Chorioretinitis is the inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the posterior segment of the eye, including the choroid Choroid The thin, highly vascular membrane covering most of the posterior of the eye between the retina and sclera. Eye: Anatomy and the retina Retina The ten-layered nervous tissue membrane of the eye. It is continuous with the optic nerve and receives images of external objects and transmits visual impulses to the brain. Its outer surface is in contact with the choroid and the inner surface with the vitreous body. The outermost layer is pigmented, whereas the inner nine layers are transparent. Eye: Anatomy. The condition is usually caused by infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, the most common of which is toxoplasmosis Toxoplasmosis Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Felines are the definitive host, but transmission to humans can occur through contact with cat feces or the consumption of contaminated foods. The clinical presentation and complications depend on the host's immune status. Toxoplasma/Toxoplasmosis. Some of these infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease can affect the fetus in utero and present as congenital abnormalities Congenital Abnormalities Malformations of organs or body parts during development in utero. Omphalocele. Systemic diseases such as sarcoidosis Sarcoidosis Sarcoidosis is a multisystem inflammatory disease that causes noncaseating granulomas. The exact etiology is unknown. Sarcoidosis usually affects the lungs and thoracic lymph nodes, but it can also affect almost every system in the body, including the skin, heart, and eyes, most commonly. Sarcoidosis are also associated with this condition. Painless blurry vision Vision Ophthalmic Exam, floaters, and scotomas are typical clinical features. With systemic and congenital disorders, extraocular manifestations are observed. Diagnosis is by funduscopy and slit-lamp examination Slit-Lamp Examination Blepharitis, with use of laboratory tests and imaging dictated by the risk factors, medical history, and treatment monitoring. Treatment is directed toward eliminating the infection with antibiotics or antivirals and reducing inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation with glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids or immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants.
Last updated: Feb 14, 2023
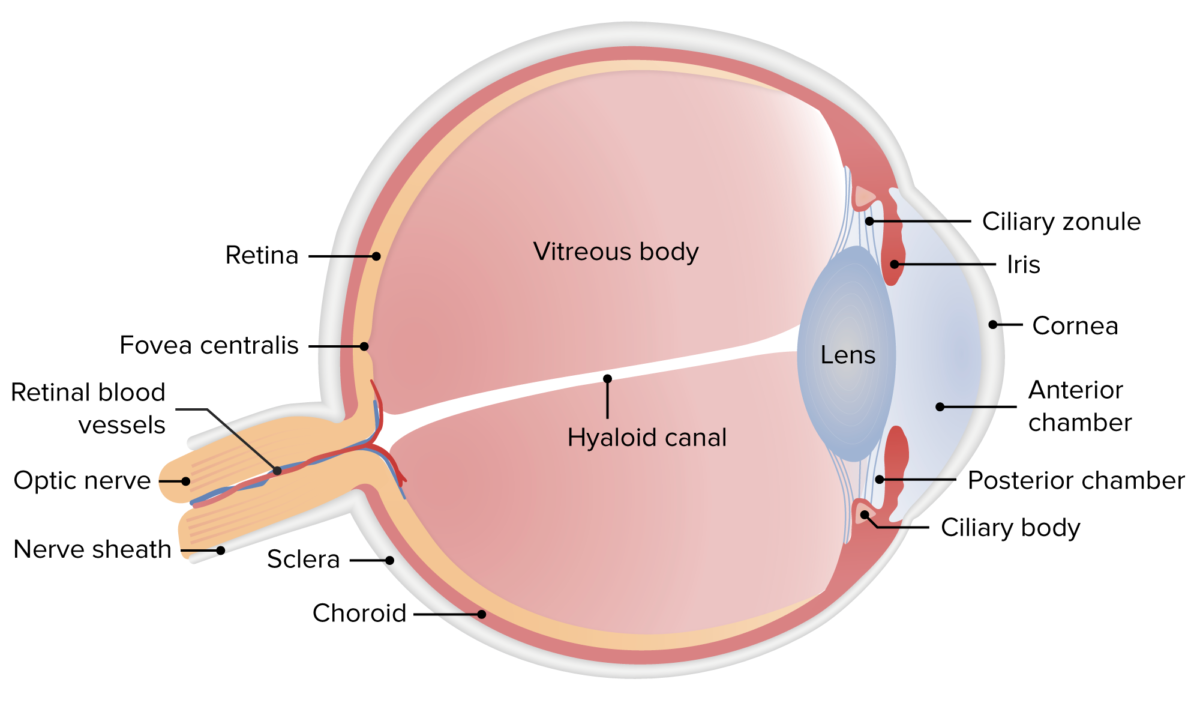
Anatomy of the human eye
Image by Lecturio.Active infection
Reactivated infection
Guided by:
| Infection | Ophthalmologic findings |
|---|---|
| Toxoplasmosis Toxoplasmosis Toxoplasmosis is an infectious disease caused by Toxoplasma gondii, an obligate intracellular protozoan parasite. Felines are the definitive host, but transmission to humans can occur through contact with cat feces or the consumption of contaminated foods. The clinical presentation and complications depend on the host’s immune status. Toxoplasma/Toxoplasmosis |
|
| Congenital toxoplasmosis Congenital toxoplasmosis Prenatal protozoal infection with toxoplasma gondii which is associated with injury to the developing fetal nervous system. The severity of this condition is related to the stage of pregnancy during which the infection occurs; first trimester infections are associated with a greater degree of neurologic dysfunction. Clinical features include hydrocephalus; microcephaly; deafness; cerebral calcifications; seizures; and psychomotor retardation. Signs of a systemic infection may also be present at birth, including fever, rash, and hepatosplenomegaly. Toxoplasma/Toxoplasmosis | Punched-out or excavated macular lesion |
| CMV retinitis CMV retinitis Infection of the retina by cytomegalovirus characterized by retinal necrosis, hemorrhage, vessel sheathing, and retinal edema. Cytomegalovirus retinitis is a major opportunistic infection in AIDS patients and can cause blindness. Retinal Detachment |
|
| Tuberculosis Tuberculosis Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis complex bacteria. The bacteria usually attack the lungs but can also damage other parts of the body. Approximately 30% of people around the world are infected with this pathogen, with the majority harboring a latent infection. Tuberculosis spreads through the air when a person with active pulmonary infection coughs or sneezes. Tuberculosis |
|
| Toxocariasis Toxocariasis Toxocariasis is caused by the nematodes Toxocara canis and T. cati. These species frequently infect dogs and cats and are most commonly transmitted to humans via accidental ingestion of eggs through the fecal-oral route. Toxocara are not able to complete their life cycle in humans, but they do migrate to organs (including the liver, lungs, heart, brain, and eyes), where they cause inflammation and tissue damage. Toxocariasis | Whitish granuloma in periphery or posterior pole (from larval localization) |
| Syphilis Syphilis Syphilis is a bacterial infection caused by the spirochete Treponema pallidum pallidum (T. p. pallidum), which is usually spread through sexual contact. Syphilis has 4 clinical stages: primary, secondary, latent, and tertiary. Syphilis | Great imitator: presents as chorioretinitis, papilledema Papilledema Swelling of the optic disk, usually in association with increased intracranial pressure, characterized by hyperemia, blurring of the disk margins, microhemorrhages, blind spot enlargement, and engorgement of retinal veins. Chronic papilledema may cause optic atrophy and visual loss. Idiopathic Intracranial Hypertension, optic neuritis Optic neuritis Inflammation of the optic nerve. Commonly associated conditions include autoimmune disorders such as multiple sclerosis, infections, and granulomatous diseases. Clinical features include retro-orbital pain that is aggravated by eye movement, loss of color vision, and contrast sensitivity that may progress to severe visual loss, an afferent pupillary defect (Marcus-Gunn pupil), and in some instances optic disc hyperemia and swelling. Inflammation may occur in the portion of the nerve within the globe (neuropapillitis or anterior optic neuritis) or the portion behind the globe (retrobulbar neuritis or posterior optic neuritis). Cranial Nerve Palsies, placoid lesions |
| Ocular histoplasmosis Histoplasmosis Histoplasmosis is an infection caused by Histoplasma capsulatum, a dimorphic fungus. Transmission is through inhalation, and exposure to soils containing bird or bat droppings increases the risk of infection. Most infections are asymptomatic; however, immunocompromised individuals generally develop acute pulmonary infection, chronic infection, or even disseminated disease. Histoplasma/Histoplasmosis syndrome | Discrete chorioretinal oval-round lesions (“punched-out” histo spots) |
Fundus photos of the left eye showing tuberculous vitritis, vasculitis, and chorioretinitis superior to the macula
Image: “Left eye showing vitritis, vasculitis and chorioretinitis” by Department of Ophthalmology, Tan Tock Seng Hospital, Singapore, 308433 Singapore. License: CC BY 4.0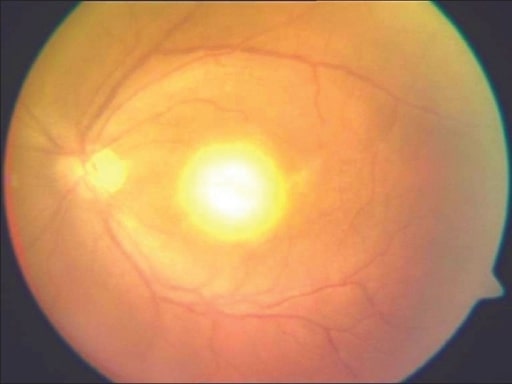
Typical “headlight in the fog appearance” in a patient with acquired toxoplasmosis
Image: “Headlight in the fog” appearance by Medical Research Foundation, Chennai, India. License: CC BY 2.0
Fundus picture showing a typical punched-out macular scar of a healed congenital toxoplasmosis
Image: “healed congenital toxoplasmosis” by Medical Research Foundation, Chennai, India. License: CC BY 2.0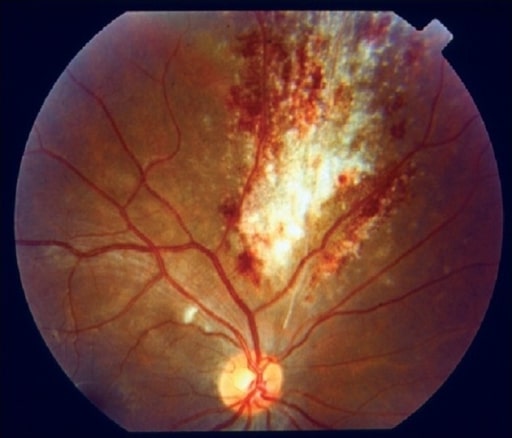
Fundus picture showing a typical “pizza pie appearance” in a patient with cytomegalovirus retinitis
Image: “pizza pie appearance” by Medical Research Foundation, Chennai, India. License: CC BY 2.0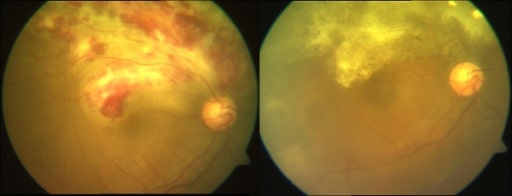
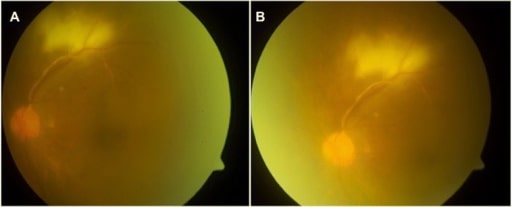
Composite color fundus photographs showing a case of active and healed CMV retinitis. Pre- (left) and post-treatment (right) with ganciclovir.
Image: “active and healed CMV retinitis” by Medical Research Foundation, 18, College Road, Sankara Nethralaya, Chennai, 600006, India. License: CC BY 2.0
Drusen are yellow deposits under the retina, the light-sensitive tissue at the back of the eye. Drusen consist of lipids and fatty protein.
Image: “Oxidative stress, innate immunity, and age-related macular degeneration” by Department of Ophthalmology and Shiley Eye Institute, University of California San Diego, San Diego, CA, USA. License: CC BY 4.0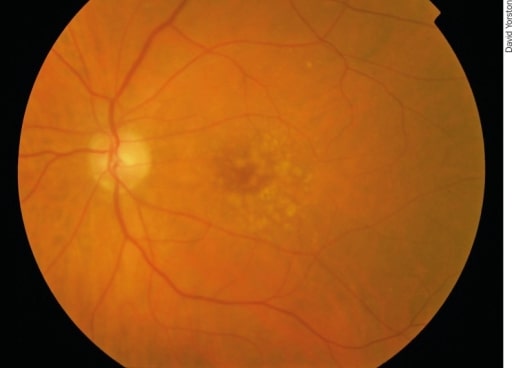
Early AMD: There are irregular pale dots at the macula, which are called drusen. They are caused by a build-up of waste products from photoreceptor metabolism. Although drusen are associated with AMD, most patients with drusen will not develop severe AMD.
Image: “Early AMD” by Africa Regional Medical Advisor: Fred Hollows Foundation, Kigali, Rwanda. License: CC BY 2.0| Disease/condition | Ophthalmologic findings |
|---|---|
| Sarcoidosis Sarcoidosis Sarcoidosis is a multisystem inflammatory disease that causes noncaseating granulomas. The exact etiology is unknown. Sarcoidosis usually affects the lungs and thoracic lymph nodes, but it can also affect almost every system in the body, including the skin, heart, and eyes, most commonly. Sarcoidosis |
|
| Behcet’s disease |
|
| Birdshot retinochoroidopathy | Birdshot lesions: cream-colored choroidal lesions radiating from optic disc Optic disc The portion of the optic nerve seen in the fundus with the ophthalmoscope. It is formed by the meeting of all the retinal ganglion cell axons as they enter the optic nerve. Eye: Anatomy |
| White dot syndrome |
|
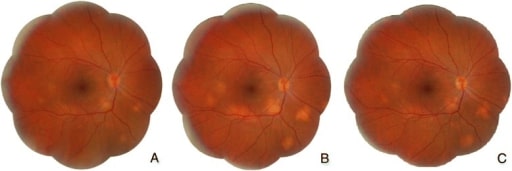
Sarcoidosis:
A. Initial visit: optic disc hyperemia and edema and yellowish subretinal lesions located in the posterior pole and lower midperiphery
B. After 6-month therapy of prednisone: decreased optic disc hyperemia and edema but increased choroidal granulomas
C. After 18-month therapy of prednisone and methotrexate: decreased choroidal granulomas
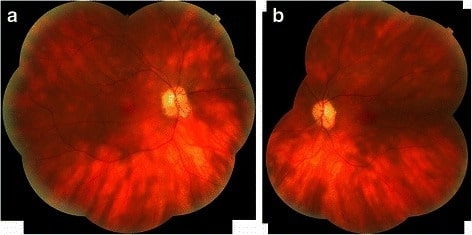
Photomontage of right (a) and left (b) eyes of a patient with birdshot chorioretinopathy revealing classic creamy ovoid lesions and the linear streaks emanating from the optic disc
Image: “Birdshot chorioretinopathy” by Department of Ophthalmology, Queen Elizabeth Hospital Birmingham, University Hospitals Birmingham NHS Foundation Trust, Birmingham, UK. License: CC BY 4.0Non-infectious chorioretinitis is treated with corticosteroids and immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants.
For non-resolving chorioretinitis, rule out malignancies (masquerade syndromes).
The differential diagnoses of chorioretinitis include the following conditions: