Minimal change disease (MCD), also known as lipoid nephrosis, is the most common cause of nephrotic syndrome in children Nephrotic Syndrome in Children Nephrotic syndrome is a renal disorder caused by conditions that increase the permeability of the glomerular filtration barriers. Nephrotic syndrome affects all age groups but has a higher pediatric prevalence. This disorder can be due to both primary (renal) and secondary (systemic) causes. Nephrotic Syndrome in Children. The designation “minimal change” comes from the very little changes noticed in kidney biopsies under light microscopy. Hallmark clinical findings include edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema, proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children, hypoalbuminemia Hypoalbuminemia A condition in which albumin level in blood (serum albumin) is below the normal range. Hypoalbuminemia may be due to decreased hepatic albumin synthesis, increased albumin catabolism, altered albumin distribution, or albumin loss through the urine (albuminuria). Nephrotic Syndrome in Children, and hyperlipidemia. Diagnosis is based on clinical suspicion and supportive lab findings. Corticosteroid administration is the cornerstone of management, and the prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is largely favorable.
Last updated: May 17, 2024
Minimal change disease (MCD) is a primary glomerular disorder of unclear etiology that causes nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome. The term “minimal” refers to the minimal structural changes of the glomeruli when observed under light microscopy.
Nephrotic syndrome:
The condition is accompanied by retention of water and sodium. The image shows facial swelling/edema. The degree to which edema occurs can vary. There may be slight edema in the eyelids that decreases during the day, swelling affecting the lower limbs, generalized swelling, or full-blown anasarca.
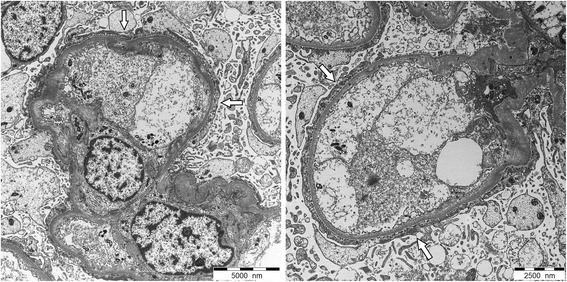
Electron microscopy of a glomerulus seen in a patient with minimal change disease (MCD):
In minimal change disease, podocytes are fused, appearing as a single layer (white arrows).
Electron-dense deposits are not seen in MCD, and the glomerular basement membrane remains of normal thickness distinguish it from other glomerular diseases.
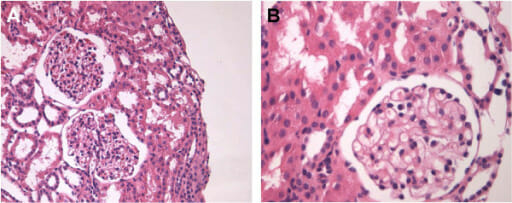
Renal biopsy of minimal change disease on normal light microscopy
A: H&E stain, 200x
B: H&E stain, 400x