Lipopeptides and lipoglycopeptides are classes of antibiotics that have activity against gram-positive Gram-Positive Penicillins bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology and that act on the bacterial cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic. Lipopeptides (daptomycin) disrupt the cell membrane Cell Membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane by creating an ion-conducting channel and causing potassium Potassium An element in the alkali group of metals with an atomic symbol k, atomic number 19, and atomic weight 39. 10. It is the chief cation in the intracellular fluid of muscle and other cells. Potassium ion is a strong electrolyte that plays a significant role in the regulation of fluid volume and maintenance of the water-electrolyte balance. Hyperkalemia efflux and membrane depolarization Depolarization Membrane Potential. The subsequent processes lead to inhibited protein synthesis Synthesis Polymerase Chain Reaction (PCR) and eventual bacterial cell death Cell death Injurious stimuli trigger the process of cellular adaptation, whereby cells respond to withstand the harmful changes in their environment. Overwhelmed adaptive mechanisms lead to cell injury. Mild stimuli produce reversible injury. If the stimulus is severe or persistent, injury becomes irreversible. Apoptosis is programmed cell death, a mechanism with both physiologic and pathologic effects. Cell Injury and Death. Lipoglycopeptides have a dual action of inhibiting bacterial cell-wall synthesis Synthesis Polymerase Chain Reaction (PCR) by binding peptidoglycan Peptidoglycan Penicillins precursors and causing cell membrane Cell Membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane depolarization Depolarization Membrane Potential. Telavancin, dalbavancin, and oritavancin belong to this group of drugs. All these medications are administered IV, as they have poor oral absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption. The lipopeptides and lipoglycopeptides are excreted unchanged in the urine. Dosage Dosage Dosage Calculation adjustments are generally needed in cases of reduced renal function. Both classes of antibiotics are used as alternative agents for gram-positive Gram-Positive Penicillins infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease ( bacteremia Bacteremia The presence of viable bacteria circulating in the blood. Fever, chills, tachycardia, and tachypnea are common acute manifestations of bacteremia. The majority of cases are seen in already hospitalized patients, most of whom have underlying diseases or procedures which render their bloodstreams susceptible to invasion. Glycopeptides, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and soft tissue Soft Tissue Soft Tissue Abscess infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease). Telavancin is also effective against hospital-acquired and ventilator-associated pneumonia Ventilator-Associated Pneumonia Multidrug-resistant Organisms and Nosocomial Infections.
Last updated: Aug 18, 2022
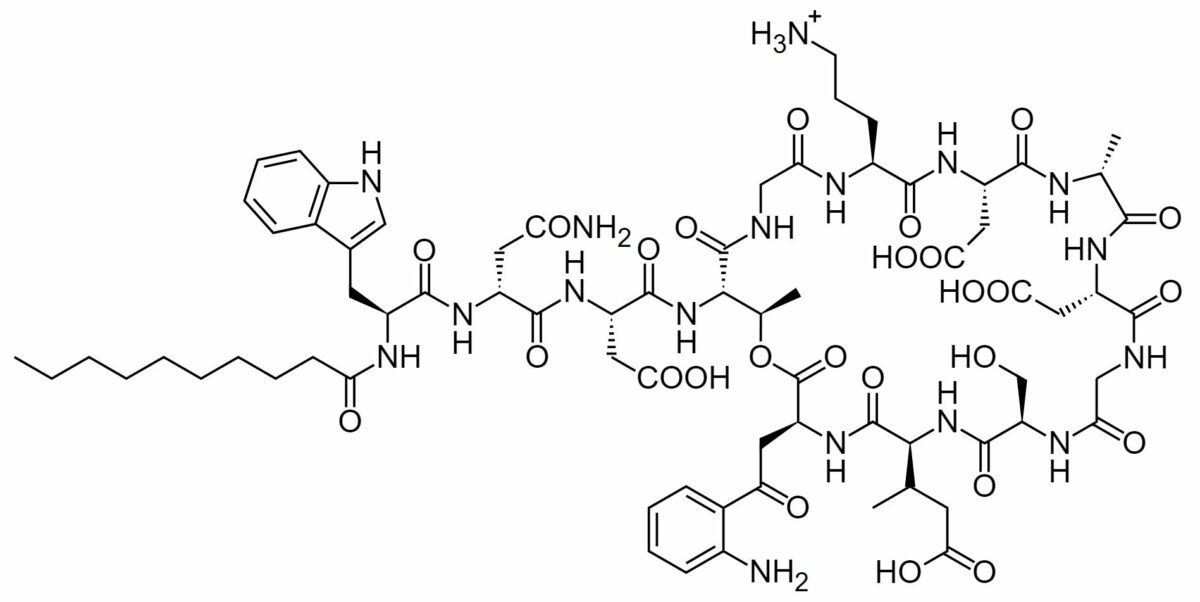
Chemical structure of daptomycin:
Daptomycin is a large molecule that is composed of multiple amino acids (including L-tryptophan at the upper left) and decanoic acid (the saturated, medium-chain fatty acid at the lower left).
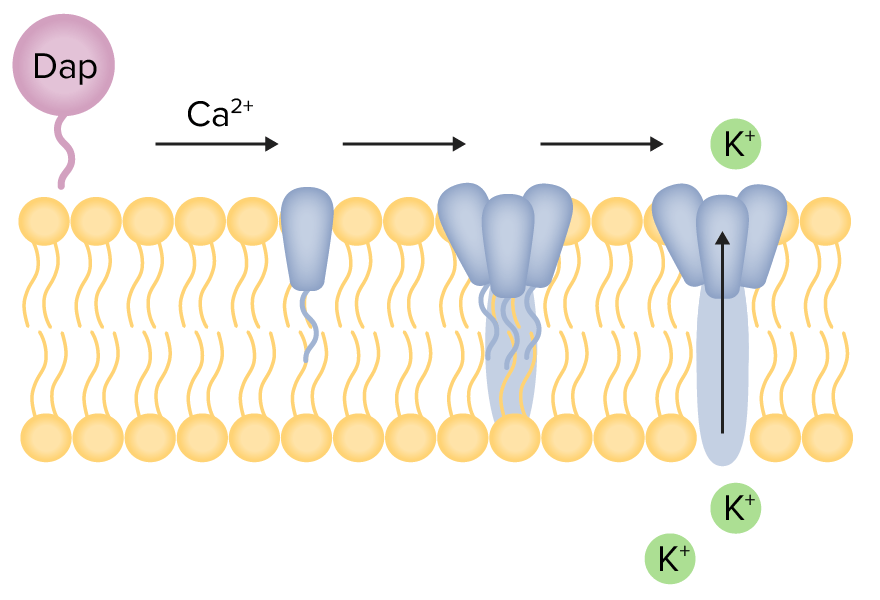
Mechanism of action for daptomycin:
Daptomycin (Dap) complexes with calcium, allowing it to integrate into the bacterial cell membrane, The daptomycin molecules aggregate to form a channel-like hole in the membrane. Potassium ions are able to leak out of the membrane, and rapid depolarization occurs. There is loss of ion gradient, which eventually leads to inhibition of protein synthesis, effectively resulting in cell death.
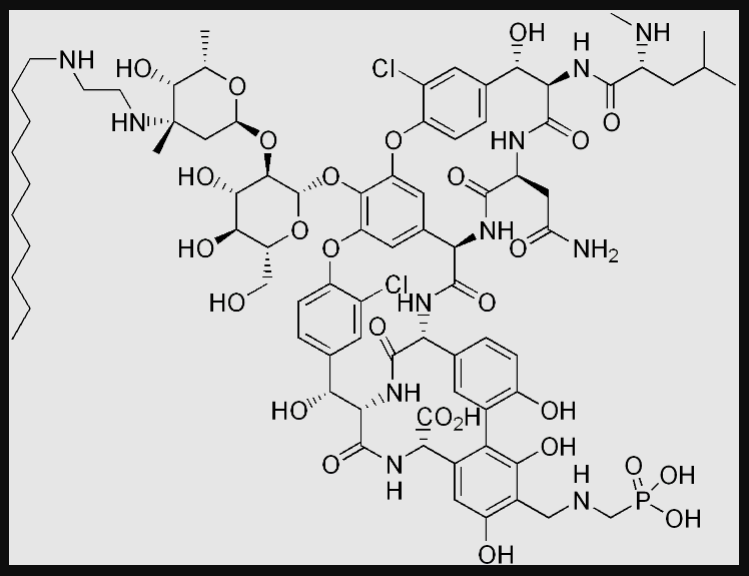
Chemical structure of telavancin
Image: “Telavancin” by Edgar181. License: Public Domain
Chemical structure of oritavancin
Image: “Oritavancin” by Fvasconcellos. License: Public Domain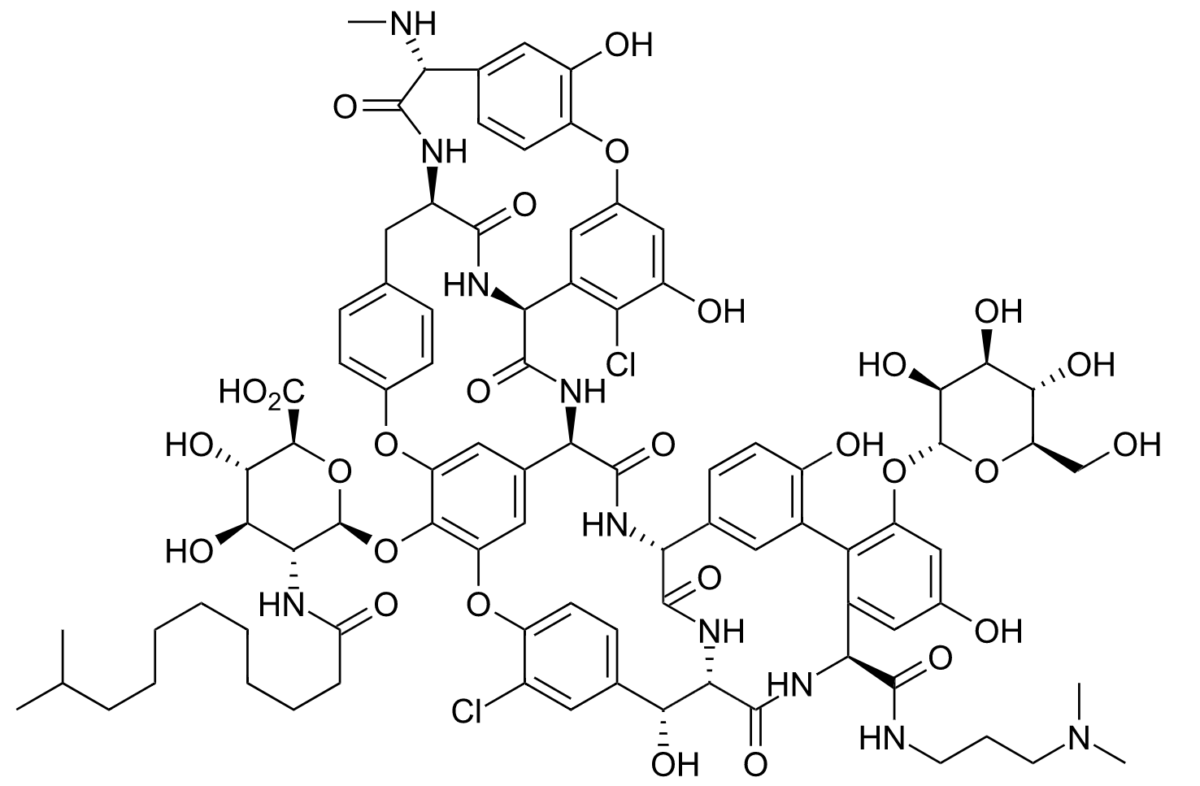
Chemical structure of dalbavancin
Image: “Dalbavancin B0” by Hbf878. License: CC0 1.0Lipopeptides and lipoglycopeptides are agents active against gram-positive Gram-Positive Penicillins bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology.
The following antibiotics are agents with activity against gram-positive Gram-Positive Penicillins bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology. All act on the bacterial cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic through varying mechanisms.
| Class of antibiotics | Mechanism of action | Drugs |
|---|---|---|
| Lipopeptides | Disruption of the bacterial cell membrane Cell Membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane by generating an ion-conducting channel, depolarizing the membrane, and leading to cell death Cell death Injurious stimuli trigger the process of cellular adaptation, whereby cells respond to withstand the harmful changes in their environment. Overwhelmed adaptive mechanisms lead to cell injury. Mild stimuli produce reversible injury. If the stimulus is severe or persistent, injury becomes irreversible. Apoptosis is programmed cell death, a mechanism with both physiologic and pathologic effects. Cell Injury and Death | Daptomycin |
| Glycopeptides Glycopeptides The glycopeptide antibiotics (GPAs) vancomycin and teicoplanin are inhibitors of bacterial cell wall synthesis and considered the last resort treatment of severe infections due to gram-positive bacteria such as Staphylococcus aureus, Enterococcus spp., and Clostridiodes difficile. Glycopeptides | Inhibition of cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic synthesis Synthesis Polymerase Chain Reaction (PCR) by binding to the D-alanyl-D-alanine terminus of cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic peptidoglycan Peptidoglycan Penicillins (PG) precursors |
|
| Lipoglycopeptides | Dual action of inhibition of cell wall Cell wall The outermost layer of a cell in most plants; bacteria; fungi; and algae. The cell wall is usually a rigid structure that lies external to the cell membrane, and provides a protective barrier against physical or chemical agents. Cell Types: Eukaryotic versus Prokaryotic synthesis Synthesis Polymerase Chain Reaction (PCR) and depolarization Depolarization Membrane Potential of the cell membrane Cell Membrane A cell membrane (also known as the plasma membrane or plasmalemma) is a biological membrane that separates the cell contents from the outside environment. A cell membrane is composed of a phospholipid bilayer and proteins that function to protect cellular DNA and mediate the exchange of ions and molecules. The Cell: Cell Membrane |
|
Different antibiotics have varying degrees of activity against different bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology. The table below outlines the antibiotics with activity against 3 important classes of bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology: gram-positive Gram-Positive Penicillins cocci Cocci Bacteriology, gram-negative bacilli Bacilli Shigella, and anaerobes Anaerobes Lincosamides.
