The kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy, solid organs located in the lower back, are extremely important in regulating homeostasis Homeostasis The processes whereby the internal environment of an organism tends to remain balanced and stable. Cell Injury and Death through their role in maintaining blood volume, electrolyte balance, acid–base equilibrium Equilibrium Occurs when tumor cells survive the initial elimination attempt These cells are not able to progress, being maintained in a state of dormancy by the adaptive immune system. In this phase, tumor immunogenicity is edited, where T cells keep selectively attacking highly immunogenic tumor cells.This attack leaves other cells with less immunogenicity to potentially develop resistance to the immune response. Cancer Immunotherapy, blood-pressure regulation, and removal of metabolic waste from the blood. Evaluation of renal function and early detection of kidney dysfunction is of primary importance. Tests of renal function are useful in identifying the presence of renal disease, monitoring the response of kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy to treatment, and determining the progression of renal disease.
Last updated: May 17, 2024
Nephron Nephron The functional units of the kidney, consisting of the glomerulus and the attached tubule. Kidneys: Anatomy:
Parts of nephron Nephron The functional units of the kidney, consisting of the glomerulus and the attached tubule. Kidneys: Anatomy:
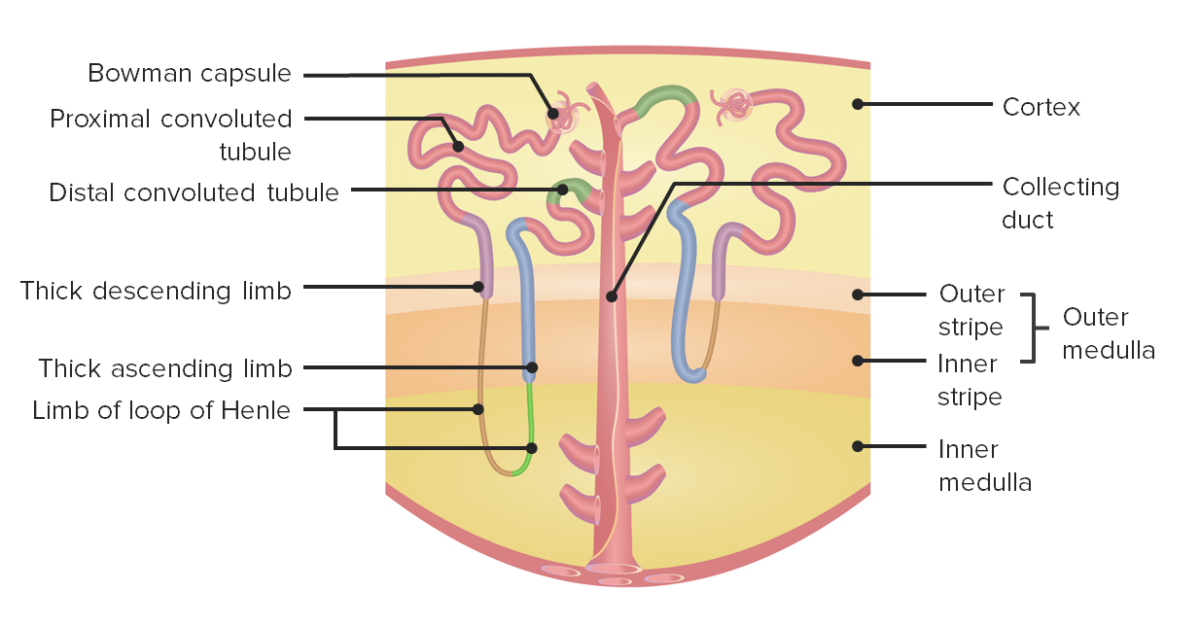
Nephron anatomy:
The left side shows a juxtamedullary nephron, while the right side shows a cortical nephron.
Urine is a waste by-product composed of excess water and metabolic waste filtered out of the bloodstream by nephrons. Urine formation is a stepwise process.
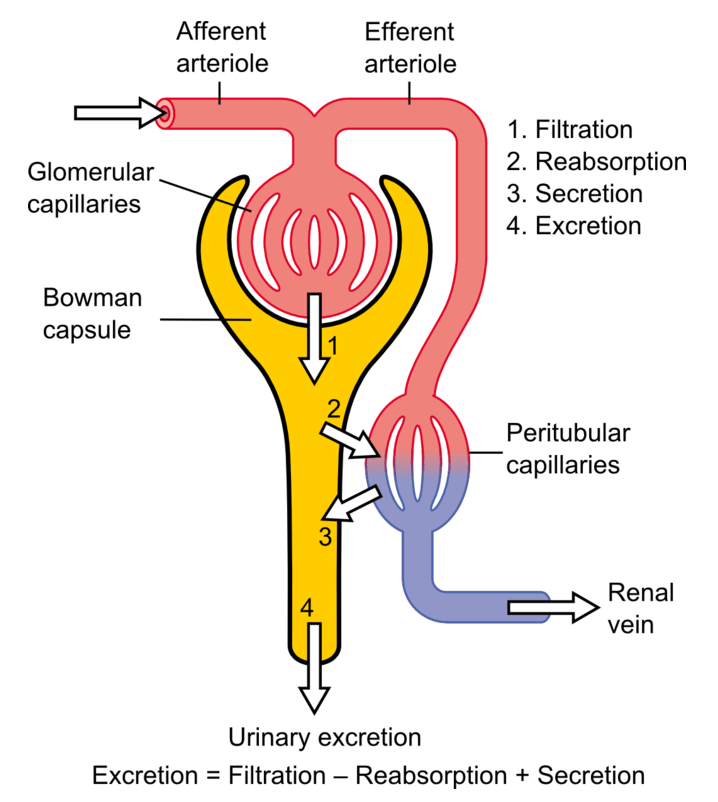
The basic anatomy of the nephron and the steps involved in urine formation
Image: “Physiology of Nephron” by Madhero88. License: CC BY 3.0, edited by Lecturio.The most commonly used marker to assess kidney function is the measurement of excreted creatinine, based on which the eGFR can be calculated.
Provides more useful information than either tests alone:
There are 3 basic components to urinalysis Urinalysis Examination of urine by chemical, physical, or microscopic means. Routine urinalysis usually includes performing chemical screening tests, determining specific gravity, observing any unusual color or odor, screening for bacteriuria, and examining the sediment microscopically. Urinary Tract Infections (UTIs) in Children:
| Cast | Clinical significance/diseases |
|---|---|
| RBC casts |
|
| WBC casts |
|
| Epithelial cell casts |
|
| Fatty casts Fatty Casts Minimal Change Disease | Nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome |
| Granular, muddy brown casts | Acute tubular necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage (ATN) |
| Waxy casts |
|
| Hyaline casts |
|
The following conditions are associated with abnormal kidney function tests:
The following conditions are associated with abnormal urinalysis Urinalysis Examination of urine by chemical, physical, or microscopic means. Routine urinalysis usually includes performing chemical screening tests, determining specific gravity, observing any unusual color or odor, screening for bacteriuria, and examining the sediment microscopically. Urinary Tract Infections (UTIs) in Children: