Toxocariasis is caused by the nematodes Toxocara canis and T. cati. These species frequently infect dogs and cats and are most commonly transmitted to humans via accidental ingestion of eggs through the fecal–oral route. Toxocara are not able to complete their life cycle in humans, but they do migrate to organs (including the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy, lungs Lungs Lungs are the main organs of the respiratory system. Lungs are paired viscera located in the thoracic cavity and are composed of spongy tissue. The primary function of the lungs is to oxygenate blood and eliminate CO2. Lungs: Anatomy, heart, brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, and eyes), where they cause inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation and tissue damage. Depending on the affected site, patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may develop visceral larva migrans or ocular larva migrans. Visceral larva migrans can present with flu-like symptoms Flu-Like Symptoms Babesia/Babesiosis, as well as hepatic, pulmonary, neurologic, and cardiac manifestations. Ocular larva migrans presents with unilateral vision Vision Ophthalmic Exam impairment, and a white, elevated granuloma may be seen on fundus Fundus The superior portion of the body of the stomach above the level of the cardiac notch. Stomach: Anatomy examination. The diagnosis is guided by clinical suspicion and may be supported with serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus. Management includes anthelmintic therapy and steroids Steroids A group of polycyclic compounds closely related biochemically to terpenes. They include cholesterol, numerous hormones, precursors of certain vitamins, bile acids, alcohols (sterols), and certain natural drugs and poisons. Steroids have a common nucleus, a fused, reduced 17-carbon atom ring system, cyclopentanoperhydrophenanthrene. Most steroids also have two methyl groups and an aliphatic side-chain attached to the nucleus. Benign Liver Tumors for severe disease.
Last updated: Mar 28, 2025

Spherical Toxocara egg with a brown, granulated appearance
Image: “Toxocara (roundworm)” by SuSanA Secretariat. License: CC BY 2.0Toxocariasis is caused by the following species:
Transmission occurs through:
In animals Animals Unicellular or multicellular, heterotrophic organisms, that have sensation and the power of voluntary movement. Under the older five kingdom paradigm, animalia was one of the kingdoms. Under the modern three domain model, animalia represents one of the many groups in the domain eukaryota. Cell Types: Eukaryotic versus Prokaryotic:
In humans:
Most Toxocara infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are asymptomatic and have a benign Benign Fibroadenoma course. The 2 major forms of toxocariasis are visceral larva migrans and ocular larva migrans.
General:
Hepatic:
Pulmonary:
Less common manifestations:
Unilateral symptoms:
Findings:
Complications:
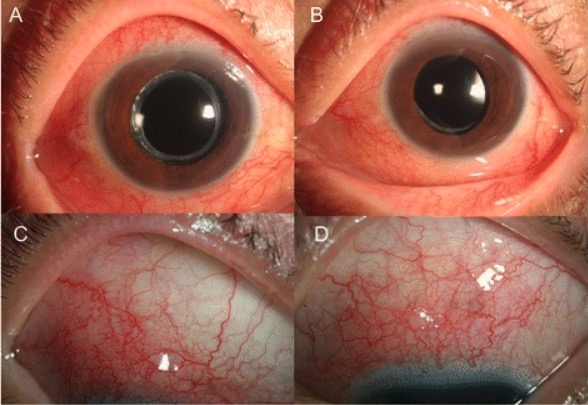
Images of the right (A and C) and left (B and D) eyes showing diffuse injection and scleral vessel engorgement, consistent with scleritis, due to Toxocara infection
Image: “Ocular toxocariasis” by Kang Yeun Pak et al. License: CC BY 4.0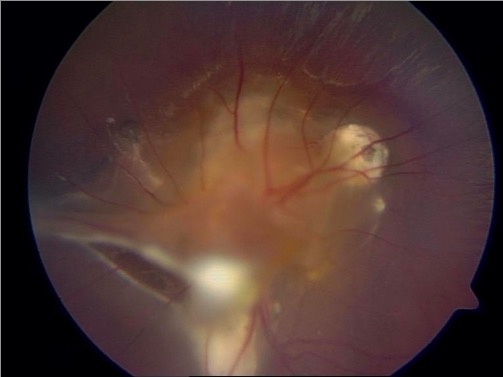
Fundoscopic examination showing subretinal granulomas with two fibrous traction bands proliferating at the periphery in a patient with ocular larva migrans due to Toxocara infection
Image: “Central and peripheric subretinal granulomas” by Department and Clinic of Tropical and Parasitic Diseases, University of Medical Sciences, Przybyszewskiego 49, 60-355 Poznań, Poland. License: CC BY 3.0The diagnosis of toxocariasis requires a high index of suspicion.
Serologic testing:
Supporting evaluation:
Imaging is usually guided by the patient’s clinical presentation.

CT image showing a small, oval, low-attenuation nodule in the right lobe of the liver (arrow) due to hepatic visceral larva migrans from Toxocara canis
Image: “Contrast-enhanced CT” by Lim JH. License: CC BY 2.5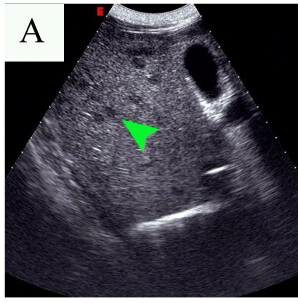
Abdominal ultrasound showing multiple small, hypoechoic lesions (arrowhead) in the liver due to hepatic visceral larva migrans from Toxocara
Image: “Abdominal ultrasound results before and after the first therapy” by Tao Yu et al. License: CC BY 2.0Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with mild symptoms do not require therapy, since the disease is self-limited. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with moderate to severe disease may be given:
| Organism | Enterobius vermicularis Enterobius Vermicularis Enterobius/Enterobiasis | Toxocara canis | Ascaris Ascaris Ascaris is a genus of parasitic nematodes. The infection, ascariasis, is most often caused by A. lumbricoides. Transmission occurs primarily via ingestion of water or food contaminated with Ascaris eggs. Most patients with ascariasis are asymptomatic. Ascaris/Ascariasis lumbricoides | Strongyloides stercoralis Strongyloides stercoralis A species of parasitic nematode widely distributed in tropical and subtropical countries. The females and their larvae inhabit the mucosa of the intestinal tract, where they cause ulceration and diarrhea. Strongyloidiasis | Schistosoma Schistosoma Schistosomiasis is an infection caused by Schistosoma, a trematode. Schistosomiasis occurs in developing countries with poor sanitation. Freshwater snails are the intermediate host and are transmitted to humans through skin contact with contaminated fresh water. The clinical presentation occurs as a result of the host’s immune response to antigens from the eggs. Schistosoma/Schistosomiasis mansoni |
|---|---|---|---|---|---|
| Characteristics | Nematode | Nematode | Nematode | Nematode | Trematode Trematode Class of parasitic flukes consisting of three subclasses, monogenea, aspidogastrea, and digenea. The digenetic trematodes are the only ones found in man. They are endoparasites and require two hosts to complete their life cycle. Schistosoma/Schistosomiasis |
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli | Humans | Dogs | Humans |
|
Humans |
| Transmission | Fecal–oral | Fecal–oral | Fecal–oral | Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions contact with contaminated soil | Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions contact with contaminated water |
| Clinical |
|
|
|
|
|
| Diagnosis |
|
|
Stool analysis |
|
|
| Management |
|
|
|
|
Praziquantel Praziquantel An anthelmintic used in most schistosome and many cestode infestations. Anthelmintic Drugs |
| Prevention | Good hygiene |
|
|
|
|

Low-power microscopic view of Enterobius vermicularis
Image: “Double bulb oesophagus of Enterobius vermicularis, under low power” by Kaniyarakkal V et al. License: CC BY 4.0
An adult Ascaris lumbricoides worm
Image: “An adult Ascaris lumbricoides worm” by CDC Division of Parasitic Diseases. License: Public Domain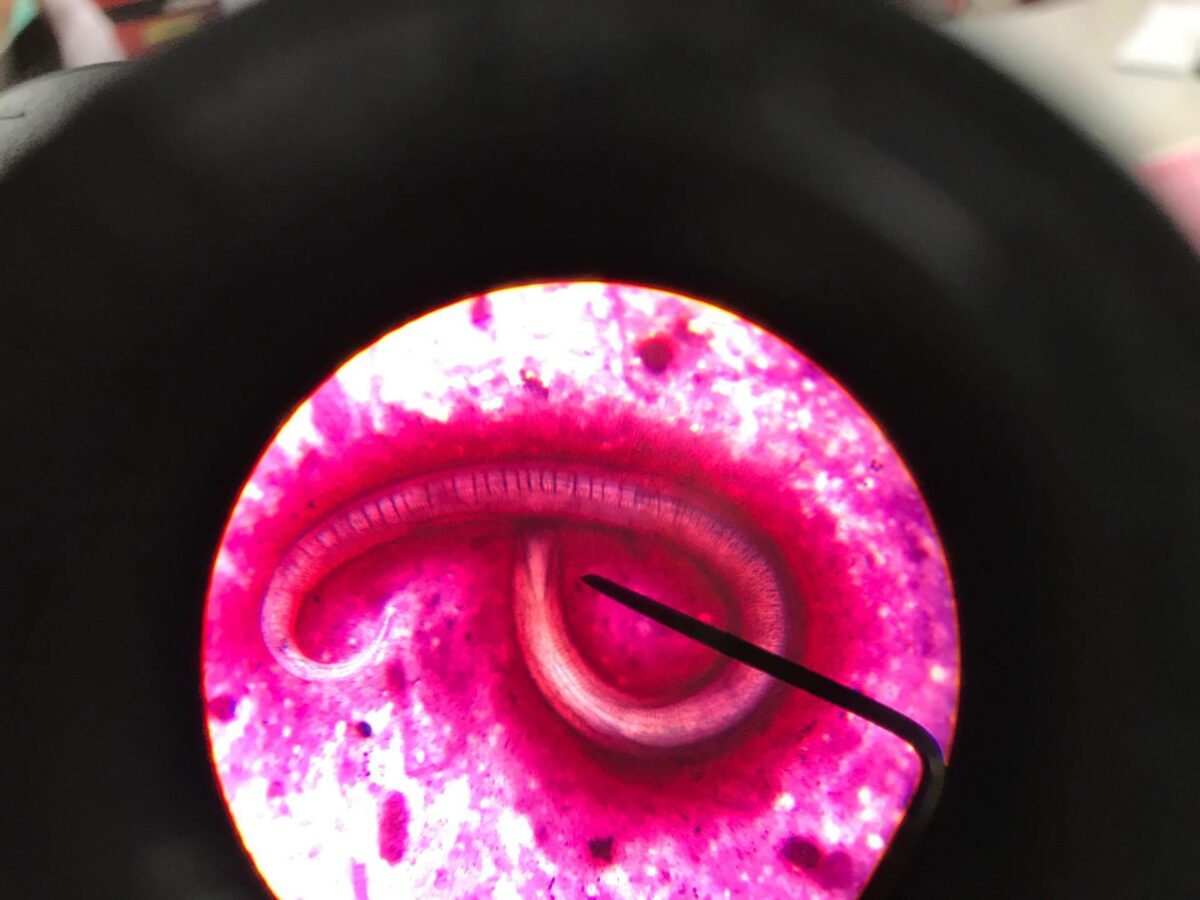
Strongyloides stercoralis parasite
Image: “Strongyloides Stercoralis in sputum” by CDC Division of Parasitic Diseases. License: CC BY 4.0
An adult Schistosoma mansoni seen on electron microscopy
Image: “Schistosoma mansoni, adult. SEM [Scanning electron microscopy] of worm, unstained” by Otis Historical Archives of “National Museum of Health & Medicine”. License: CC BY 2.0