillin antibiotic proposed for pseudomonas infections. It is also used in combination with other antibiotics. Penicillins– tazobactam Tazobactam A penicillanic acid and sulfone derivative and potent beta-lactamase inhibitor that enhances the activity of other anti-bacterial agents against beta-lactamase producing bacteria. Cephalosporins | Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Clostridium spp. | Benzylpenicillin, metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess | Metronidazole Metronidazole A nitroimidazole used to treat amebiasis; vaginitis; trichomonas infections; giardiasis; anaerobic bacteria; and treponemal infections. Pyogenic Liver Abscess |