Schistosomiasis is an infection caused by Schistosoma, a trematode. Schistosomiasis often occurs in developing countries with poor sanitation Sanitation The development and establishment of environmental conditions favorable to the health of the public. Hepatitis E Virus. Freshwater snails are the intermediate host infected by schistosomes, which are then transmitted to humans through skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions contact with contaminated fresh water. The clinical presentation occurs as a result of the host’s immune response to antigens from the eggs. Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic, but others may develop acute schistosome dermatitis Dermatitis Any inflammation of the skin. Atopic Dermatitis (Eczema), acute schistosomiasis syndrome, or chronic schistosomiasis. The diagnosis can be made with microscopic evaluation of the urine or feces, serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus, or PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR). The mainstay of treatment for schistosomiasis is the anthelmintic medication praziquantel Praziquantel An anthelmintic used in most schistosome and many cestode infestations. Anthelmintic Drugs.
Last updated: Mar 29, 2023
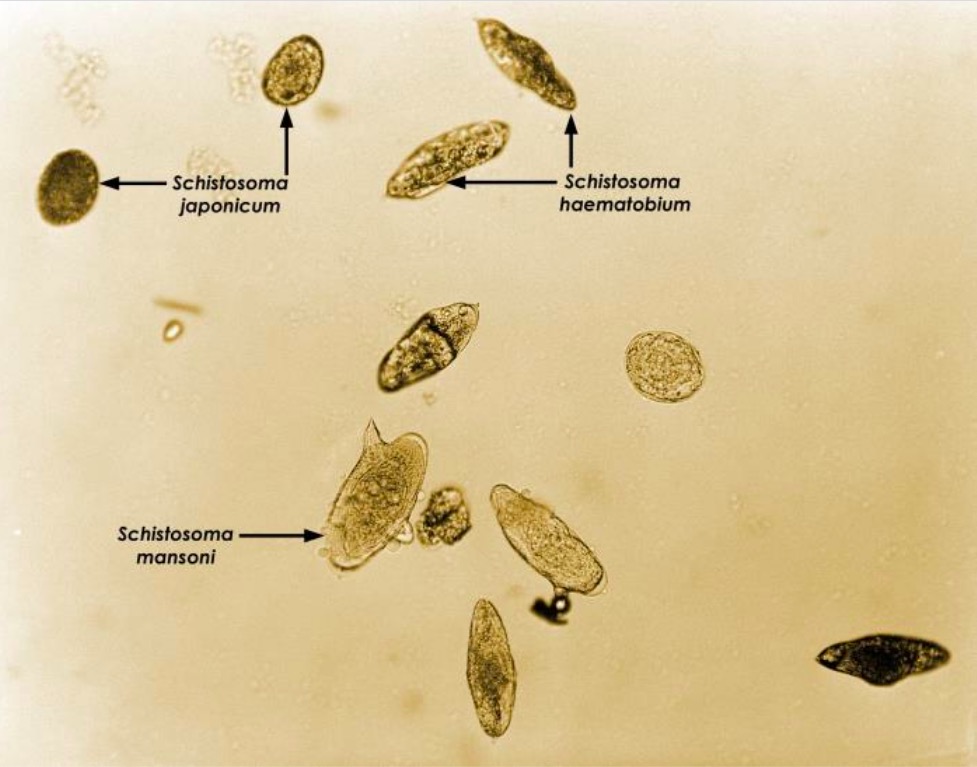
Photomicrograph depicting a grouping of 3 different species of Schistosoma eggs: S. japonicum, S. mansoni, and S. haematobium.
Image: “21017” by CDC/Dr. Brodsky. License: Public DomainTransmission occurs through skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions contact with infected fresh water.
Schistosoma occupies freshwater environments in areas with poor sewerage management.
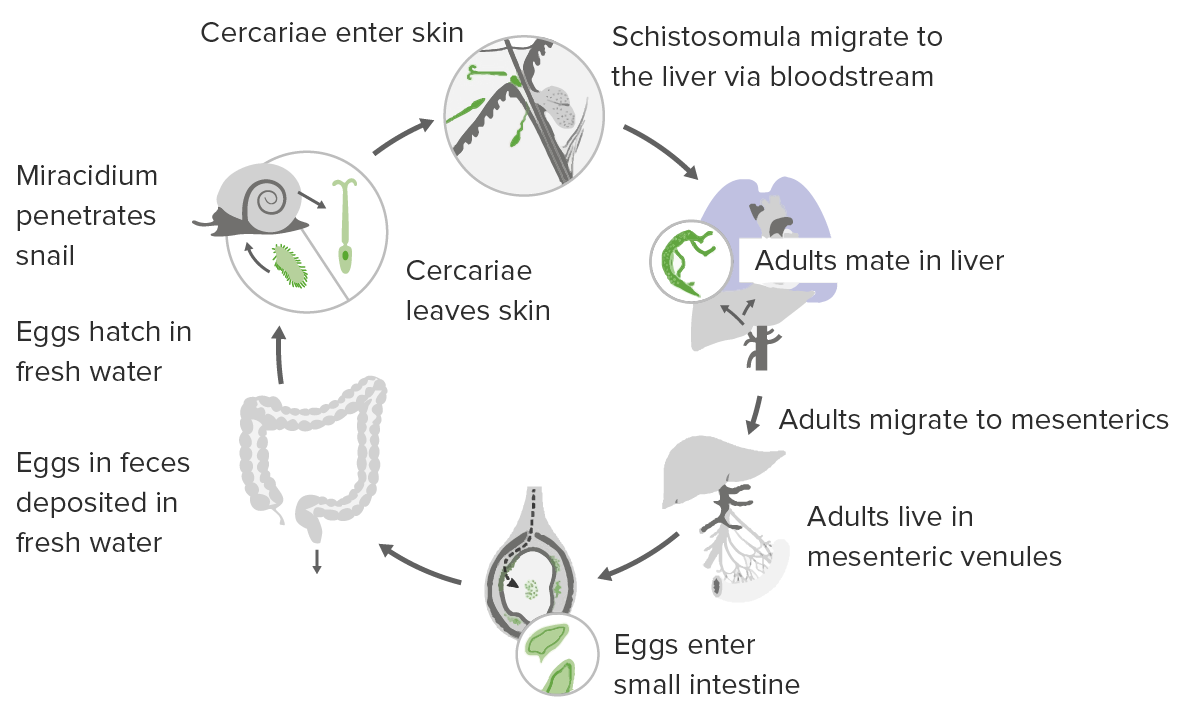
The life cycle of Schistosoma
Image by Lecturio.
Schistosoma mansoni cercaria
Image:“Schistosoma” by CDC/Dr. D.S. Martin. License: Public DomainClinical disease is caused by:
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are asymptomatic. Symptomatic individuals can present in several ways:
Also known as “swimmer’s itch”:

A papular rash due to acute schistosome dermatitis:
The hypersensitivity reaction occurs when skin is penetrated by Schistosoma cercariae.
Occurs due to a systemic hypersensitivity reaction 3–8 weeks after the initial infection:
Presentation can vary depending on the number of eggs in the tissues, the infection site, and the immune response of the host.
Intestinal schistosomiasis:
Hepatosplenic schistosomiasis:
Genitourinary schistosomiasis:
Neuroschistosomiasis:
Personal protection in endemic areas:
Control strategies:
| Organism | Enterobius vermicularis Enterobius Vermicularis Enterobius/Enterobiasis | Toxocara canis Toxocara canis A species of parasitic nematode found in the intestine of dogs. Lesions in the brain, liver, eye, kidney, and lung are caused by migrating larvae. In humans, these larvae do not follow normal patterns and may produce visceral larva migrans (larva migrans, visceral). Toxocariasis | Ascaris Ascaris Ascaris is a genus of parasitic nematodes. The infection, ascariasis, is most often caused by A. lumbricoides. Transmission occurs primarily via ingestion of water or food contaminated with Ascaris eggs. Most patients with ascariasis are asymptomatic. Ascaris/Ascariasis lumbricoides | Strongyloides stercoralis Strongyloides stercoralis A species of parasitic nematode widely distributed in tropical and subtropical countries. The females and their larvae inhabit the mucosa of the intestinal tract, where they cause ulceration and diarrhea. Strongyloidiasis | Schistosoma mansoni |
|---|---|---|---|---|---|
| Characteristics | Nematode Nematode A phylum of unsegmented helminths with fundamental bilateral symmetry and secondary triradiate symmetry of the oral and esophageal structures. Many species are parasites. Toxocariasis | Nematode Nematode A phylum of unsegmented helminths with fundamental bilateral symmetry and secondary triradiate symmetry of the oral and esophageal structures. Many species are parasites. Toxocariasis | Nematode Nematode A phylum of unsegmented helminths with fundamental bilateral symmetry and secondary triradiate symmetry of the oral and esophageal structures. Many species are parasites. Toxocariasis | Nematode Nematode A phylum of unsegmented helminths with fundamental bilateral symmetry and secondary triradiate symmetry of the oral and esophageal structures. Many species are parasites. Toxocariasis | Trematode |
| Reservoir Reservoir Animate or inanimate sources which normally harbor disease-causing organisms and thus serve as potential sources of disease outbreaks. Reservoirs are distinguished from vectors (disease vectors) and carriers, which are agents of disease transmission rather than continuing sources of potential disease outbreaks. Humans may serve both as disease reservoirs and carriers. Escherichia coli | Humans | Dogs | Humans |
|
Humans |
| Transmission | Fecal–oral | Fecal–oral | Fecal–oral | Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions contact with contaminated soil | Skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions contact with contaminated water |
| Clinical |
|
|
|
|
|
| Diagnosis |
|
|
Stool analysis |
|
|
| Management |
|
|
|
|
Praziquantel Praziquantel An anthelmintic used in most schistosome and many cestode infestations. Anthelmintic Drugs |
| Prevention | Good hygiene |
|
|
|
|

Low-power, microscopic view of Enterobius vermicularis
Image:“Double bulb oesophagus of Enterobius vermicularis, under low power” by Kaniyarakkal V et al. License: CC BY 4.0
Adult Ascaris lumbricoides worm
Image:“An adult Ascaris lumbricoides worm” by CDC Division of Parasitic Diseases. License: Public Domain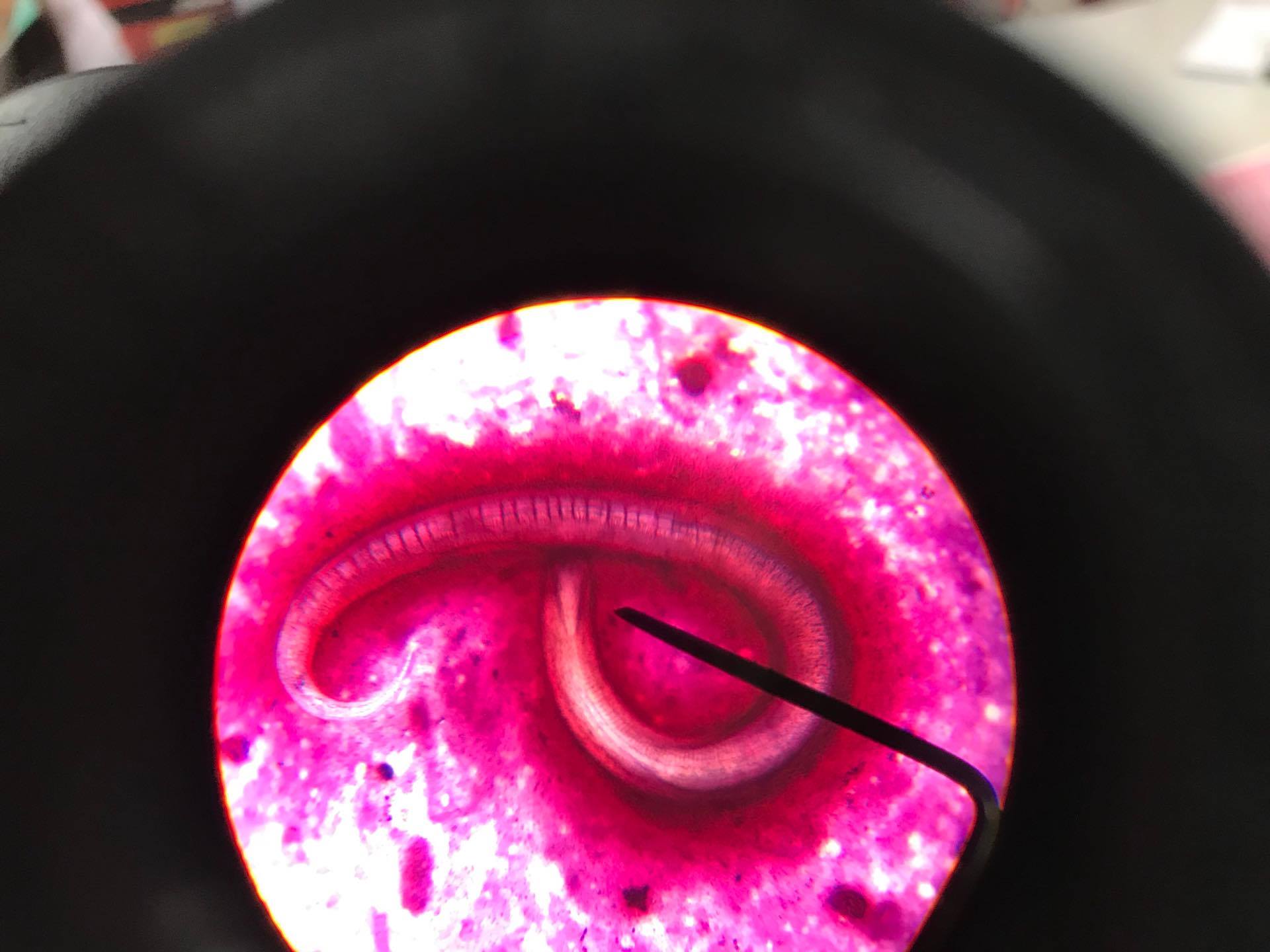
Strongyloides stercoralis parasite
Image:“Strongyloides Stercoralis in sputum” by CDC Division of Parasitic Diseases. License: CC BY 4.0
Adult Schistosoma mansonias seen on electron microscopy
Image: “Schistosoma mansoni, adult. SEM [Scanning electron microscopy] of worm, unstained” by Otis Historical Archives of “National Museum of Health & Medicine”. License: CC BY 2.0