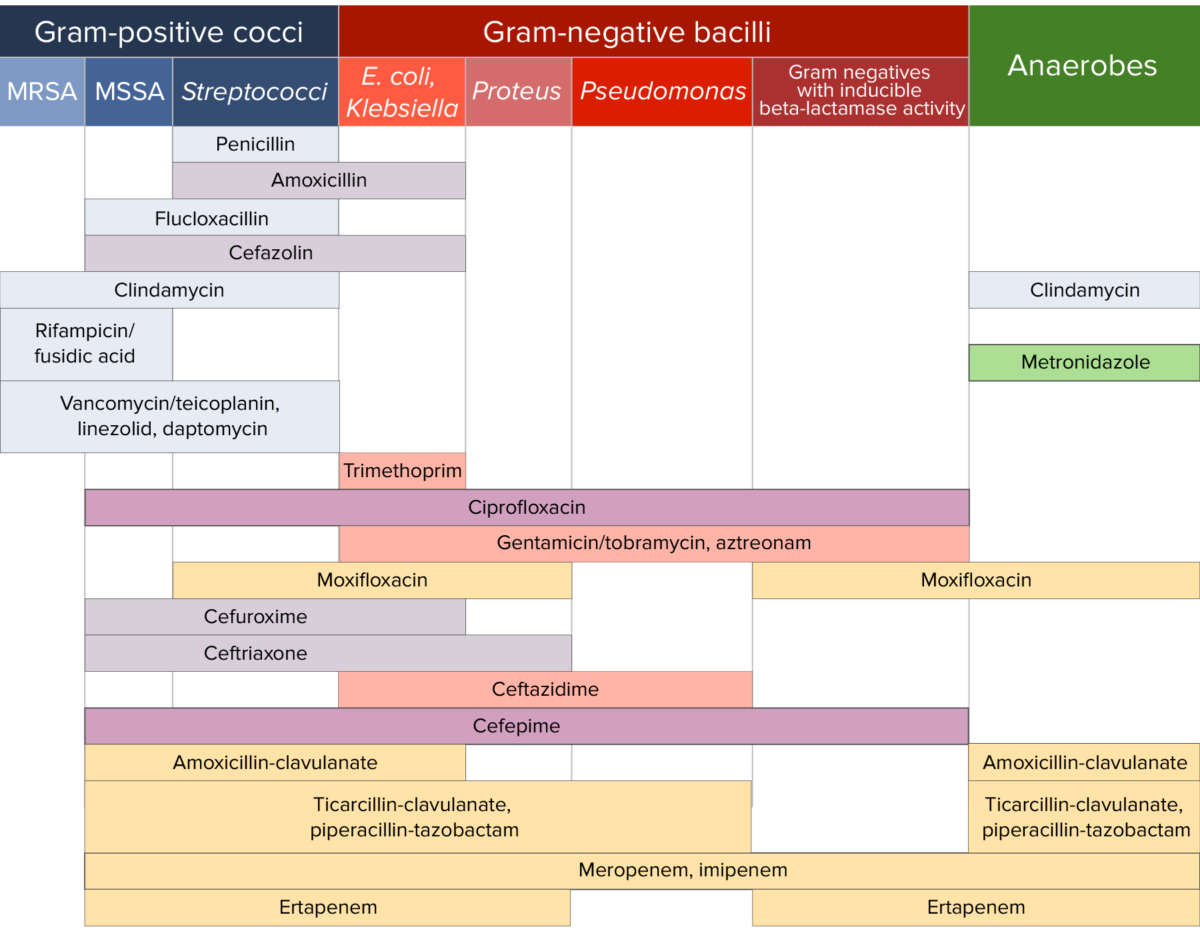
Antibiotic sensitivity:
Chart comparing the microbial coverage of different antibiotics for gram-positive cocci, gram-negative bacilli, and anaerobes.